Cardiovascular Pharmacology 2
Time limit: 0
Quiz Summary
0 of 37 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 37 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- NBME 7 BLOCK 4 0%
- Pediatrics 0%
Would you like to submit your quiz result to the leaderboard?
![captcha]()
Loading
| Pos. | Name | Entered on | Points | Result |
|---|---|---|---|---|
| Table is loading | ||||
| No data available | ||||
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 37
1. Question
A 6-day-old boy in the neonatal intensive care unit has a heart murmur. The patient was born at 27 weeks gestation and intubated due to surfactant deficiency. Birth weight was 1.14 kg (2 lb 8 oz). Temperature is 37 C (98.6 F), blood pressure is 66/12 mm Hg, and pulse is 182/min. A continuous murmur with systolic accentuation is best heard at the left heart border. There are bounding femoral and palmar pulses. Abdominal examination is unremarkable. Blood culture is sterile. Elevated levels of which of the following substances is most likely contributing to this patient’s condition?
CorrectIncorrect -
Question 2 of 37
2. Question
A 53-year-old man comes to the physician for a follow-up visit after an acute myocardial infarction. His medications include metoprolol and low-dose aspirin. He used to smoke 2 packs of cigarettes daily but quit after his myocardial infarction. The patient’s father has hypertension and his mother has type 2 diabetes mellitus. He currently weighs 100 kg (220 lb) and is 178 cm (70 in) tall. Examination shows an obese male with no other abnormalities. His total serum cholesterol level is 155 mg/dL, with an HDL level of 27 mg/dL and a triglyceride level of 92 mg/dL. Which of the following lipid-lowering agents would be most effective for preventing future cardiovascular events in this patient?
CorrectIncorrect -
Question 3 of 37
3. Question
A 79-year-old man is brought to the hospital due to confusion for the past 2 days. The patient has had nausea, decreased appetite, and poor oral intake for several weeks. He has also mentioned that everything around him has “a yellow tint.” He has no abdominal pain. Medical history includes long-standing heart failure with reduced ejection fraction and atrial fibrillation. Medications include metoprolol, digoxin, lisinopril, and apixaban. The patient is afebrile. Blood pressure is 130/80 mm Hg and pulse is 58/min. The abdomen is soft and nontender; there is no rigidity or rebound and no masses are present. Age-related changes in which of the following factors most likely accounts for this patient’s symptoms?
CorrectIncorrect -
Question 4 of 37
4. Question
A 36-year-old man comes to the office after he was found to have an abnormal lipid panel during employee wellness testing at his company. He has no prior medical problems and takes no medications. The patient is a software technician and has a sedentary lifestyle. He eats mostly fast foods, rarely exercises, and drinks 2-3 cans of beer daily. His BMI is 31 kg/m2. Physical examination is unremarkable. Results of laboratory studies performed in the office are as follows:
Total cholesterol 290 mg/dL High-density lipoprotein 45 mg/dL Low-density lipoprotein 110 mg/dL Triglycerides 675 mg/dL Lifestyle modification with a balanced diet, regular exercise, and reduced alcohol intake is advised. He is also started on fenofibrate therapy. This medication is most likely to help the patient by which of the following mechanisms?
CorrectIncorrect -
Question 5 of 37
5. Question
A 72-year-old man is brought to the hospital due to severe substernal chest pain and shortness of breath for the last several hours. The pain started suddenly when he was outside working in the garden. Medical history includes diet-controlled diabetes mellitus and hypertension. Physical examination reveals bilateral crackles and a third heart sound. ECG shows ST elevation in multiple leads. The patient is diagnosed with an acute myocardial infarction complicated by acute severe heart failure. He is started on dobutamine infusion and prepared for coronary catheterization. Which of the following is most likely to be increased due to the medication used in this patient?
CorrectIncorrect -
Question 6 of 37
6. Question
A 71-year-old woman comes to the emergency department due to progressive dyspnea and orthopnea for the last week. She has a history of myocardial infarction and systolic heart failure with a left ventricular ejection fraction of 15%. The patient is compliant with her medications, which include carvedilol, furosemide, aspirin, lisinopril, and atorvastatin. Blood pressure is 118/74 mm Hg and pulse is 72/min. Examination reveals elevated jugular venous pressure, bibasilar crackles, an S3 heart sound, and bilateral lower extremity pitting edema. The patient is started on dobutamine infusion, which provides significant symptom relief. Echocardiogram shows mild improvement in cardiac contractility. Which of the following is the likely mechanism underlying this patient’s clinical improvement?
