Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 39-year-old woman, gravida 7 para 7, is evaluated for increased vaginal bleeding. Twenty minutes ago, the patient underwent a vacuum-assisted vaginal delivery for fetal heart rate abnormalities of a 4.1-kg (9-lb) infant over an intact perineum. The placenta delivered spontaneously and was intact on inspection. Estimated blood loss for the delivery was 425 mL. This pregnancy was complicated by gestational hypertension for which the patient underwent induction of labor. Her 6 previous pregnancies were uncomplicated. The patient has no chronic medical problems and has had no surgeries. She takes a prenatal vitamin daily. She does not use tobacco, alcohol, or illicit drugs. The patient is now experiencing heavy vaginal bleeding with large blood clots. Blood pressure is 140/80 mm Hg, pulse is 106/min, and respirations are 20/min. On abdominal examination, the uterine fundus is soft and palpated 3 cm above the umbilicus. The perineal pad is saturated with blood, and there are fist-sized blood clots extruding from the vagina. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
A 34-year-old woman, gravida 1 para 0, comes to the office at 35 weeks gestation for a routine prenatal visit. The patient reports good fetal movement and has no contractions or leakage of fluid. She has type 2 diabetes mellitus that has been managed with insulin since the first trimester due to poor glycemic control. This pregnancy has also been complicated by fetal growth restriction diagnosed at 28 weeks gestation when fundal height was lagging. An ultrasound revealed an estimated fetal weight at the 3rd percentile for gestational age. Since then, the patient has been followed with weekly ultrasounds. Today on examination, blood pressure is 130/80 mm Hg and pulse is 92/min. BMI is 34 kg/m2. Fundal height is 31 cm. Ultrasound shows a fetus in vertex presentation with oligohydramnios. Doppler studies of the umbilical artery show new-onset reversed end-diastolic flow. A nonstress test shows moderate variability with no accelerations. A 2-hour postprandial blood glucose level is 155 mg/dL. A group B Streptococcus rectovaginal culture has not yet been collected. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
A 29-year-old woman, gravida 1 para 0, comes to the emergency department at 33 weeks gestation with contractions. The patient was previously seen in the emergency department 5 days ago for preterm contractions. At that time, the tocometer showed contractions every 5 minutes. The cervix was found to be closed, long, and posterior, and transvaginal ultrasound revealed a cervical length of 4 cm. Nucleic acid amplification testing of the cervix for Neisseria gonorrhea and Chlamydia trachomatis, rectovaginal culture for group B Streptococcus, and a urine culture were all negative. After several hours, the contractions subsided, the cervix remained closed, and the patient was discharged home. Today, the patient has had contractions of increasing intensity every 3 minutes but no vaginal bleeding or rupture of membranes. She has no medical conditions or previous surgeries. Temperature is 36.7 C (98 F), blood pressure is 110/70 mm Hg, and pulse is 88/min. Fetal heart rate monitoring shows no abnormalities. Tocometer shows contractions every 3 minutes. The cervix is 5 cm dilated on pelvic examination. A bedside ultrasound confirms a vertex presentation. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
The following vignette applies to the next 2 items.
A 31-year-old woman, gravida 1 para 0, at 28 weeks gestation comes to the office for a routine prenatal visit. The patient has had good fetal movement. She has no abdominal pain or vaginal bleeding but reports a thin, malodorous vaginal discharge that is increasing and now requires her to use a panty liner. The patient’s pregnancy has been complicated by gestational diabetes mellitus diagnosed at 26 weeks gestation. Due to uncontrolled glucose levels last week, an oral antihyperglycemic medication was prescribed; glucose level today shows improvement. The patient has no other chronic medical conditions. She exercises 3 days a week at a water aerobics class. The patient does not use tobacco, alcohol, or recreational drugs. She has no drug allergies. Temperature is 37.1 C (98.8 F), blood pressure is 120/76 mm Hg, and pulse is 74/min. Fundal height is 28 cm. Fetal heart rate is 150/min by Doppler ultrasonography. Pelvic examination shows a nontender, closed cervix without cervical discharge and a nontender gravid uterus. Thin, gray vaginal discharge is present, but no vesicles, ulcers, or other lesions are seen. There is no leakage of fluid through the cervix during the Valsalva maneuver. Microscopy of the vaginal fluid shows epithelial cells that have a stippled appearance but no ferning. Urine dipstick test is negative for protein and glucose.
Item 1 of 2
Which of the following is the most appropriate management of this patient’s condition?
CorrectIncorrect -
Question 5 of 40
5. Question
Item 2 of 2
The appropriate action is taken. The patient asks for the rationale of the management plan. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 6 of 40
6. Question
A 31-year-old woman, gravida 2 para 1, at 30 weeks gestation comes to the emergency department due to increased swelling in her face and lower extremities. She has noticed a sudden onset of swelling and a 2.72-kg (6-lb) weight gain in the last day. The patient has not urinated in the last 12 hours despite an increase in fluid intake. She has a twin pregnancy and no chronic medical conditions. Blood pressure is 154/98 mm Hg, and pulse is 98/min. Bladder catheterization yields a total of 10 mL of dark urine. Urinalysis shows no red blood cells. Which of the following pathologic factors is the most likely cause of this patient’s decreased urine output?
