Time limit: 0
Quiz Summary
0 of 37 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 37 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 37
1. Question
A 33-year-old Caucasian male presents to your office and complains that solid food ‘sticks in the chest.’ He says that he has to chew food more carefully, take more liquids with meals, and swallow small portions. He recalls having a similar episode several months ago that got better after ‘following a diet’, but it was much less severe. He has had periodic chest pain behind the sternum for the last several years. He denies any recent significant weight loss, abdominal pain, nausea, vomiting, diarrhea/constipation, black stools and neck lumps. He smokes one pack of cigarettes daily and consumes alcohol occasionally. He is currently not taking any medications. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 2 of 37
2. Question
An 84-year-old man is being treated for advanced pharyngeal cancer with radiation and chemotherapy. He complains of mouth ulcers, pain, and difficulty swallowing. His other medical problems include hypertension, osteoporosis, and Parkinson’s disease. He had a stroke several years ago. His older son lives with him, and helps with his care. The patient weighs 132 pounds (60 kg), and his BMI is 22 kg/m2. His lab values are as follows:
Hemoglobin
9.4 g/dL
Ht
28%
MCV
80fl
Platelet count
250,000/cm3
Leukocyte count
5,000/cm3
Segmented neutrophils
74%
Lymphocytes
20%
Monocytes
6%
Serum Na
138 mEq/L
Serum K
4.0 mEq/L
Chloride
108 mEq/L
Bicarbonate
22 mEq/L
BUN
18 mg/dL
Serum Creatinine
0.8 mg/dL
Calcium
8.6 mg/dL
Blood Glucose
122 mg/dL
Gastrostomy tube is placed for enteral feeding. Which of the following is the most appropriate nutrition goal for this patient?
CorrectIncorrect -
Question 3 of 37
3. Question
A 35-year-old woman comes to the clinic due to severe heartburn that is resistant to over-the-counter antacids. The patient has no known medical problems and takes no other medications. She occasionally has a glass of wine with dinner but does not use tobacco or illicit drugs. Physical examination shows scattered telangiectasias on the face, several ulcers at the tips of the fingers, and small calcium deposits in the soft tissues of the hands and elbows. Which of the following processes is the most likely cause of this patient’s heartburn?
CorrectIncorrect -
Question 4 of 37
4. Question
A 16-year-old male comes to your office for a routine check-up. He was diagnosed with asthma six months ago and started on inhaled corticosteroids as well as an albuterol inhaler as needed. He reports a modest improvement in his symptoms using this regimen. He has no complaints currently. Physical examination reveals white plaques on his buccal mucosa that can be scraped off, leaving hyperemic spots. The lungs are clear on auscultation. Which of the following is the best initial therapy for the oral lesion?
CorrectIncorrect -
Question 5 of 37
5. Question
A 55-year-old man is brought to the emergency department with severe abdominal pain and vomiting for the last 24 hours. The patient’s abdominal pain began abruptly, and he describes it as a stabbing sensation radiating to his back. He then developed malaise, chills, nausea, and several episodes of vomiting. The patient’s medical history includes hypertension, hyperlipidemia, and gout. Medications include chlorthalidone, atorvastatin, and allopurinol. Family history is unremarkable. The patient occasionally uses alcohol and has smoked a half a pack of cigarettes a day for 20 years. He does not use illicit drugs. Temperature is 39.4 C (102.9 F), blood pressure is 105/58 mm Hg, pulse is 110/min, and respirations are 18/min. BMI is 27 kg/m2. Physical examination shows a middle-age man in moderate distress. The patient has scleral icterus, normal jugular venous pressure, clear lung fields, and distinct S1 and S2. The abdomen is soft and tender to palpation over the midepigastrium and right upper quadrant. There is no rebound tenderness, rigidity, hepatomegaly, or splenomegaly. The remainder of the examination is normal. Laboratory test results are as follows:
Complete blood count
Leukocytes
18,000/mm3
Hemoglobin
13.3 g/dL
Hematocrit
40%
Platelets
440,000/mm3
Serum chemistry
Sodium
142 mEq/L
Potassium
3.2 mEq/L
Chloride
102 mEq/L
Bicarbonate
28 mEq/L
Blood urea nitrogen
26 mg/dL
Creatinine
1.2 mg/dL
Calcium
8.8 mg/dL
Glucose
120 mg/dL
Liver function studies
Total protein
8.5 g/dL
Albumin
4.3 g/dL
Total bilirubin
5.3 mg/dL
Direct bilirubin
3.4 mg/dL
Alkaline phosphatase
320 U/L
Aspartate aminotransferase
112 U/L
Alanine aminotransferase
149 U/L
Lipase
1,112 U/L (normal: 0-160)
Abdominal ultrasound demonstrates multiple small gallbladder stones and common bile duct dilation. No stones are visualized in the biliary tree. The pancreas is not well visualized due to gastric shadow. Blood cultures are drawn. The patient is admitted and treated with intravenous fluids and antibiotics. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 6 of 37
6. Question
A 52-year-old man is being evaluated due to upper abdominal discomfort, nausea, and frequent heartburn for the past 6 months. His symptoms are partially relieved with over-the-counter antacids. The patient has had no chest pain, dysphagia, odynophagia, vomiting, black or bloody stools, or weight loss. He has a history of hypertension and mild intermittent asthma. He has a 20-pack-year smoking history but quit 3 years ago. BMI is 32.8 kg/m2. Upper gastrointestinal endoscopy shows moderate esophagitis with velvety, reddish mucosa extending from the gastroesophageal junction into the distal esophagus and mild antral gastritis. Biopsy results are consistent with Barrett esophagus without dysplasia. Antral mucosal biopsies do not show evidence of Helicobacter pylori infection. He is started on proton pump inhibitor therapy. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 7 of 37
7. Question
A 74-year-old man comes to the office due to several months of choking spells, dysphagia, and cough. He has also had recurrent episodes of pneumonia. His other medical problems include hypertension and osteoarthritis. Blood pressure is 130/70 mm Hg. The patient has foul-smelling breath, but his oropharyngeal and neck examinations are normal. Cardiopulmonary examination is also normal. A barium swallow study is performed and reveals an abnormality in the upper esophagus, as shown in the image below.