CorrectIncorrect -
Question 7 of 37
7. Question
A 45-year-old man comes to the clinic due to recurrent palpitations accompanied by chest discomfort and shortness of breath. A year ago, he was diagnosed with paroxysmal atrial fibrillation treated with rate control using a beta blocker. Past medical history is also significant for hypertension and obesity. Echocardiogram shows left atrial enlargement, normal left ventricular ejection fraction, and no significant valvular disease. 24-hour Holter monitoring reveals bursts of atrial fibrillation associated with the patient’s symptoms. He is initiated on dofetilide to maintain normal sinus rhythm. This medication exerts its main effect on which portion of the action potential curve?
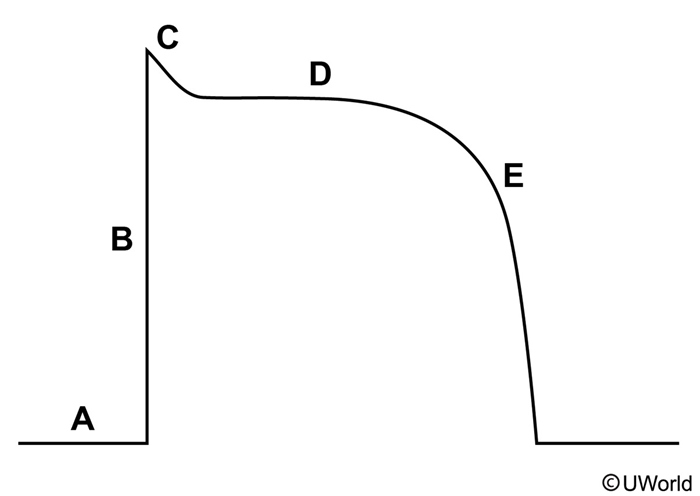 CorrectIncorrect
CorrectIncorrect -
Question 8 of 37
8. Question
A 47-year-old man comes to the office due to worsening muscle weakness and dark urine for the past several days. Two weeks ago, the patient was evaluated for dyspepsia and found to have Helicobacter pylori infection; he was started on treatment and has had partial symptom improvement. Medical history includes hypertension and hyperlipidemia, for which he takes amlodipine and simvastatin. Temperature is 37.1 C (98.8 F), blood pressure is 130/80 mm Hg, and pulse is 74/min. Physical examination shows diffuse muscle tenderness. Laboratory evaluation reveals elevated blood urea nitrogen and serum creatinine levels. Urine microscopy shows no red or white blood cells. Which of the following medications most likely precipitated this patient’s current condition?
CorrectIncorrect -
Question 9 of 37
9. Question
A 60-year-old man comes to the emergency department with dizziness and palpitations. He woke up this morning with an intermittent pounding sensation in his chest. The patient has occasionally experienced a similar sensation in the past and did not think it was serious. Later, while mowing the lawn, he became lightheaded and had to sit down to avoid passing out. After receiving the appropriate workup, the patient is diagnosed with a cardiac arrhythmia and started on a medication known to prolong the QT interval. However, the drug is associated with a lower incidence of torsade de pointes than other QT-prolonging agents. Which of the following medications was most likely used in this patient?
CorrectIncorrect -
Question 10 of 37
10. Question
A 66-year-old man comes to the emergency department due to several episodes of lightheadedness and a recent fall. The symptoms are especially pronounced in the morning when he gets up from bed. The patient takes medications for hypertension, stable angina pectoris, gout, and benign prostate hyperplasia. He also has osteoarthritis of the right knee and takes occasional nonsteroidal anti-inflammatory drugs. His blood pressure is 120/80 mm Hg and pulse is 70/min in the supine position, and 90/60 mm Hg and 87/min on standing, respectively. Cardiopulmonary examination is normal. Blockade of which of the following receptors is most likely contributing to this patient’s current condition?
CorrectIncorrect -
Question 11 of 37
11. Question
A 50-year-old man is brought to the ER with severe dizziness and confusion. He states that he had an episode of chest pain and took several tablets of nitroglycerin. His current medications include a daily aspirin for heart attack prevention, an occasional acetaminophen for headaches and occasionally tadalafil for erectile dysfunction. His blood pressure is 50/20 mmHg and his heart rate is 120 beats/min. Which of the following cellular changes is most likely responsible for this patient’s symptoms?