CorrectIncorrect -
Question 7 of 40
7. Question
A 21-year-old woman, gravida 1 para 0, comes to the office at 32 weeks gestation for a routine prenatal visit. The patient is doing well today and reports good fetal movement and no contractions or leakage of fluid. She has had an uncomplicated pregnancy so far. However, her prenatal care has been inconsistent. An initial prenatal visit at 12 weeks gestation confirmed her gestational age. A second-trimester anatomy ultrasound was normal. The patient has had no previous surgeries or chronic medical conditions. Prepregnancy weight was 50 kg (110 lb); she has since gained 4.5 kg (10 lb). Blood pressure is 138/82 mm Hg and pulse is 95/min. Fundal height is 28 cm and fetal heart rate is 152/min by Doppler. Urinalysis shows trace proteinuria. An ultrasound reveals a fetus in vertex positioning with an estimated fetal weight in the 9th percentile and an abdominal circumference <1st percentile. The placenta appears normal, the amniotic fluid index is 12 cm (normal: 5-24), and umbilical artery Doppler velocimetry is normal. In addition to serial umbilical Doppler ultrasounds, which of the following is the most appropriate management of this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
A 33-year-old woman, gravida 2 para 1 aborta 1, comes to the office for preconception counseling. The patient feels well. Her first pregnancy occurred 6 years ago and was complicated by diet-controlled gestational diabetes mellitus and preeclampsia with severe features that required hospitalization at 32 weeks gestation and cesarean delivery at 34 weeks gestation. After delivery, the patient was discharged on antihypertensives, which were discontinued 6 weeks postpartum. She had a normal 2-hour glucose tolerance test at the same visit. Her second pregnancy 4 years ago resulted in a spontaneous abortion at 7 weeks gestation. The patient has no other chronic medical conditions and only takes a daily prenatal vitamin. She practices yoga 4 or 5 times a week. The patient does not use tobacco or recreational drugs but drinks alcohol socially once or twice a month. Blood pressure is 100/70 mm Hg. BMI is 20 kg/m2. Pelvic examination is normal. She plans to try for pregnancy in the next few months. In addition to continuing prenatal vitamins, which of the following is the best advice for this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 30-year-old woman, gravida 2 para 1 aborta 1, comes to the office for preconception counseling. The patient’s first pregnancy 10 years ago resulted in a term cesarean delivery due to fetal malpresentation. That pregnancy was otherwise uncomplicated. She is now with a new partner and recently had a first-trimester spontaneous abortion. The patient has no chronic medical conditions, and her only surgery was the cesarean delivery. She takes a prenatal vitamin daily and drinks 2 cups of coffee each morning. The patient participates in a 30-minute high-intensity aerobics class 3 times a week and plays tennis every weekend. Blood pressure is 110/60 mm Hg and pulse is 68/min. BMI is 22 kg/m2. Physical examination shows a small, nontender, retroverted uterus; no adnexal masses or tenderness; and a cervix with no visible lesions or discharge. The patient wants to know what she can do to prepare for her next pregnancy. Which of the following is the most appropriate response regarding this patient’s risk for another spontaneous abortion?
CorrectIncorrect -
Question 10 of 40
10. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to the Next Item, you will not be able to add or change an answer.
A 23-year-old woman, gravida 3 para 2, at 35 weeks gestation comes to the emergency department due to vaginal bleeding. The bleeding began after intercourse, and she has since soaked 3 perineal pads in 2 hours. The patient reports normal fetal movement and mild intermittent cramping but no leakage of amniotic fluid. She has had limited prenatal care, and her only ultrasound at 7 weeks gestation was normal. The patient has a history of 2 prior cesarean deliveries at term. The first delivery was performed for a category III fetal heart rate tracing; the second was an elective repeat. The patient has a history of intravenous drug use and smokes a pack of cigarettes a day. She has no known drug allergies. Blood pressure is 130/70 mm Hg and pulse is 98/min. Fetal heart rate tracing is 140/min with moderate variability, accelerations, and no decelerations. The tocometer shows contractions every 5-7 minutes. On examination, the patient is in no distress. The abdomen is gravid, soft, and nontender. There is frank blood on the patient’s perineal pad.
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
Item 2 of 2
A bedside ultrasound reveals a low, posterior placenta that extends over the internal cervical os. The patient continues to have heavy vaginal bleeding, and a cesarean delivery is performed under spinal anesthesia. The neonate and placenta are delivered without difficulty. During repair of the uterine incision, she reports difficulty breathing shortly before becoming unresponsive. Blood pressure is 70/40 mm Hg, pulse is 124/min, and respirations are 34/min. Pulse oximetry is 86% on room air. A lung examination reveals decreased breath sounds bilaterally. Endotracheal intubation is performed, and the airway is secured. Profuse bleeding is noted from the uterine incision and placental bed. Examination of the Foley catheter reveals frank blood in the collection bag. Which of the following most likely led to this patient’s decompensation?
CorrectIncorrect -
Question 12 of 40
12. Question
A 36-year-old woman, gravida 6 para 5, at 41 weeks gestation is brought to the emergency department due to spontaneous rupture of membranes and painful contractions every 3 minutes. The patient’s current pregnancy has been uncomplicated. A 1-hour glucose challenge test was 155 mg/dL (normal: <140) at 28 weeks gestation; however, the confirmatory 3-hour glucose tolerance test was normal. She has no chronic medical conditions and has had no previous surgeries. Vital signs are normal. Fetal heart rate tracing is category 1, and the tocometer shows contractions every 3 minutes. Fundal height is 42 cm. Pelvic examination confirms rupture of membranes, and the cervix is dilated 5 cm. Following admission, the patient receives epidural analgesia for pain control, and labor progresses rapidly to 10-cm dilation. After 30 minutes of pushing, the fetal head delivers but immediately retracts against the perineum. She is instructed to push; gentle downward traction is applied to the fetal head, and the anterior fetal shoulder does not deliver. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