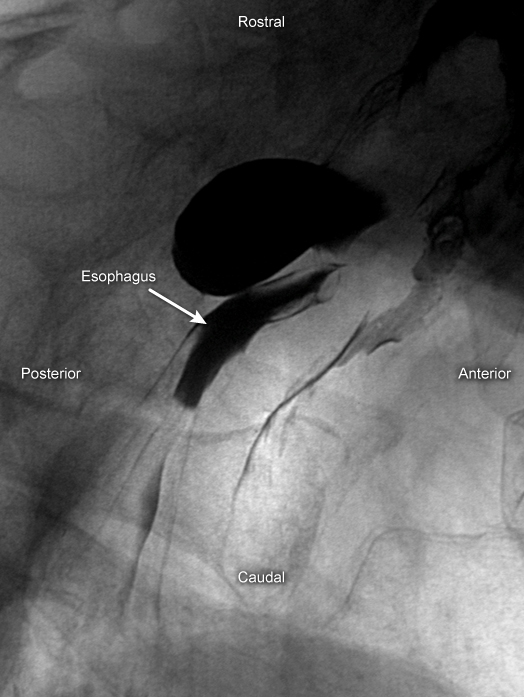
Which of the following mechanisms is the most likely cause of his symptoms?
CorrectIncorrect -
Question 8 of 37
8. Question
A 68-year-old man comes to the emergency department with left lower quadrant abdominal pain. CT scan reveals acute diverticulitis, and oral ciprofloxacin and metronidazole are prescribed. Four days later, the patient returns to the emergency department with persistent abdominal pain associated with chills, nausea, decreased appetite, and malaise. Medical history includes hypertension, hyperlipidemia, and gout. Two benign polyps were removed during a colonoscopy 5 years ago. Temperature is 38.5 C (101.3 F), blood pressure is 130/80 mm Hg, pulse is 112/min, and respirations are 18/min. The abdomen is soft and nondistended, with significant left lower quadrant tenderness and guarding but no rebound. Bowel sounds are decreased. Rectal examination shows left-sided tenderness. Testing of stool for occult blood is negative. Laboratory results are as follows:
Complete blood count
Hemoglobin
13 g/dL
Platelets
400,000/mm3
Leukocytes
16,000/mm3
Serum chemistry
Bicarbonate
24 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Glucose
100 mg/dL
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 9 of 37
9. Question
A 46-year-old woman comes to the physician for diarrhea and occasional fecal incontinence. She has had 3-4 loose stools a day and vague rectal discomfort for the last 2 months. The patient says, “I often feel a painful urge to go but only pass a small amount of mucus.” She has noticed bright red blood mixed with the stool on several occasions. The patient was treated for cervical cancer with surgery and chemoradiation a year ago. She is afebrile. On examination, there is mild tenderness in left lower quadrant but no guarding or rebound. Rectal examination shows guaiac-positive brown stool. Her stool Clostridium difficile toxin polymerase chain reaction testing is negative. Rectosigmoidoscopy shows pale rectal mucosa, several serpiginous telangiectasias, and small areas of mucosal hemorrhage. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 10 of 37
10. Question
A 42-year-old woman with a history of chronic alcoholism comes to the emergency department due to 2 days of severe abdominal pain. She describes the pain as sharp, nonradiating, and located in the center of her abdomen. The patient also reports nausea and several episodes of vomiting. Medical history is significant for type 2 diabetes mellitus and asthma. Medications include metformin, sitagliptin, and inhaled albuterol. For the last 2 years she has drunk 2 or 3 pints of alcohol at a time, several times a week. The patient smokes a pack of cigarettes a day and occasionally uses cocaine. Family history is not significant. Temperature is 36.7 C (98.1 F), blood pressure is 110/60 mm Hg, pulse is 92/min, and respirations are 16/min. Oxygen saturation is 96% on room air. BMI is 27 kg/m2. Physical examination shows dry mucous membranes, normal jugular venous pressure, clear lung fields, and normal S1 and S2. The abdomen is soft and tender in the midepigastric region without hepatosplenomegaly. Bowel sounds are present. There is no rebound tenderness, rigidity, or costovertebral angle tenderness, and no peripheral edema. Neurologic examination is within normal limits. Laboratory results are as follows:
Complete blood count
Leukocytes
9,000/mm3
Hemoglobin
13.1 g/dL
Hematocrit
40%
Mean corpuscular volume
102 μm3
Platelets
180,000/mm3
Serum chemistry
Sodium
133 mEq/L
Potassium
3.1 mEq/L
Chloride
94 mEq/L
Bicarbonate
30 mEq/L
Blood urea nitrogen
24 mg/dL
Creatinine
0.8 mg/dL
Calcium
9.6 mg/dL
Glucose
160 mg/dL
Liver function studies
Total protein
8 g/dL
Albumin
4.3 g/dL
Total bilirubin
0.3 mg/dL
Direct bilirubin
0.1 mg/dL
Alkaline phosphatase
120 U/L
Aspartate aminotransferase
87 U/L
Alanine aminotransferase
49 U/L
Lipase
652 U/L
Fasting lipid panel
Total cholesterol
220 mg/dL
High-density lipoprotein
52 mg/dL
Low-density lipoprotein
110 mg/dL
Triglycerides
300 mg/dL
Abdominal ultrasound reveals no gallstones or pericholecystic fluid collection. The pancreas is not well visualized. Which of the following is the best predictor for the severity of this patient’s disease?