CorrectIncorrect -
Question 12 of 37
12. Question
A 47-year-old man with known coronary artery disease comes to the emergency department with chest tightness, sweating, and palpitations. His symptoms began abruptly 2 hours ago while he was at work. Six months ago, the patient underwent percutaneous angioplasty of the right coronary artery. Past medical history also includes anxiety and panic attacks. Blood pressure is 180/90 mm Hg and pulse is 110/min with a regular rhythm. An esmolol infusion produces rapid symptom relief and heart rate slowing. Which of the following portions of the ECG will be affected most significantly by the medication?
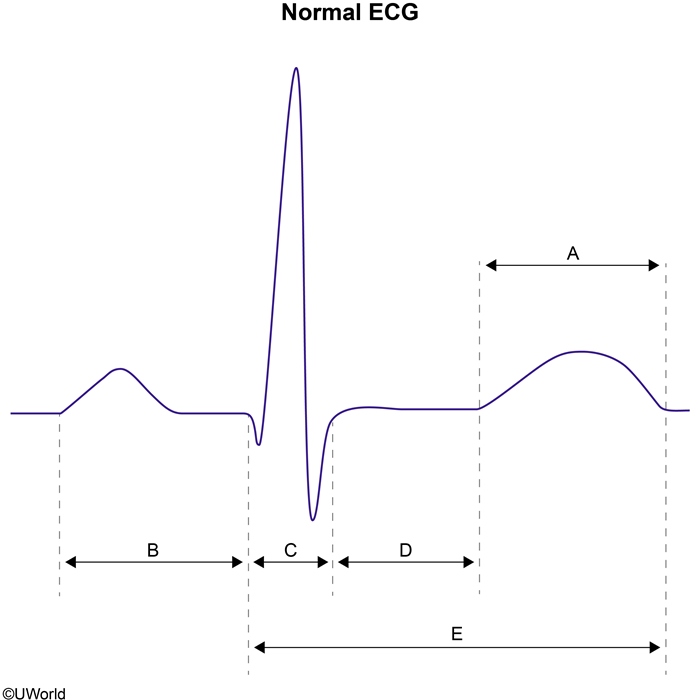 CorrectIncorrect
CorrectIncorrect -
Question 13 of 37
13. Question
A 64-year-old man with a long-standing history of hypertension is brought to the emergency department with a dry cough and shortness of breath. The patient has been unable to sleep in the flat position for the past 2 days. Blood pressure is 192/102 mm Hg and pulse is 92/min and regular. Physical examination reveals an S4 and bibasilar crackles. He is started on intravenous nitroglycerin infusion and soon after reports significant symptomatic relief. Which of the following physiologic changes are most likely to occur following administration of this medication?
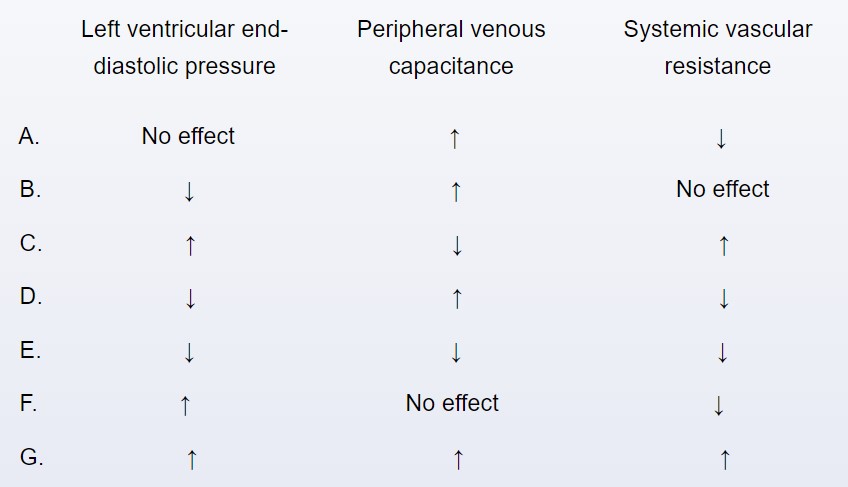 CorrectIncorrect
CorrectIncorrect -
Question 14 of 37
14. Question
An 82-year-old man is brought to the emergency department after a syncopal episode. He has had no chest pain or dyspnea but he has constipation of recent onset. He was hospitalized 2 weeks ago for atrial fibrillation with rapid ventricular response and was discharged home with oral medications after appropriate management. Medical history is also significant for hypertension and severe chronic obstructive pulmonary disease requiring home supplemental oxygen. Blood pressure is 105/60 mm Hg and pulse is 50/min. Examination reveals bilaterally decreased breath sounds, no wheezing, and normal heart sounds. ECG shows new-onset second-degree atrioventricular block. Which of the following drugs is the most likely cause of his current condition?