A 26-year-old woman, gravida 1 para 0, at 39 weeks gestation is admitted to the hospital with painful contractions. The patient has had no vaginal bleeding or rupture of membranes. Fetal movement is normal. Her pregnancy has been complicated by diet-controlled gestational diabetes mellitus. She has no other chronic medical conditions and has had no surgeries. Blood pressure is 120/70 mm Hg and pulse is 84/min. Fetal heart rate tracing shows a baseline of 140/min, moderate variability, accelerations, and no decelerations. The tocodynamometer shows contractions every 3 minutes. Cervical examination reveals the cervix to be 7 cm dilated and 100% effaced, with the fetal head at 0 station. Epidural anesthesia is administered. Two hours later, the patient is reevaluated for labor progression. Fetal heart tracing continues to be normal. The tocodynamometer now shows contractions every 4-6 minutes. Examination reveals the cervix to be 7 cm dilated and 100% effaced with the fetal head at 0 station, unchanged from the previous examination. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 27-year-old woman comes to the office for an infertility evaluation. She has been unable to conceive despite 2 years of frequent unprotected intercourse with her husband. The patient had a progestin-containing intrauterine device for 5 years, during which time she was amenorrheic. The intrauterine device was removed 2 years ago, but since then her periods have occurred every 2-4 months. The patient has no chronic medical conditions and has had no previous surgery. She had Chlamydia trachomatis cervicitis as a teenager but no other sexually transmitted infections. Pap tests, including the most recent a year ago, have all been normal. She takes a prenatal vitamin daily and does not use tobacco, alcohol, or recreational drugs. The patient is a graduate student and works at the university library. Blood pressure is 100/50 mm Hg and pulse is 68/min. BMI is 33 kg/m2. Terminal hair is noted above the upper lip. Breast examination shows terminal hair around the areola but no masses or discharge. The abdomen is soft and obese with no masses or tenderness. Nodulocystic acne is noted over the upper back. Pelvic examination shows a small, mobile uterus and no adnexal masses. TSH and FSH levels are normal but total testosterone level is elevated. The husband’s semen analysis is normal. A hysterosalpingogram shows bilateral intraabdominal spill from the fallopian tubes. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 34-year-old woman, gravida 3 para 2, at 12 weeks gestation comes to the office for a routine prenatal visit. The patient reports no nausea, vomiting, abdominal pain, or vaginal bleeding. The patient’s 2 previous pregnancies were complicated by poorly controlled type 2 diabetes mellitus and resulted in term cesarean deliveries for fetal macrosomia. Both children are healthy. The patient has no other chronic medical conditions. She takes a prenatal vitamin daily, and her glucose levels are controlled with an insulin regimen. She does not use tobacco, alcohol, or illicit drugs. Family history is noncontributory. Blood pressure is 120/70 mm Hg and pulse is 68/min. BMI is 30 kg/m2. Bedside Doppler examination reveals a fetal heart rate of 164/min. The patient requested a first-trimester combined test, and the results revealed normal-range nuchal translucency thickness, low pregnancy-associated plasma protein A, and an elevated β-hCG level. The results are discussed and the patient desires further management of these results. Which of the following is the best recommendation in management of this patient’s laboratory findings?
CorrectIncorrect -
Question 16 of 40
16. Question
A 38-year-old woman, gravida 3 para 2, at 35 weeks gestation comes to the emergency department due to sudden-onset visual changes and headache. The patient reports “spots” in her vision for the past few hours and an occipital headache. She took a dose of acetaminophen, but it did not improve her symptoms. The patient’s pregnancy has been complicated by gestational diabetes mellitus requiring insulin. Blood pressure is 168/114 mm Hg and pulse is 90/min. The pupils are equal and reactive to light. Extraocular movements are intact. Visual field testing shows partial loss of vision bilaterally. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 17 of 40
17. Question
A 29-year-old woman, gravida 1 para 0, at 39 weeks gestation comes to the emergency department due to painful contractions and vaginal spotting. The contractions occur every 5 minutes and started 6 hours ago, just after she experienced a gush of fluid. The patient reports normal fetal movement. Her prenatal course has been notable for many missed appointments. The patient’s last office visit was at 34 weeks gestation, and she has not been tested for group B Streptococcus (GBS) during this pregnancy. Temperature is 37.2 C (99 F) and blood pressure is 120/70 mm Hg. Fetal monitoring shows a baseline heart rate of 140/min, moderate variability, positive accelerations, and no decelerations; the tocodynamometer shows contractions every 5 minutes. Speculum examination confirms membrane rupture; on digital cervical examination, the cervix is 5 cm dilated and 80% effaced, with the head at −1 station. The patient is informed that she will be admitted due to ruptured membranes, and she asks if she will need antibiotics during labor. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 18 of 40
18. Question
A 25-year-old woman, gravida 1 para 0, comes to the office to establish prenatal care. The patient reports no nausea or vomiting, abdominal pain, or vaginal bleeding. However, over the past year, she has experienced progressive shortness of breath with daily activities and has recently noticed that her fingers turn blue with exertion. The patient has an unrepaired congenital ventricular septal defect with resulting pulmonary hypertension and heart failure that is managed with diuretics. Today, blood pressure is 110/80 mm Hg, pulse is 104/min, and respirations are 24/min. Pulse oximetry is 89% on room air. BMI is 23 kg/m2. A transvaginal ultrasound reveals a 6-week intrauterine gestation with a normal fetal heart rate. Recent echocardiogram showed an ejection fraction of 25%. The patient is concerned about her medical condition with this pregnancy and asks how it should be managed. Which of the following is the most appropriate management for this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
A 24-year-old woman is brought to labor and delivery after having a spontaneous vaginal delivery at home an hour ago. This was the patient’s first pregnancy. She did not receive prenatal care, and her pregnancy was at 39 weeks gestation by approximate last menstrual period. The patient has no chronic medical conditions and takes no medications. Prepregnancy BMI was 40 kg/m². On examination, the newborn boy is lying on the patient’s chest. The umbilical cord was clamped and cut immediately following delivery. He weighs 4.6 kg (10 lb 1 oz), and respirations are 70/min. The facies are symmetric with prominent cheeks. A systolic murmur is noted on cardiac examination. The skin appears reddish-purple. The remainder of the newborn’s examination is unremarkable. Maternal blood type is O, Rh D-negative. The newborn’s blood type is O, Rh D-positive. Which of the following is the most likely cause of this newborn’s presentation?