CorrectIncorrect -
Question 11 of 37
11. Question
A 33-year-old woman with a 9-year history of ulcerative colitis comes to the office due to concern about her risk of colon cancer. One of her close family friends died recently from this cancer. The patient wants to “undergo all the tests for colon cancer.” She has no other comorbid conditions and is under the care of a gastroenterologist who has kept her disease well controlled with sulfasalazine. Compared with sporadic colorectal carcinoma, colorectal malignancy arising in this patient would more likely exhibit which of the following features?
CorrectIncorrect -
Question 12 of 37
12. Question
A 37-year-old man comes to the office for a routine preventive visit. He is healthy and asymptomatic and has no significant medical history. The patient has a 5-pack-year smoking history but quit 10 years ago. He drinks 1 or 2 beers daily. The patient works as a sales manager for a manufacturing company. His father had colon cancer that was diagnosed at age 53, but there is no other family history of cancer. Vital signs are within normal limits. No abnormalities are noted on examination. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 13 of 37
13. Question
A 65-year-old man comes to the office with dysphagia. For the last 3 months, he has relied on protein shakes and juices for nourishment as he has had difficulty swallowing solid foods. He has also had a diminished appetite and an estimated weight loss of 9.1 kg (20 lb). Medical history includes hyperlipidemia, emphysema, and previous episodes of pancreatitis. Family history includes lung cancer in his mother. The patient smoked a pack of cigarettes daily for 50 years but quit 2 years ago. He has been drinking a fifth (750 mL) of vodka weekly for the last decade. Vital signs are normal. BMI is 19.2 kg/m2. Temporal wasting is present but physical examination is otherwise unremarkable. Upper endoscopy reveals a 4-cm mass in the middle third of the esophagus, and several biopsies are taken. Thoracic imaging reveals mediastinal lymphadenopathy. Histologic evaluation of the biopsy specimens will most likely show which of the following in this patient?
CorrectIncorrect -
Question 14 of 37
14. Question
A 40-year-old woman comes to the office to discuss nutrition. She says, “I have been overweight since the birth of my third child 10 years ago, and none of the diets I have tried ever seem to help.” The patient reduced her food intake by 100-200 kcal/day on a restricted-fat diet 4 weeks ago, but her weight has not changed. She says, “I want to make sure I am doing the right thing. I tried to read about diets on the internet but I don’t know what to believe.” Medical history is notable for hypothyroidism, treated with a stable dose of levothyroxine. She does not smoke and drinks alcohol on social occasions only. Family history is significant for breast cancer and coronary artery disease in her mother and colon cancer in her father. Vital signs are normal. BMI is 32 kg/m2. The thyroid is normal to palpation. Cardiopulmonary examination is normal. The abdomen is soft and nontender with no hepatomegaly. Deep tendon reflexes are normal and symmetric. Serum TSH is 2.1 µU/mL. Which of the following is the most appropriate nutritional recommendation for this patient?
CorrectIncorrect -
Question 15 of 37
15. Question
A 26-year-old woman comes to the emergency department due to diarrhea. For the last 2 days, she has had abrupt-onset diarrhea associated with crampy lower abdominal pain and fatigue. The patient is experiencing 4-6 watery bowel movements daily with visible blood throughout the stool. She has otherwise been well with no ill contacts and has not recently traveled internationally. Temperature is 37.5 C (99.5 F), blood pressure is 110/76 mm Hg, and pulse is 90/min. Abdominal examination shows normal bowel sounds with mild diffuse tenderness and no peritoneal signs. Laboratory results are as follows:
Serum chemistry
Sodium
136 mEq/L
Potassium
3.8 mEq/L
Chloride
97 mEq/L
Blood urea nitrogen
18 mg/dL
Creatinine
0.9 mg/dL
Glucose
74 mg/dL
Complete blood count
Hemoglobin
12.2 g/dL
Leukocytes
11,900/mm3
Platelets
350,000/mm3
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 16 of 37
16. Question
A 55-year-old man comes to the office to follow up on cirrhosis secondary to nonalcoholic fatty liver disease, which was diagnosed after a liver biopsy a year ago. The patient has had no abdominal pain, abdominal swelling, hematemesis, or melena. He does not use tobacco or alcohol. Vital signs are normal. BMI is 34 kg/m2. On examination, the heart and lungs are normal to auscultation. The abdomen is soft, nondistended, and without organomegaly or masses. The patient has received hepatitis A and B vaccinations. A year ago, upper gastrointestinal endoscopy revealed no varices. Laboratory results obtained today are stable compared to previous results and are as follows:
Alanine aminotransferase (SGPT)
96 IU/L
Aspartate aminotransferase (SGOT)
89 IU/L
Total bilirubin
1.2 mg/dL
Alkaline phosphatase
70 IU/L
Creatinine
1.0 mg/dL
Hemoglobin
12.1 g/dL
White blood cells
8,700/mm3
Platelets
140,000/mm3
Which of the following is the most appropriate management of this patient?