CorrectIncorrect -
Question 15 of 37
15. Question
A 65-year-old immigrant from Eastern Europe comes to the physician because of a four-week history of low-grade fever, multiple joint pains, and a well-demarcated erythematous rash on his face and trunk. The patient denies hair loss, mucosal ulceration, or photosensitivity. His serum test is positive for the presence of anti-nuclear antibody (ANA) in very high titers. The patient reports a past medical history of coronary artery disease, congestive heart failure, and “cardiac rhythm abnormalities.” This patient should be specifically questioned about the intake of which of the following medications?
CorrectIncorrect -
Question 16 of 37
16. Question
A 60-year-old man is diagnosed with exertional angina. His treatment regimen includes metoprolol, isosorbide dinitrate and aspirin. He takes isosorbide dinitrate early in the morning and again in the afternoon, but he does not take an evening dose. Such a pattern of drug administration is intended to decrease which of the following?
CorrectIncorrect -
Question 17 of 37
17. Question
A 44-year-old man reports exertional shortness of breath and palpitations. On examination, he has a systolic murmur at the left sternal border and cardiac apex, which gets louder when he stands up. He is diagnosed with obstructive hypertrophic cardiomyopathy and paroxysmal atrial fibrillation, and is started on a medication. Changes in the action potential of ventricular muscle cells before and after administration of medication are shown in the image below
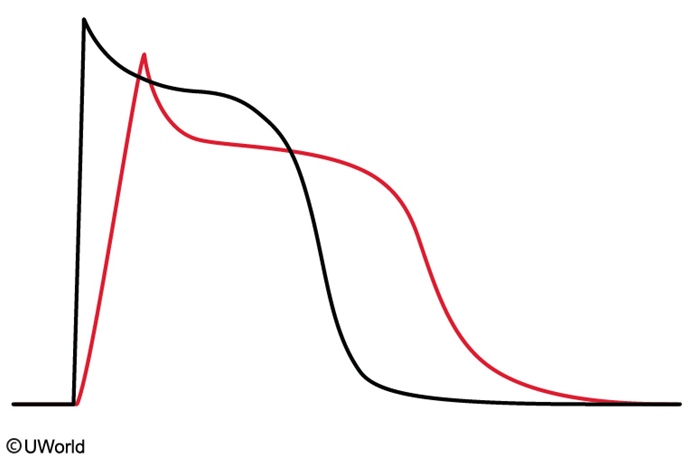
Black curve = Before administration of medication
Red curve = After administration of medicationThe patient is most likely being treated with which of the following medications?
CorrectIncorrect -
Question 18 of 37
18. Question
A 60-year-old man who was recently diagnosed with hypertension comes to the office for follow-up. He was treated with lisinopril but stopped a week ago due to a dry, nagging cough. Past medical history is notable for type 2 diabetes mellitus with moderately increased albuminuria but normal creatinine clearance. His other medications include metformin and rosuvastatin. The patient does not smoke or drink alcohol. His blood pressure is 150/92 mm Hg. BMI is 31 kg/m2. Physical examination, including the heart and lungs, is unremarkable. Which of the following is the best treatment for this patient’s hypertension?
CorrectIncorrect -
Question 19 of 37
19. Question
A 54-year-old man with nonischemic cardiomyopathy comes to the office for a follow-up visit. He has been hospitalized frequently for acute decompensated heart failure, and currently has dyspnea on mild exertion. The patient also has a history of hypertension and takes multiple medications. Blood pressure is 116/70 mm Hg, and pulse is 72/min and regular. Physical examination shows elevated jugular venous pressure, bibasilar lung crackles, and lower extremity edema. Serum creatinine is 1.0 mg/dL and serum potassium is 4.2 mEq/L. Three weeks after starting digoxin therapy, the patient reports symptomatic improvement. Which of the following is the initial cellular event triggering this response to the new medication?