CorrectIncorrect -
Question 20 of 40
20. Question
A 19-year-old woman comes to the emergency department with pelvic pain, fever, and chills that began last night. The patient’s last menstrual period was 12 weeks ago, and she had a surgical pregnancy termination at a clinic 2 days ago. Temperature is 38.3 C (100.9 F), blood pressure is 92/60 mm Hg, and pulse is 102/min. Physical examination shows diffuse lower abdominal tenderness without rebound or guarding. Speculum examination reveals an open cervical os and malodorous tissue in the vaginal canal. Bimanual examination shows moderate uterine tenderness and no adnexal masses. Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 21 of 40
21. Question
A 31-year-old woman, gravida 2 para 1, at 36 weeks gestation comes to labor and delivery due to regular menstrual-like cramping and low back pain. She reports no leakage of fluid or vaginal bleeding; fetal movement is normal. The patient’s pregnancy has been uncomplicated. Her first pregnancy resulted in a vaginal delivery at 39 weeks gestation. The patient has no chronic medical conditions, and she had an appendectomy at age 15. She takes a prenatal vitamin daily and has no known medication allergies. Temperature is 36.7 C (98.1 F), blood pressure is 100/70 mm Hg, and pulse is 94/min. Fetal heart rate monitoring shows a baseline of 145/min, moderate variability, and no decelerations. The tocometer shows contractions every 3-4 minutes. On pelvic examination, the cervix is 4 cm dilated and 50% effaced. Ultrasound confirms a vertex presentation and an occiput posterior position. Prenatal laboratory results are significant for A, Rh(D)-negative blood type and a recent negative group B Streptococcus rectovaginal culture. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 22 of 40
22. Question
A 19-year-old woman, gravida 1 para 0, at 10 weeks gestation comes to the emergency room due to sudden-onset nausea, vomiting, and worsening abdominal pain. The nausea and vomiting began 3 days ago and were initially responsive to an over-the-counter antiemetic. However, for the last day, she has been unable to tolerate food and is now unable to tolerate liquids. For the past few hours, the patient has had severe pain in the right upper quadrant. She has not had any sick contacts, hematemesis, diarrhea, changes in stool color, or weight loss. The patient has sickle cell disease and had multiple episodes of dactylitis as a toddler; however, the last acute pain episode requiring hospitalization occurred several years ago. She was on penicillin prophylaxis until age 5 and is taking no daily medications. The patient is up to date on vaccinations. She was treated for trichomoniasis 2 years ago; recent sexually transmitted infection screening was negative. Temperature is 38.3 C (100.9 F), blood pressure is 140/80 mm Hg, pulse is 88/min, and respirations are 20/min. Pulse oximetry is 98% on room air. BMI is 21 kg/m2. Examination shows darkening of the sclerae. Cardiac examination is normal, and the lungs are clear to auscultation. The right upper quadrant is tender on abdominal examination, but there is no lower abdominal pain, rebound, or guarding. Pelvic examination shows no uterine tenderness. Deep tendon reflexes are 2+. Laboratory results are as follows:
Complete blood count
Hemoglobin
8 g/dL
Platelets
160,000/mm3
Leukocytes
13,800/mm3
Liver function studies
Aspartate aminotransferase (SGOT)
62 U/L
Alanine aminotransferase (SGPT)
49 U/L
Urinalysis
Protein
negative
Glucose
negative
Bacteria
none
Ultrasound reveals a 10-week intrauterine gestation with fetal cardiac activity. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
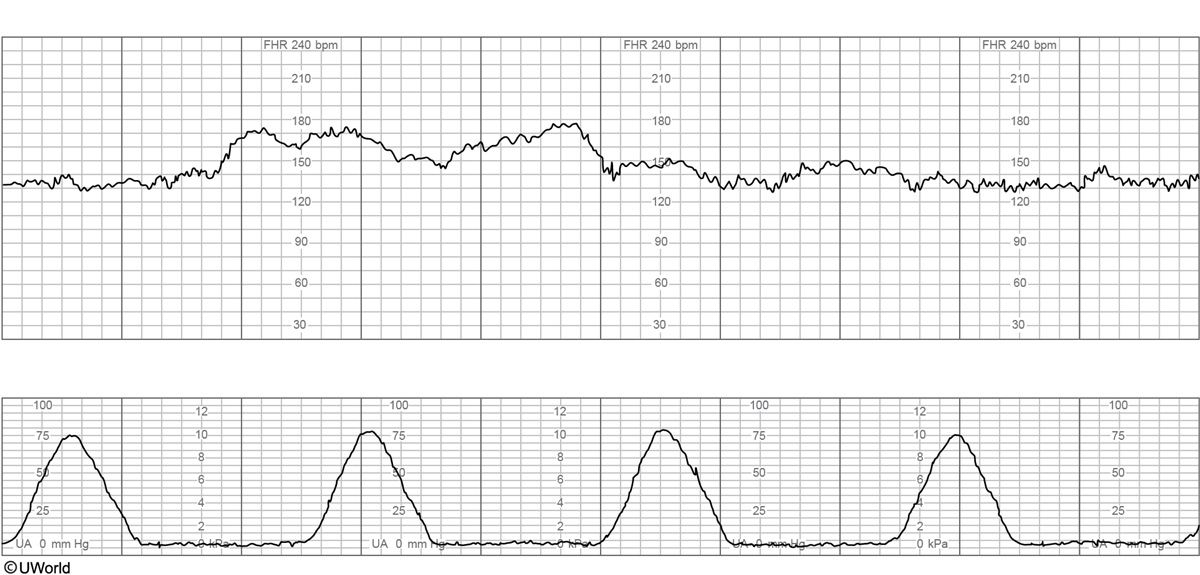
A 34-year-old woman, gravida 2 para 1, at 38 weeks gestation comes to the emergency department for contractions and vaginal spotting. The contractions started 4 hours ago and are now occurring every 3 minutes. She reports normal fetal movement and no leakage of fluid. The patient had no prenatal care but was hospitalized at 18 weeks gestation for viral gastroenteritis. A fetal ultrasound performed during this hospitalization was normal. The patient’s previous delivery, a year ago, was a term cesarean delivery for breech presentation. The patient has no chronic medical conditions and has had no other surgeries. She does not use tobacco, alcohol, or illicit drugs. Temperature is 36.7 C (98 F), blood pressure is 100/60 mm Hg, and pulse is 84/min. The fetal heart rate tracing is shown below:
Examination shows the cervix to be 5 cm dilated and 80% effaced, with the fetal head at 0 station. Blood type is O, Rh negative. The patient is admitted and epidural anesthesia is administered. Two hours later, the patient has spontaneous rupture of membranes and becomes acutely uncomfortable. Blood pressure is 140/92 mm Hg and pulse is 100/min. The fetal heart rate tracing now is shown below:
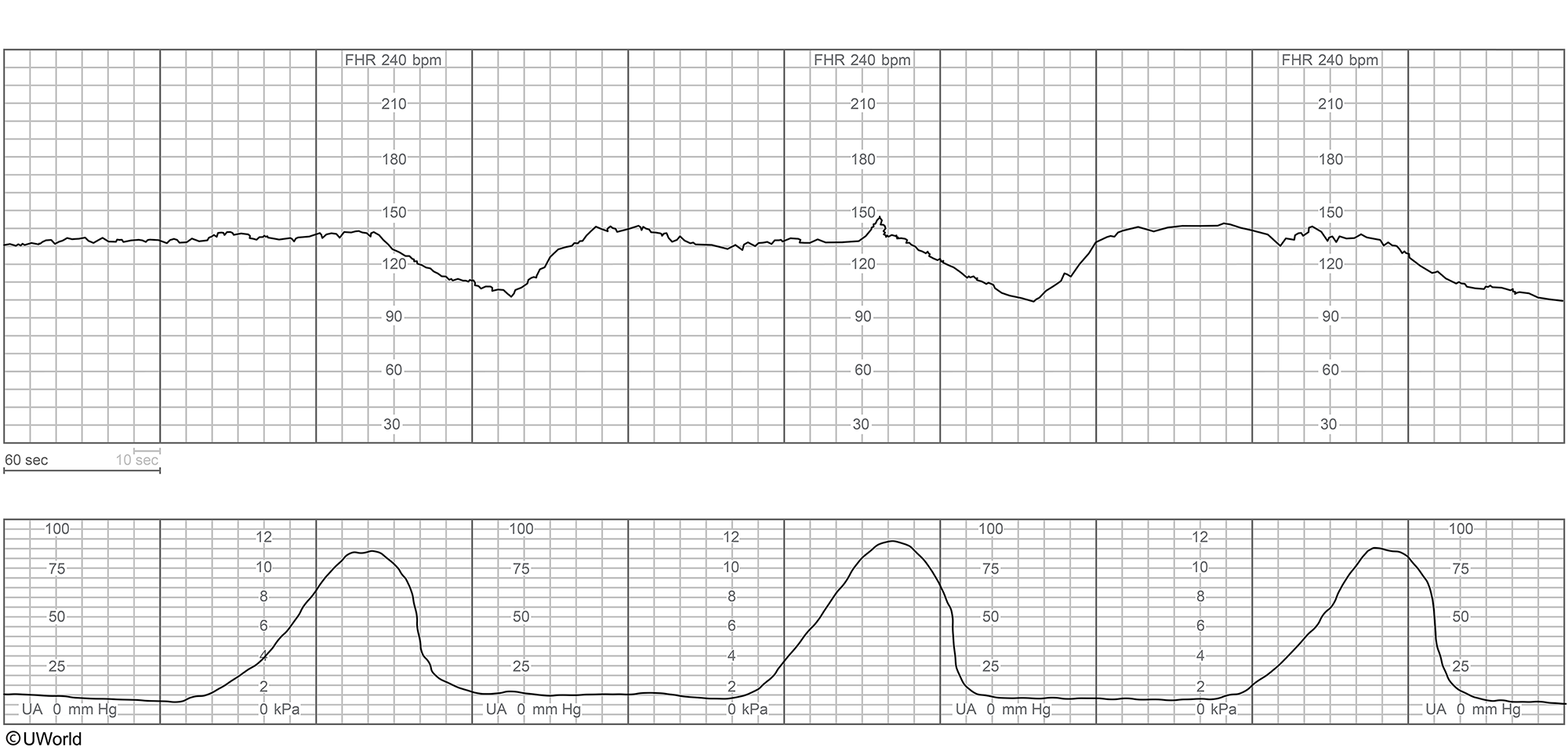
The patient begins to have heavy vaginal bleeding. The cervix is now 5 cm dilated and 80% effaced, with the fetal head at -3 station. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
A 33-year-old woman, gravida 2 para 1, comes to the office due to a positive home urine pregnancy test. Her last menstrual period was 6 weeks ago, and pelvic ultrasonography confirms an intrauterine pregnancy. The patient has idiopathic pulmonary hypertension complicated by Eisenmenger syndrome. She is aware that pregnancy poses a major mortality risk to herself and the fetus due to the hemodynamic changes of gestation, labor, and delivery. The patient consents to pregnancy termination with a mifepristone and misoprostol regimen. Which of the following is the mechanism of action for mifepristone in this clinical situation?