CorrectIncorrect -
Question 17 of 37
17. Question
A 22-year-old man comes to the office due to swallowing difficulties. For the past 2 years, he has had episodic, burning, retrosternal pain with eating. In the past month, the patient has also had the sensation that solid food “gets stuck halfway down” after he swallows. He has taken over-the-counter omeprazole without relief. Medical history is notable for seasonal allergies. The patient also has migraines, for which he takes sumatriptan and ibuprofen. On abdominal examination, bowel sounds are normal and no focal tenderness is present. The endoscopic appearance of the midesophagus is shown in the exhibit. Which of the following is the most appropriate next step in management of this patient?
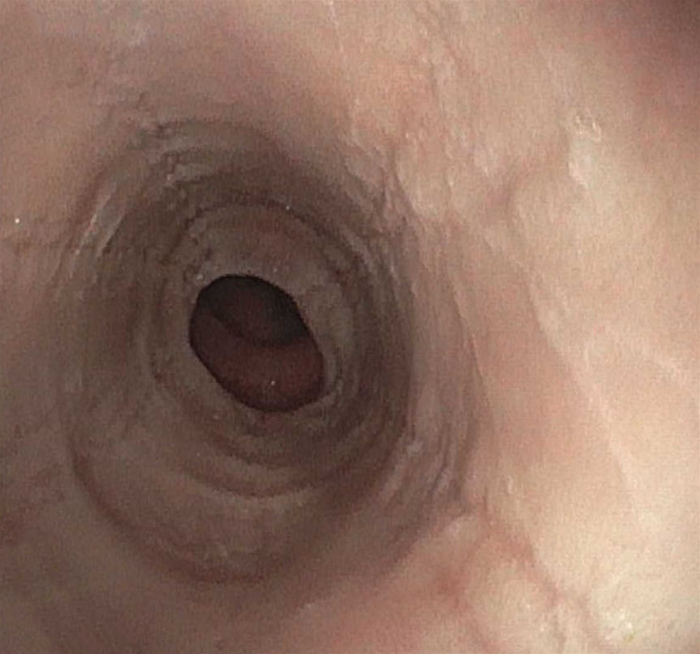 CorrectIncorrect
CorrectIncorrect -
Question 18 of 37
18. Question
A 64-year-old man comes to the emergency department due to diarrhea and intermittent abdominal cramps for the past 6 weeks. The patient has had 4 or 5 bowel movements every day over this period, and the stools contain blood and mucus. He also reports poor appetite and fatigue and has lost 5.9 kg (13 lb). The patient has intermittent right knee swelling and tenderness that responds to ibuprofen. He has taken no antibiotics recently and has no other medical conditions. The patient was last seen by a physician 2 years ago; his last colonoscopy 4 years ago was normal. Family history is positive for colon cancer in his mother. Temperature is 38.1 C (100.6 F), blood pressure is 142/84 mm Hg, pulse is 98/min, and respirations are 16/min. Physical examination shows tenderness in the left lower quadrant without rebound or guarding. Digital rectal examination is positive for blood. Laboratory results are as follows:
Leukocytes
13,600 mm3
Hemoglobin
9.6 g/dL
Platelets
314,000/mm3
Erythrocyte sedimentation rate
65 mm/hr
Flexible sigmoidoscopy reveals erythematous, friable mucosa of the entire rectum and the majority of the sigmoid colon. Small, shallow ulcers are also seen. Which of the following is the most likely cause of this patient’s current condition?