CorrectIncorrect -
Question 20 of 37
20. Question
A 34-year-old man is found to have dyslipidemia. His other medical problems include a myocardial infarction 1 week ago. His father died of myocardial infarction at the age of 48 years. Several other family members have had myocardial infarctions and hypertension. The patient smoked cigarettes and drank alcohol occasionally but quit after his myocardial infarction. He is started on simvastatin and cholestyramine. Which of the following best describes the independent effects of simvastatin and cholestyramine, respectively, on hepatic cholesterol synthesis?
CorrectIncorrect -
Question 21 of 37
21. Question
A 42-year-old woman comes to the office with persistent hyperlipidemia despite 6 months of maintaining a healthy diet and exercising regularly. Although her past medical history is significant for biliary colic secondary to gallstones, the patient has refused elective cholecystectomy. Her father died of a myocardial infarction at age 54, and her mother has diabetes mellitus. The patient’s temperature is 36.1 C (97 F), blood pressure is 122/79 mm Hg, pulse is 78/min, and respirations are 14/min. Examination shows no abnormalities. Laboratory studies obtained 1 week ago show elevated serum triglycerides and LDL cholesterol levels. Drug therapy is discussed with the patient. Given this patient’s preexisting gallbladder disease, which of the following drugs should be avoided?
CorrectIncorrect -
Question 22 of 37
22. Question
A 60-year-old man comes to the clinic for a preoperative evaluation. The patient has severe osteoarthritis of the right knee, and an elective total knee arthroplasty has been planned. Other medical conditions are well-controlled hypertension and stable coronary artery disease. Vital signs are within normal limits. Physical examination is unremarkable. The patient is educated to avoid taking over-the-counter NSAIDs immediately prior to surgery due to risk of excessive perioperative bleeding. He is also instructed to discontinue low-dose aspirin at least 5 days prior to surgery. Which of the following is the most likely reason for stopping this drug well in advance of surgery?
CorrectIncorrect -
Question 23 of 37
23. Question
A 62-year-old man comes to the office for follow-up of hypertension. He was diagnosed with hypertension 10 years ago and has been treated with a number of different medications. However, the patient has had to discontinue several medications due to side effects such as dizziness, palpitations, and headaches. Currently he takes ramipril and chlorthalidone and is tolerating them well. Blood pressure is 160/92 mm Hg and was 158/89 mm Hg at his most recent prior visit. ECG shows sinus bradycardia (55/min) with PR interval prolongation (280 msec). Which of the following medications would be most effective for lowering this patient’s blood pressure without worsening his ECG abnormalities?
CorrectIncorrect -
Question 24 of 37
24. Question
A 60-year-old man comes to the office for follow-up due to persistent atrial fibrillation. He reports occasional palpitations and poor exercise tolerance. For the past year, the patient’s atrial fibrillation has been managed with a rate-control strategy using metoprolol. Three months ago, his metoprolol dosage was increased for improved rate control, but today in the office, he reports that he was unable to tolerate the new dosage due to dizziness. Blood pressure is 110/70 mm Hg and pulse is 105/min and irregular. Examination shows no abnormalities. Echocardiography reveals left atrial enlargement, an ejection fraction of 59%, and no significant valvular disease. The patient is advised to remain on his previously tolerated metoprolol dose, and digoxin is added to the medication regimen. Four weeks later, he reports symptom improvement. Resting pulse is 84/min and irregular. Which of the following best explains digoxin’s effect on heart rate in this patient?
CorrectIncorrect -
Question 25 of 37
25. Question
A 22-year-old man comes to the emergency department with abdominal pain and vomiting. His symptoms began acutely 24 hours ago with nausea and decreased appetite. His medical history is unremarkable. The patient drinks 3-4 beers a week and does not use tobacco or illicit drugs. BMI is 37 kg/m2. Physical examination is notable for moderate epigastric tenderness with decreased bowel sounds but no rebound tenderness, guarding, or abdominal rigidity. Fasting laboratory studies show a serum triglyceride concentration of 1,500 mg/dL (normal: <200 mg/dL). Once the patient has been medically stabilized, which of the following medications would be most helpful in preventing recurrences of his condition?