CorrectIncorrect -
Question 25 of 40
25. Question
A 37-year-old woman, gravida 1 para 0, at 27 weeks gestation comes to the emergency department due to nausea and back pain. Over the past week, the patient has noticed a progressive increase in back pain and swelling in her feet. This pregnancy has been complicated by large uterine fibroids. Prior to conception, the patient’s uterus measured 20 cm due to a large, right, lateral, fundal fibroid. Temperature is 37.2 C (99 F), blood pressure is 140/80 mm Hg, and pulse is 108/min. There is bilateral costovertebral angle tenderness. The lower extremities have 3+ pitting edema to the midshins. Bedside bladder ultrasound reveals minimal urine in the bladder; a catheter urinalysis is negative for nitrites and leukocyte esterase. Laboratory results are as follows:
First trimester
Today
Hemoglobin
11 g/dL
10.8 g/dL
Platelets
200,000/mm3
189,000/mm3
Leukocytes
8,000/mm3
10,000/mm3
Creatinine
0.6 mg/dL
1.7 mg/dL
Aspartate aminotransferase (SGOT)
12 U/L
15 U/L
Alanine aminotransferase (SGPT)
10 U/L
18 U/L
Renal ultrasound reveals severe hydronephrosis in the right kidney and moderate hydronephrosis in the left kidney. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 26 of 40
26. Question
A 35-year-old woman, gravida 1 para 0, at 27 weeks gestation is evaluated in the labor and delivery unit after she was involved in a motor vehicle collision in which the airbags deployed. She was the restrained driver with an appropriately placed lap-and-shoulder belt. After being evaluated in the emergency department and having a facial laceration repaired, the patient was transferred to labor and delivery for additional monitoring. She has dull abdominal pain but reports no vaginal bleeding or leakage of fluid and feels fetal movement. The patient has had no prenatal care other than a 9-week ultrasound and has no chronic medical conditions or prior surgeries. Blood pressure is 100/70 mm Hg, pulse is 104/min, and respirations are 16/min. Pulse oximetry is 99% on room air. The abdomen is mildly tender at the uterine fundus, without rebound or guarding. Sterile speculum examination shows a closed cervix with no vaginal bleeding or rupture of membranes. Fetal heart rate tracing has a baseline of 130/min with moderate variability, accelerations, and no decelerations. The tocometer exhibits low-amplitude contractions every 3 minutes. Initial laboratory results are as follows:
Complete blood count
Hemoglobin
9.6 g/dL
Platelets
180,000/mm3
Blood type
A, Rh negative
Antibody screen
negative
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
A 20-year-old woman, gravida 1 para 0, comes to the emergency department due to severe headache and right-sided weakness. The patient has had a constant, dull headache for the past week. The pain is greatest when she awakens in the morning. Coughing or straining worsens the pain and causes transient blurry vision. On awakening this morning, the patient was unable to stand due to right leg weakness, and she had difficulty calling for help because she could not pick up the phone with her right hand. She has no prior medical conditions. The patient is at 24 weeks gestation and had nausea and vomiting during the first trimester but no other pregnancy-related complications. Her only medication is a daily prenatal multivitamin. The patient stopped smoking cigarettes and drinking alcohol once she learned she was pregnant, and she has no history of recreational drug use. Her sister has a history of pulmonary embolism. Temperature is 36.7 C (98.1 F), blood pressure is 120/76 mm Hg, pulse is 80/min and regular, and respirations are 16/min. Bilateral pupils are equal, round, and reactive. Funduscopy shows bilateral papilledema. Neurologic examination is notable for right-sided motor weakness with pronator drift and Babinski sign on the right. Sensation is intact, and the patient has normal mentation. Meningeal signs are absent. Neuroimaging reveals intraluminal thrombus in the superior sagittal sinus and a small area of juxtacortical intraparenchymal hemorrhage. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 28-year-old woman, gravida 1 para 0, at 37 weeks gestation comes to the emergency department due to leakage of fluid and painful uterine contractions that occur every 2-5 minutes. The patient has a spontaneous dichorionic/diamniotic twin gestation; her pregnancy has otherwise been uncomplicated. Serial ultrasonography throughout the pregnancy has consistently shown concordant growth of the twins. The patient has no chronic medical conditions and has had no surgeries. Examination confirms rupture of membranes; on digital examination, the cervix is 5 cm dilated. Bedside ultrasonography reveals that the twins are in vertex/vertex presentation. The patient is admitted for labor, and epidural analgesia is administered. Eight hours after admission, the patient’s cervix is completely (10 cm) dilated, and twin A is delivered vaginally with Apgar scores of 8 and 9 at 1 and 5 minutes, respectively. The patient is reexamined, and the cervix has contracted to 9 cm, 100% effaced, with the vertex of twin B at −2 station. The amniotic membranes are intact. Fetal heart tracing is category 1. Tocometry shows contractions every 2-3 minutes. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
A 27-year-old woman, gravida 3 para 1 aborta 1, at 36 weeks gestation comes to the emergency department due to abdominal pain and heavy vaginal bleeding that began acutely an hour ago. She reports no leakage of fluid. The patient’s 11-week and 18-week ultrasounds revealed a singleton intrauterine pregnancy with a posterior placenta. She was previously evaluated in the emergency department at 27 weeks gestation for preterm contractions after she fell on her abdomen. Her examination at that time was normal and she was discharged without intervention. The patient has no chronic medical conditions. Her pregnancy history includes an 8-week spontaneous abortion and a cesarean delivery after a failed labor induction. The patient smokes ½ pack of cigarettes a day, but does not drink alcohol or use illicit drugs. She takes a daily prenatal vitamin and iron supplementation. Temperature is 36.7 C (98 F), blood pressure is 110/60 mm Hg, and pulse is 94/min. The fetal heart rate tracing shows a baseline of 150/min, moderate variability, no accelerations, and occasional late decelerations. Tocometer shows contractions every 2 minutes. Abdominal examination demonstrates a firm, tender, gravid abdomen. Speculum examination shows 50 mL of clotted blood in the vagina and continued heavy bleeding. The cervix is 4 cm dilated and 80% effaced, with the fetal head at 0 station. Which of the following is the most likely cause of this patient’s presentation?