CorrectIncorrect -
Question 19 of 37
19. Question
A 79-year-old woman is brought to the emergency department by her daughter due to bloody stools. The patient has a 3-day history of occasionally passing blood with her stools but this morning she filled up the toilet bowl with bloody stools. She has not had another bowel movement since. She does not have any associated symptoms such as nausea, vomiting, or abdominal pain. Her past medical history includes mild dementia, hypertension, diet-controlled diabetes mellitus, and osteoarthritis. She does not smoke or drink alcohol. The patient takes a baby aspirin daily and nonsteroidal anti-inflammatory agents occasionally for hip pain. Her temperature is 36.7 C (98 F), heart rate is 89/min, blood pressure is 146/82 mm Hg, and respiratory rate is 16/min. She appears pale. Abdominal examination is unremarkable. Rectal examination reveals bright red blood in the rectal vault, without tenderness. Nasogastric aspirate shows copious amounts of bilious fluid. Laboratory results are as follows:
Complete blood count
Hematocrit
28%
Platelets
200,000/mm3
Serum chemistry
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Coagulation studies
International Normalized Ratio (INR)
0.8
She is started on intravenous fluids and blood work is ordered including blood type and cross-match. Which of the following is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 20 of 37
20. Question
A 45-year-old woman comes to the office for progressive itchiness and fatigue. She also notes yellowing of the eyes and skin. Physical examination shows scleral icterus, multiple excoriations on both the upper and the lower extremities, and hepatomegaly. Laboratory results are as follows:
Liver function studies
Total bilirubin
5.3 mg/dL
Alkaline phosphatase
982 U/L
Aspartate aminotransferase (SGOT)
89 U/L
Alanine aminotransferase (SGPT)
67 U/L
Gamma-glutamyl transpeptidase
450 U/L (normal: 10-60 U/L)
Liver biopsy reveals dense lymphocytic infiltration of the portal triads, as well as granulomatous destruction of interlobular bile ducts. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 21 of 37
21. Question
A 70-year-old woman comes to the emergency department due to abdominal pain and bloody diarrhea. Last night, the patient experienced mild cramping with abdominal pain and an urgent desire to defecate, but when she went to the bathroom, she did not have a bowel movement. The patient attributed her symptoms to the spicy food she had for lunch and took some antacids, but the pain persisted. This morning she had large-volume diarrhea containing bright red blood. She has had no nausea or vomiting and has never had similar symptoms. The patient was found to have diverticulosis during a colonoscopy 2 years ago, so a high-fiber diet was advised. Other medical problems include hypertension, type 2 diabetes mellitus, coronary artery disease, and end-stage renal disease from diabetic nephropathy. She receives intermittent maintenance hemodialysis (most recently yesterday) and has had several occasions of hypotension during dialysis, requiring intravenous fluid replacement. The patient does not use tobacco, alcohol, or illicit drugs. She has taken no antibiotics or nonsteroidal analgesics recently. The patient lives with her husband and has not recently traveled. Temperature is 37.2 C (99 F), blood pressure is 119/81 mm Hg, pulse is 90/min, and respirations are 16/min. The abdomen is mildly distended and soft with moderate left-sided tenderness. There is no rebound tenderness and bowel sounds are decreased. Rectal examination reveals bloody stool but no tenderness or mass. Laboratory results are as follows:
Complete blood count
Leukocytes
14,500/mm3
Hemoglobin
10.4 g/dL
Platelets
220,000/mm3
Serum chemistry
Sodium
135 mEq/L
Potassium
4.6 mEq/L
Chloride
102 mEq/L
Bicarbonate
18 mEq/L
Glucose
120 mg/dL
Serum amylase
231 U/L
INR
1.0
Activated PTT
32 sec
Upright abdominal radiography reveals a dilated transverse colon with no free air. Flexible sigmoidoscopy shows mucosal edema. Which of the following is the most likely cause of this patient’s current symptoms?
CorrectIncorrect -
Question 22 of 37
22. Question
A 45-year-old man comes to the clinic for follow-up 8 weeks after an episode of acute pancreatitis due to alcohol abuse. The patient initially presented with abdominal pain radiating to his back, nausea, and vomiting. His condition improved with supportive care, and the hospital course was uncomplicated. Since discharge, he reports occasional mild abdominal discomfort but otherwise feels well. His abdominal discomfort is not associated with food. He has no vomiting, diarrhea, or early satiety. The patient has stopped drinking since his last admission, but continues to smoke a pack of cigarettes a day and has done so for the last 30 years. Temperature is 36.7 C (98.2 F), blood pressure is 125/70 mm Hg, pulse is 72/min, and respirations are 16/min. On physical examination, oropharynx is without lesions, lungs are clear, and there are normal S1 and S2 without murmurs. Abdominal examination reveals fullness and mild tenderness over the epigastric area. Bowel sounds are present. There is no hepatomegaly, splenomegaly, guarding, or rebound tenderness. The remainder of the examination is normal. Laboratory results are as follows:
Complete blood count
Leukocytes
4,100/mm3
Hemoglobin
13.2 g/dL
Mean corpuscular volume
104 µm3
Platelets
180,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
4.4 mEq/L
Chloride
98 mEq/L
Bicarbonate
26 mEq/L
Blood urea nitrogen
8 mg/dL
Creatinine
0.8 mg/dL
Liver function studies
Total protein
7.5 g/dL
Albumin
3.7 g/dL
Total bilirubin
0.3 mg/dL
Alkaline phosphatase
70 U/L
Aspartate aminotransferase (SGOT)
37 U/L
Alanine aminotransferase (SGPT)
24 U/L
Lipase
254 U/L (normal: 0-160)
Which of the following is the most likely cause of this patient’s persistent abdominal pain?