CorrectIncorrect -
Question 26 of 37
26. Question
A 68-year-old man reports myalgia and fatigue during a follow-up office visit. The patient has been taking high-intensity statin therapy since he had an acute myocardial infarction several weeks ago. His other medical problems include hypertension and type 2 diabetes mellitus. On examination, there is mild generalized muscle tenderness. Serum creatine kinase level is 456 U/L. Vitamin D and TSH levels are within normal range. The patient’s statin therapy is discontinued, and he is started on a medication that inhibits cholesterol absorption at the brush border of the small intestine. Which of the following drugs was most likely started in this patient?
CorrectIncorrect -
Question 27 of 37
27. Question
A 63-year-old man comes to the office for a follow-up visit. Two months ago, he was hospitalized for chest pain and was found to have a blockage in the left anterior descending artery. He had percutaneous coronary intervention with placement of a drug-eluting stent, and was discharged on appropriate medical therapy. His other medical problems include hypertension, type 2 diabetes mellitus, and degenerative joint disease. The patient has been taking all his medications as prescribed. He has no chest pain but does have diffuse muscle aches and cramps, especially after exercise. Physical examination is unremarkable. Laboratory testing reveals elevated serum creatine kinase. The medication most likely responsible for this patient’s current findings also causes which of the following effects?
CorrectIncorrect -
Question 28 of 37
28. Question
A 46-year-old man comes to the office to follow up mixed hyperlipidemia. His lipid levels have progressively worsened over the last 10 years associated with gradual weight gain. In the last 6 months, the patient has attempted to modify his diet and exercise regimen, but his lipid levels have not improved. Past medical history is unremarkable, and he currently takes no medications. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 130/86 mm Hg, pulse is 76/min, and BMI is 28 kg/m2. Cardiovascular examination is normal. Which of the following drugs, when used as monotherapy, would be most likely to increase triglyceride levels in this patient?
CorrectIncorrect -
Question 29 of 37
29. Question
A 22-year-old man comes to the office due to a 6-month history of difficulty breathing and chest discomfort on exertion. He also reports intermittent palpitations. The patient’s only other medical condition is major depression. Temperature is 37 C (98.6 F), blood pressure is 120/80 mm Hg, pulse is 82/min, and respirations are 15/min. Pulse oximetry on room air shows an oxygen saturation of 98%. BMI is 24 kg/m2. The lungs are clear on auscultation. Cardiac examination reveals a prominent left ventricular impulse on palpation, an S4, and a faint systolic murmur at the left sternal border that accentuates during the strain phase of the Valsalva maneuver. Verapamil therapy would most likely improve this patient’s dyspnea through which of the following mechanisms?
CorrectIncorrect -
Question 30 of 37
30. Question
A 56-year-old man comes to the emergency department due to palpitations and lightheadedness over the last 2 hours. He has a history of hypertension but no other cardiac conditions and never before had similar symptoms. The patient drinks 1 to 2 alcoholic beverages daily but does not smoke cigarettes or use illicit drugs. Blood pressure is 132/76 mm Hg and pulse is 116/min and irregular. Cardiopulmonary examination is normal, except for tachycardia. Resting ECG shows atrial fibrillation. The patient undergoes transesophageal echocardiography, which reveals normal cardiac anatomy and no intracardiac thrombi. Electrical cardioversion is performed. After the intervention, sinus rhythm is restored, and amiodarone therapy is begun to maintain normal sinus rhythm. Which of the following cardiac electrophysiologic changes are most likely to occur in this patient due to the medication?