CorrectIncorrect -
Question 30 of 40
30. Question
A 32-year-old woman, gravida 3 para 2, at 38 weeks gestation is admitted to labor and delivery for contractions and vaginal spotting. The patient reports good fetal movement and no rupture of membranes. Her last prenatal visit was at 18 weeks gestation. She has no chronic medical conditions or previous surgeries. Her first 2 pregnancies ended in uncomplicated vaginal deliveries. The patient takes a prenatal vitamin daily. She smoked cigarettes occasionally prior to this pregnancy but does not use alcohol or recreational drugs. Temperature is 36.7 C (98 F), blood pressure is 110/80 mm Hg, and pulse is 76/min. The fetal heart rate tracing shows a baseline of 140/min, moderate variability, multiple accelerations, and no decelerations. The tocometer shows contractions every 3 minutes. On pelvic examination, several flesh-colored, hyperkeratotic papules are noted on the posterior introitus, labia majora, and labia minora. The papules are 1-2 cm in diameter, have a smooth surface, and are sessile. The cervix is 5 cm dilated and 90% effaced. The patient’s sexually transmitted infection screen at her initial prenatal visit was negative. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 16-year-old girl, gravida 1 para 0, at 6 weeks gestation comes to the office for an initial prenatal visit. The patient reports mild nausea and vomiting in the morning but is able to drink and eat small meals in the afternoon. She had vaginal spotting a week ago, but the bleeding has resolved. The patient has no chronic medical conditions and has had no surgeries. She was taking oral contraceptive pills inconsistently but stopped 2 weeks ago when she realized she was pregnant. The patient started a daily prenatal vitamin at that time. Her mother had 3 pregnancies, all of which ended in uncomplicated vaginal deliveries at term. The patient has no known medication allergies and does not use tobacco, alcohol, or recreational drugs. Blood pressure is 110/60 mm Hg and pulse is 68/min. BMI is 24 kg/m2. Speculum examination shows a closed cervix and no vaginal bleeding or lesions. Bimanual examination shows a 6-week-sized uterus and no adnexal masses. A pelvic ultrasound confirms a 6-week intrauterine gestation with a normal fetal heart rate. This patient is at increased risk for which of the following pregnancy complications?
CorrectIncorrect -
Question 32 of 40
32. Question
A 27-year-old woman, gravida 1 para 0, at 9 weeks gestation comes to the office for an initial prenatal visit. She feels well and has had no abdominal pain or vaginal bleeding. The patient has sickle cell disease and has had multiple hospitalizations and transfusions for acute pain episodes. She was on hydroxyurea, but it was discontinued several months ago when she began attempting conception. The patient has had no acute pain episodes since discontinuation of the medication. She has no other chronic medical conditions. The patient is up to date on vaccinations. Temperature is 36.7 C (98.1 F), blood pressure is 150/80 mm Hg, and pulse is 76/min. Pulse oximetry is 99% on room air. BMI is 22 kg/m2. Cardiac examination reveals a normal rate and regular rhythm. The lungs are clear to auscultation bilaterally. Pelvic examination demonstrates a 9-week-sized uterus without adnexal masses or tenderness. Urine dipstick shows 1+ proteinuria. Ultrasound confirms a 9-week intrauterine gestation with fetal cardiac activity. In addition to routine prenatal laboratory testing, which of the following is the next best step in management of this patient?
CorrectIncorrect -
Question 33 of 40
33. Question
A 29-year-old Asian woman, gravida 1 para 0, comes to the office at 26 weeks gestation for prenatal care. The patient has no abdominal pain, vaginal bleeding, or leakage of fluid. Fetal movement is normal. For the last few weeks, she has become increasingly fatigued and is sleeping at least 8 hours a night in addition to taking an afternoon nap. Her pregnancy has been uncomplicated and initial prenatal laboratory results were as follows:
Complete blood count
Hemoglobin
11 g/dL
Platelets
280,000/mm3
Immunologic and rheumatologic studies
Hepatitis panel
Hepatitis B surface antigen
negative
HIV screening
HIV-1 antibody
negative
HIV-2 antibody
negative
Rapid plasma reagin
negative
The patient has no chronic medical conditions and has had no previous surgeries. She takes a daily prenatal vitamin; however, she was unable to begin taking it until 18 weeks gestation due to daily nausea and vomiting. Blood pressure is 110/60 mm Hg and pulse is 64/min. Weight is 60 kg (132.3 lb), a 5-kg (11-lb) increase from her prepregnancy weight. Fetal heart rate is 145/min by Doppler ultrasound. Fundal height is 26 cm. Urine dipstick is negative for protein and glucose. Routine third-trimester laboratory results include the following:
Hemoglobin
9 g/dL
Glucose
80 mg/dL
Rapid plasma reagin
negative
The results of a peripheral blood smear are shown below:
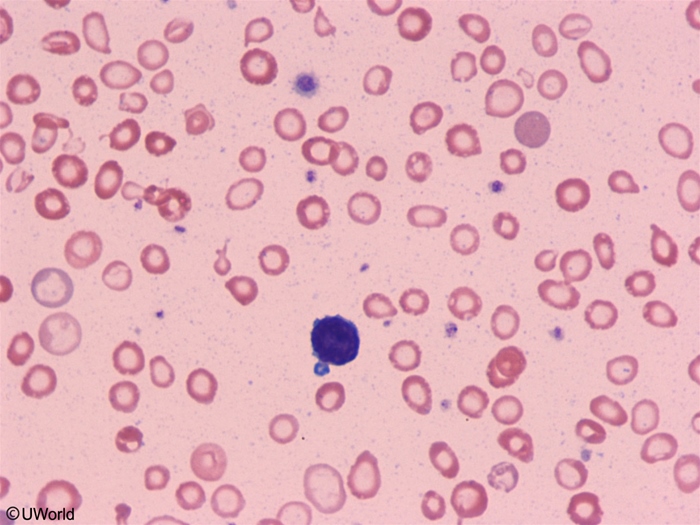
The patient asks about the cause of her fatigue and whether she needs treatment. Which of the following is the most appropriate response to this patient?
CorrectIncorrect -
Question 34 of 40
34. Question
A 33-year-old woman, gravida 2 para 1, is brought to the labor and delivery unit at 32 weeks gestation and precipitously delivers a male infant within 2 minutes of arrival. The infant appears small for gestational age. Apgar scores are 5 and 6 at 1 and 5 minutes, respectively. The mother did not receive prenatal care with this pregnancy. On delivery, the placenta appears pale and enlarged. In addition, the umbilical cord is inflamed with multiple areas of abscess-like foci of necrosis surrounding the umbilical vessels. Which of the following is the most likely cause of these findings?