CorrectIncorrect -
Question 23 of 37
23. Question
A 25-year-old man comes to the office for follow-up. The patient was diagnosed with Graves disease 12 months ago during an evaluation for diarrhea, tremor, and palpitations. He received radioiodine therapy and required initiation of levothyroxine due to iatrogenic hypothyroidism. The patient reports that most of his symptoms have improved with treatment, but he still has occasional diarrhea and fatigue. In addition, his serum TSH levels have remained elevated despite escalating dosages of levothyroxine. The patient takes no other medications and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 130/90 mm Hg and pulse is 64/min. The thyroid is not palpable and skin is mildly dry; otherwise, physical examination is unremarkable. Laboratory results are as follows:
Hemoglobin
10 g/dL
Mean corpuscular volume
74 µm3
Serum creatinine
0.8 mg/dL
Serum glucose
80 mg/dL
TSH
11 µU/mL
Free thyroxine
0.8 ng/dL
Stool occult blood test is negative. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 24 of 37
24. Question
A 33-year-old woman comes to the office due to fatigue over the last 6 months. She attributes this to her stressful work environment but still wants to be “checked up.” The patient has no significant medical history, and her only medication is an oral contraceptive. She has had no abdominal pain, back pain, vomiting, diarrhea, or leg swelling. The patient drinks 1 or 2 glasses of wine on most days of the week but does not use tobacco or illicit drugs. Vital signs are normal. Today, her weight is 64 kg (141 lbs), and the patient reports she weighed 68 kg (150 lbs) 3 months ago. The liver edge is palpable 2 cm below the right costal margin. Laboratory results are as follows:
Complete blood count
Hemoglobin
12.6 g/dL
Platelets
320,000/mm3
Leukocytes
9,000/mm3
Serum chemistry
Sodium
140 mEq/L
Potassium
4.8 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Calcium
10.6 mg/dL
Liver function studies
Albumin
4.1 g/dL
Total bilirubin
0.9 mg/dL
Alkaline phosphatase
370 U/L
Aspartate aminotransferase (SGOT)
42 U/L
Alanine aminotransferase (SGPT)
37 U/L
Gamma-glutamyl transpeptidase
168 U/L (0-30 U/L)
Amylase
45 U/L
Abdominal ultrasound confirms mild hepatomegaly; the pancreas is not well visualized. Chest x-ray reveals bilateral hilar fullness but no parenchymal opacities. Which of the following is the most likely cause of the abnormal liver function studies in this patient?
CorrectIncorrect -
Question 25 of 37
25. Question
A 65-year-old woman comes to the emergency department due to the sudden onset of severe periumbilical pain, nausea, and vomiting. She has no fever, diarrhea, constipation, or urinary complaints. Her last menstrual period was 14 years ago. The patient has a history of coronary artery disease, a recent acute anterior myocardial infarction, hypertension, and hyperlipidemia. She had an appendectomy at age 18. She has a 20-pack-year smoking history. The patient drinks alcohol occasionally. Her temperature is 36.7 C (98 F), blood pressure is 120/76 mm Hg, pulse is 120/min and irregular, and respirations are 16/min. The abdomen is soft, nondistended, nontender, and has normoactive bowel sounds. There is no rebound tenderness or rigidity. Pelvic examination is within normal limits. ECG shows atrial fibrillation without other abnormal findings. Laboratory results are as follows:
White blood cells 14,000/mm3 Sodium 140 mEq/L Potassium 4.9 mEq/L Blood urea nitrogen 20 mg/dL Creatinine 0.7 mg/dL Glucose 110 mg/dL The other studies show normal serum lipase, slightly elevated serum amylase, and normal liver function tests. Urinalysis is normal. Fecal occult blood test is negative. Plain abdominal x-ray shows no abnormalities. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 26 of 37
26. Question
A 54-year-old man comes to the office due to a recent finding of abnormal liver function tests. Four weeks ago, he went to the emergency department due to 2 days of diarrhea and vomiting. During the evaluation for viral gastroenteritis, the patient was found to have elevated liver aminotransferase levels and was advised to follow up with his primary care physician. Since then, his gastrointestinal symptoms have improved. He has had no fever, abdominal pain, nausea, vomiting, jaundice, or pruritus. The patient has no chronic medical problems. He had an appendectomy during childhood with some operative complications requiring blood transfusions. His only medication is ibuprofen as needed. The patient does not use tobacco or illicit drugs and drinks alcohol occasionally. He is married and in a monogamous relationship. Temperature is 37 C (98.6 F), blood pressure is 130/80 mm Hg, and pulse is 78/min. He has no scleral icterus, and mucous membranes are pink and moist. Cardiopulmonary examination is unremarkable. The abdomen is soft and nontender with no organomegaly. Current laboratory results are as follows:
Liver function studies
Total bilirubin
0.8 mg/dL
Alkaline phosphatase
50 U/L
Aspartate aminotransferase
94 U/L
Alanine aminotransferase
112 U/L
Hepatitis panel
Hepatitis A antibody, IgG/IgM
negative
Hepatitis B surface antibody
positive
Hepatitis B surface antigen
negative
Anti-hepatitis C virus antibody
positive
Hepatitis C virus RNA
1,779,877 IU/mL
HIV antibody
negative
The laboratory results are discussed with the patient, and a plan for treatment with direct-acting antivirals is made. The patient agrees to abstinence from alcohol as well as regular follow-up. Which of the following additional interventions is most appropriate in this patient?
CorrectIncorrect -
Question 27 of 37
27. Question
A 52-year-old woman comes to the office due to constipation. The patient has had hard, pebbly stools 2 or 3 times a week for the past month. Previously, she had soft stools 4-5 times a week. She has taken fiber supplements and increased her water intake to sufficient levels without relief. She has no nausea, changes in weight, or hematochezia. Medications include hydrochlorothiazide for hypertension and amitriptyline for insomnia, both of which were started recently due to temporary work-related stress. Colonoscopy from 2 years ago is normal. Temperature is 36.7 C (98.1 F), blood pressure is 128/79 mm Hg, and pulse is 68/min. The abdomen is soft, nontender, and nondistended; there are no masses or organomegaly. Rectal examination reveals no stool impaction. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 28 of 37
28. Question
A 32-year-old woman comes to the office due to abnormal liver imaging. The patient went to the emergency department a week ago for severe right flank pain radiating to the groin. A CT scan revealed a small ureter calculus, which she passed spontaneously the following day. The scan also found a solitary liver lesion, and the patient was advised to follow up with her primary care physician. She reports no right upper quadrant pain, nausea, jaundice, or clay-colored stool. She has no chronic medical problems and has no history of surgery or blood product transfusions. There is no history of cancer or liver disease in her family. She has taken combined oral contraceptives for the past 8 years. The patient does not use tobacco, alcohol, or illicit drugs. She works in a bank, is in a monogamous relationship with her husband, and recently traveled to Europe for her honeymoon. Vital signs are within normal limits. There is no scleral icterus, mucosal lesions, lymphadenopathy, or skin rash. Cardiopulmonary examination shows no abnormalities. Bowel sounds are active in all quadrants. The abdomen is nondistended, soft, and nontender. Liver is not enlarged, and spleen is not palpable. Laboratory results are as follows:
Complete blood count
Hemoglobin
13.2 g/dL
Platelets
380,000/mm³
Leukocytes
8,200/mm³
Liver function studies
Albumin
4.3 g/dL
Total bilirubin
0.7 mg/dL
Alkaline phosphatase
70 U/L
Aspartate aminotransferase (SGOT)
33 U/L
Alanine aminotransferase (SGPT)
24 U/L
A CT scan of the abdomen reveals a 3-cm, well-demarcated lesion in the right lobe of the liver that shows peripheral enhancement with intravenous contrast administration. There are no areas of hemorrhage, necrosis, or scarring. The remainder of the liver is normal. Which of the following is the most appropriate response to this patient regarding her liver lesion?
CorrectIncorrect -
Question 29 of 37
29. Question
A 25-year-old man comes to the emergency department due to food impaction. He was eating a steak when he felt a piece of meat lodge in the retrosternal esophagus. For the past 12 hours, the patient has unsuccessfully attempted to clear the impaction by drinking water and self-inducing vomiting. He has no prior history of dysphagia but has had frequent heartburn for several years that did not improve with twice-daily lansoprazole therapy. Medical history includes asthma, for which he takes as-needed inhaled bronchodilators. Vital signs are normal. Cardiopulmonary and abdominal examinations are unremarkable. Skin examination shows lichenification and excoriations at the anterior elbows bilaterally. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 30 of 37
30. Question
A 52-year-old woman is hospitalized because of shortness of breath on exertion, abdominal distention, and a 25-pound weight loss in the past three months. The symptoms have been progressively getting worse over the past four weeks. Her other medical problems include chronic obstructive pulmonary disease, coronary artery disease, cholelithiasis, and hepatitis-C. She has smoked two packs of cigarettes daily for 30 years. She has drunk four to six 12-ounce beers daily for >20 years. Her mother has a history of breast cancer. Her vital signs are within normal limits. Physical examination is unremarkable except for the presence of massive ascites on abdominal examination. Diagnostic paracentesis and serum chemistries reveal:
Liver function tests
Total bilirubin
1.0 mg/dL
Direct bilirubin
0.8 mg/dL
Alkaline phosphatase
120 U/L
Aspartate aminotransferase
78 U/L
Alanine aminotransferase
55 U/L
Amylase
55 U/L
Lipase
123 U/L
Total protein
5.6 g/dL
Serum albumin
2.8 g/dL
Ascitic fluid
White cell count
150 cells/cmm
Albumin
2.2 g/dL
Amylase
48 U/L
Glucose
32 mg/dL
Which of the following is the most likely cause of the ascites?
CorrectIncorrect -
Question 31 of 37
31. Question
A 55-year-old man comes to the emergency department after an episode of hematemesis. The patient has a history of alcohol-associated cirrhosis. He stopped drinking alcohol when he received the diagnosis 2 years ago. Physical examination shows ascites and dilated abdominal wall vessels. Hemoglobin is 9.6 g/dL. Intravenous octreotide and proton pump inhibitor therapy is initiated. Urgent upper gastrointestinal endoscopy reveals esophageal varices with stigmas of recent bleeding, which are endoscopically treated. The patient is hospitalized for observation and further management. This patient is at greatest risk for which of the following complications during this hospitalization?
CorrectIncorrect -
Question 32 of 37
32. Question
A 17-year-old girl is brought to the office due to yellow eyes for the past day. The patient has no other symptoms, including fever, rash, abdominal pain, vomiting, or diarrhea. She has been preparing for her high school exit examination and has been quite stressed. Temperature is 37.1 C (98.8 F), blood pressure is 110/78 mm Hg, pulse is 80/min, and respirations are 14/min. Mild scleral icterus is present. The abdomen is soft with no hepatosplenomegaly. Serum laboratory results are as follows:
Hemoglobin
13.1 g/dL
Bilirubin, total
3.3 mg/dL
Bilirubin, direct
0.3 mg/dL
Aspartate aminotransferase (SGOT)
22 U/L
Alanine aminotransferase (SGPT)
21 U/L
Two weeks after her examination, the patient’s symptoms resolve. Repeat testing shows a total bilirubin concentration of 1.5 mg/dL. Which of the following changes most likely contributed to this patient’s hyperbilirubinemia?