CorrectIncorrect -
Question 35 of 40
35. Question
A 30-year-old, primigravid, previously healthy woman at 39 weeks gestation is admitted to labor and delivery due to active labor. After pushing for 2 hours, the patient delivers a 3.6-kg (8-lb) infant over an intact perineum. Immediately after delivery of the placenta, she develops brisk vaginal bleeding. The uterine fundus is soft, and the lower uterine segment is atonic. Uterotonic therapy is administered, and bimanual massage is performed, but the patient continues to bleed heavily. The patient becomes hemodynamically unstable, and a blood transfusion is started, but the patient continues to have heavy bleeding with an estimated blood loss of 3,000 mL. She is taken to the operating room, and an emergency hysterectomy is performed. Which of the following strategies is most recommended to reduce the rate of complications for similar patients?
CorrectIncorrect -
Question 36 of 40
36. Question
A 20-year-old woman, gravida 1 para 0, at 12 weeks gestation comes to the office for routine prenatal care during the fall season. She has mild nausea, which she controls with vitamin B supplementation, but no abdominal pain or vaginal bleeding. The patient has no chronic medical conditions or previous surgeries. She takes a daily prenatal vitamin. She is currently in a monogamous relationship and has had 1 partner previously. The patient does not use tobacco, alcohol, or illicit drugs. She did not receive any routine childhood vaccinations but does not object to vaccination. She plans to start taking college courses in the next few years. The patient has no known allergies. Blood pressure is 120/70 mm Hg and pulse is 65/min. BMI is 23 kg/m2. The fetal heart rate is 150/min by bedside Doppler ultrasonography. Initial prenatal laboratory results are as follows:
Rubella antibody
negative
Varicella antibody
negative
Blood type
O, Rh negative
Which of the following preventive vaccines is most appropriate for this patient at this visit?
CorrectIncorrect -
Question 37 of 40
37. Question
A 24-year-old primigravid woman at 35 weeks gestation comes to the office for a routine prenatal visit. The patient reports no leakage of fluid or vaginal bleeding but has noticed occasional painless uterine contractions over the past week. Fetal movement is normal. Her pregnancy has been uncomplicated. The patient has no chronic medical conditions and has had no surgeries. She takes a daily prenatal vitamin and has not used tobacco, alcohol, or recreational drugs during the pregnancy. The patient takes a prenatal yoga class 3 times a week. Blood pressure is 130/80 mm Hg and pulse is 68/min. BMI is 28 kg/m2. Fetal heart rate is 142/min by Doppler ultrasound. Fundal height is 32 cm. Pelvic examination shows the cervix to be closed and long with the fetal presenting part at −2 station. Ultrasound reveals a fetus in footling breech presentation with an estimated fetal weight at the 25th percentile for gestational age, a fundal placenta, and a normal amniotic fluid level. The diagnosis of breech presentation is reviewed with the patient, who responds by saying, “I am really hoping for a vaginal delivery.” Which of the following is the most appropriate response to this patient?
CorrectIncorrect -
Question 38 of 40
38. Question
A 26-year-old primigravid woman at 30 weeks gestation comes to the emergency department due to hematuria that she has had along with dysuria for the past day. The patient was seen in the office 2 days ago for increased urinary frequency and urgency; a urine culture was collected and is still pending. She was prescribed nitrofurantoin for a suspected urinary tract infection, but she did not take her first dose until a few hours ago. The patient has had no contractions, vaginal bleeding, or leakage of fluid. She has no chronic medical conditions and no prior surgeries. Temperature is 37.3 C (99.1 F), blood pressure is 108/72 mm Hg, pulse is 96/min, and respirations are 20/min. Fetal heart tones are 150/min. Cardiopulmonary examination is normal. On abdominal examination, the uterus is gravid and nontender with a fundal height of 31 cm. There is no costovertebral angle tenderness. Laboratory results are as follows:
Complete blood count
Hemoglobin
11 g/dL
Platelets
160,000/mm3
Leukocytes
16,100/mm3
Serum chemistry
Chloride
102 mEq/L
Potassium
3.8 mEq/L
Bicarbonate
18 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.6 mg/dL
Glucose
120 mg/dL
Urinalysis
Specific gravity
Protein
+1
Glucose
negative
Leukocyte esterase
positive
Nitrites
positive
Bacteria
many
White blood cells
50+/hpf
Red blood cells
20-30/hpf
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 21-year-old woman, gravida 1 para 1, comes to the emergency department for abdominal pain and a severe headache. The pain started 2 days ago in the epigastrium and now radiates to the right upper quadrant. The pain was initially responsive to acetaminophen but has become increasingly severe. The patient also reports an occipital headache accompanied by blurry vision. A week ago, she had an uncomplicated vaginal delivery at 39 weeks gestation and, after a normal postpartum course, was discharged on day 2. The patient has a history of migraines for which she typically takes daily prophylactic medication. She stopped the medication when she became pregnant. Temperature is 36.7 C (98 F), blood pressure is 150/90 mm Hg, and pulse is 94/min. The visual fields are normal and there is no nuchal rigidity. Abdominal examination reveals tenderness to palpation over the epigastrium and right upper quadrant, and there is hepatomegaly. Bilateral lower extremities have 2+ pitting edema to the knees. Laboratory results are as follows:
Hematocrit
26%
Platelets
60,000/mm3
Total bilirubin
1.6 mg/dL
Direct bilirubin
0.5 mg/dL
Alkaline phosphatase
220 U/L
Aspartate aminotransferase
137 U/L
Alanine aminotransferase
149 U/L
Lactate dehydrogenase, serum
436 U/L
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 32-year-old woman comes to the office to discuss possible bariatric surgery. The patient has a history of obesity that has not responded to dietary modification and exercise. She has no other chronic medical conditions and has had no previous surgeries. The patient does not use tobacco, alcohol, or recreational drugs. She is considering pregnancy after her bariatric surgery. Blood pressure is 130/80 mm Hg and pulse is 86/min. BMI is 42 kg/m2. The remainder of the physical examination is unremarkable. Which of the following is the most appropriate statement regarding pregnancy after bariatric surgery?
CorrectIncorrect