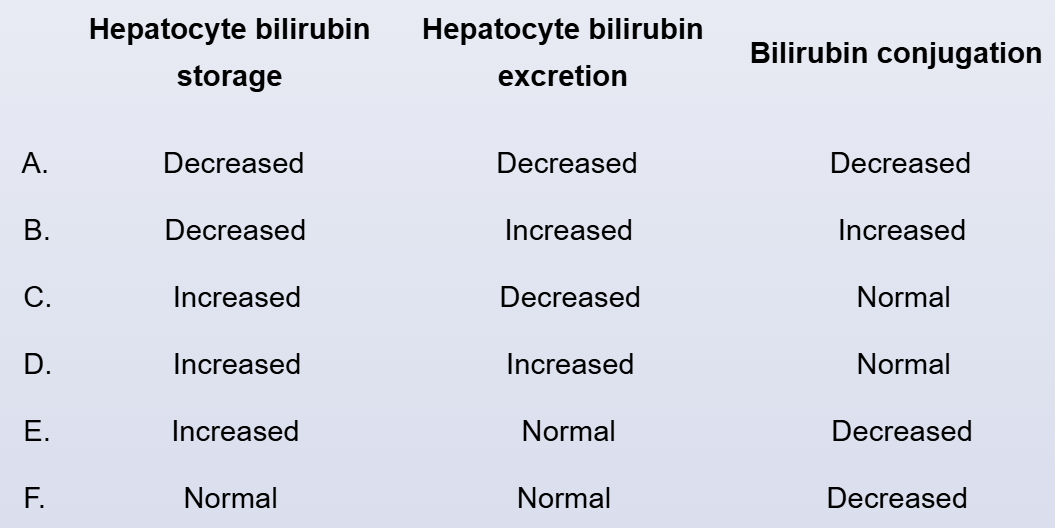 CorrectIncorrect
CorrectIncorrect -
Question 33 of 37
33. Question
A 63-year-old man comes to the emergency department due to easy fatigability and mild abdominal discomfort over the past several days. He also has had intermittent episodes of black-colored stool but has had no chest pain, palpitations, or syncope. His medical history is significant for hypertension, hyperlipidemia, and osteoarthritis. The patient takes amlodipine, lisinopril, and simvastatin. He also takes over-the-counter ibuprofen for hip and back pain that has been “acting up” over the past few weeks. The patient does not use tobacco or illicit drugs and drinks alcohol occasionally. Temperature is 37 C (98.6 F), blood pressure is 106/64 mm Hg supine and 100/72 mm Hg after 3 minutes of standing, and pulse is 98/min. The patient appears pale but is otherwise in no distress. Lung auscultation is normal. Cardiac examination is unremarkable. The abdomen is soft and nondistended with mild epigastric tenderness and hyperactive bowel sounds. Rectal examination shows occult blood-positive melenic stool. Laboratory results are as follows:
Complete blood count
Hemoglobin
7.6 g/dL
Platelets
90,000/mm3
Leukocytes
11,000/mm3
Serum chemistry
Blood urea nitrogen
38 mg/dL
Creatinine
1 mg/dL
Adequate venous access is established, and intravenous crystalloids and pantoprazole are started. Preparation for upper gastrointestinal endoscopy is made. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 34 of 37
34. Question
A 48-year-old man comes to the emergency department due to 3 days of progressively worsening retrosternal burning chest pain, dysphagia, and odynophagia. His medical problems include hypertension and end-stage renal disease. He underwent cadaveric renal allograft transplantation 8 months ago. The patient’s temperature is 38.3 C (101 F), blood pressure is 130/80 mm Hg, and pulse is 94/min. His BMI is 31 kg/m2. The oral mucosa is pink and moist without ulcerations. Cardiopulmonary examination is normal. The abdomen is soft with mild epigastric tenderness. The patient’s leukocyte count is 4,200/mm3. An esophagogastroduodenoscopy demonstrates linear, shallow ulcerations in the lower esophagus. Which of the following is most likely to be seen on esophageal biopsy?
CorrectIncorrect -
Question 35 of 37
35. Question
The following vignette applies to the next 3 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 51-year-old woman comes to the office due to 1 month of worsening diarrhea. The patient has had 5 or 6 watery stools every day with mild abdominal cramping. She has not had blood or mucus in the stool and has been awakened by the diarrhea on several occasions. The patient has had no nausea, vomiting, anorexia, weight loss, dietary changes, or recent travels. She has also had frequent episodes of flushing of her face and neck lasting several minutes, which she attributes to menopause. The patient has no chronic medical conditions and takes no medications. Screening colonoscopy at age 50 was normal. Vital signs are within normal limits. Physical examination shows a soft and nontender abdomen without organomegaly. Rectal examination is normal with negative testing for stool occult blood. Complete blood count and serum chemistry studies are within normal limits.
Item 1 of 3
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 36 of 37
36. Question
Item 2 of 3
Urinary 5-hydroxyindoleacetic acid level is elevated. Which of the following echocardiographic findings would be most suggestive of cardiac involvement by the disease process?
CorrectIncorrect -
Question 37 of 37
37. Question
Item 3 of 3
Echocardiography reveals a normal-appearing tricuspid valve without stenosis or regurgitation. CT scan of the abdomen demonstrates several liver lesions with a nonobstructive jejunal mass. Biopsy confirms a neuroendocrine tumor. Which of the following is the best initial treatment for this patient’s condition?
CorrectIncorrect