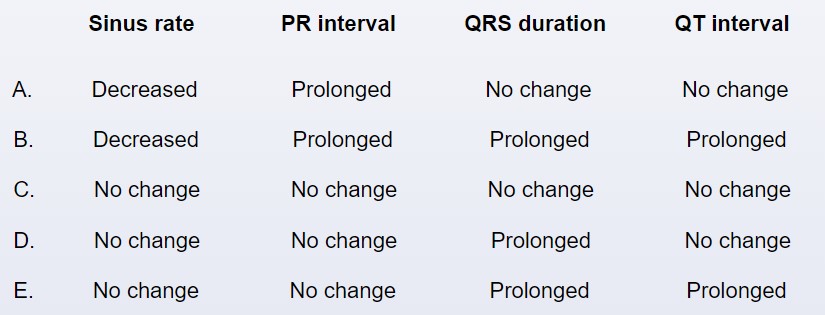 CorrectIncorrect
CorrectIncorrect -
Question 31 of 37
31. Question
A 55-year-old man comes to the emergency department due to an hour of intense substernal chest burning accompanied by sweating. He has a history of obesity and diet-controlled type 2 diabetes mellitus. On initial evaluation, blood pressure is 110/70 mm Hg and pulse is 60/min and regular. Oxygen saturation is 98% on room air. The patient is comfortable lying flat and no heart murmurs are heard. Lungs are clear on auscultation. Immediate ECG shows normal sinus rhythm with a 2-mm ST-segment elevation in leads II, III, and aVF. Aspirin and morphine are administered. As the patient is about to be transported to the catheterization lab for urgent percutaneous coronary intervention, he develops dizziness and the telemetry monitor shows sinus bradycardia at 40/min. The patient appears pale and diaphoretic and peripheral pulses are faint. Blood pressure is 70/40 mm Hg. Which of the following is the best immediate step for managing this patient’s condition?
CorrectIncorrect -
Question 32 of 37
32. Question
A 54-year-old man is evaluated for paroxysmal atrial fibrillation. During the episodes, the patient experiences palpitations, chest tightness, light-headedness, and shortness of breath. Medical history is significant for asthma, hypertension, and diet-controlled diabetes mellitus. Prior testing showed normal left ventricular ejection fraction, no evidence of valvular disease, and no obstructive coronary artery disease. It is decided to proceed with dofetilide therapy. Initiation of this therapy increases this patient’s risk for which of the following?
CorrectIncorrect -
Question 33 of 37
33. Question
A 65-year-old man is brought to the emergency department due to central chest pain for the past 2 hours. The patient describes the pain as “very severe” and “going back all the way to my spine.” He has never had similar pain. Medical history is significant for hypertension; the patient has been nonadherent with prescribed medical therapy and follow-up visits. He has a 20-pack-year smoking history. Blood pressure is 195/101 mm Hg, and pulse is 93/min and regular. Chest examination reveals clear lungs. ECG shows sinus rhythm and voltage criteria for left ventricular hypertrophy. Portable chest x-ray reveals a widened mediastinum. The patient is immediately treated with intravenous esmolol. Which of the following is the most likely purpose of this patient’s current therapy?
CorrectIncorrect -
Question 34 of 37
34. Question
A 56-year-old man comes to the hospital due to 24 hours of burning substernal chest pain. The most intense pain occurred approximately 6 hours ago, and it has started to subside. The patient has a history of diabetes mellitus. ECG shows sinus rhythm with ST-segment elevation in leads V3 to V5. In the cardiac catheterization laboratory, he is found to have total occlusion of the left anterior descending artery. Successful intervention is performed to restore blood flow in the artery. The next day, the patient’s echocardiogram shows a normal-sized left ventricle with no evidence of hypertrophy; there is apical and anterior akinesia with a reduced left ventricular ejection fraction of 38%. Which of the following is the most likely long-term effect of ACE inhibitor therapy in this patient?
CorrectIncorrect -
Question 35 of 37
35. Question
A 42-year-old man comes to the emergency department due to an episode of syncope. He was standing in his kitchen this morning when he felt palpitations for about 3 seconds; the next thing he remembers is waking up on the floor. The patient has had intermittent palpitations for the last few weeks, sometimes with associated lightheadedness. He has no significant medical history other than chronic lower back pain that began following a fall from a ladder 3 years ago. The patient fractured several lumbar vertebrae in that fall and required a surgical lumbar fusion. His back pain was uncontrolled with conservative measures, and he has been treated with escalating doses of methadone for the past year. He does not smoke or drink alcohol. The patient has a remote history of intravenous heroin abuse but has not used it for 20 years. He has no family history of early-onset heart disease, blood clots, or sudden death. Blood pressure is 120/70 mm Hg when supine and 125/75 mm Hg when standing. Physical examination is unremarkable. Which of the following ECG findings is most likely in this patient?
CorrectIncorrect -
Question 36 of 37
36. Question
An investigator studies the effects of 2 different medications on the heart rate of patients with persistent atrial fibrillation. After participants receive therapeutic doses of medication for several days, their heart rates are measured for 24 hours at rest and during 10 minutes of moderate exercise. The results are compared against placebo and shown in the graphs below. Which of the following medications is most likely represented by the red line (drug 1)?
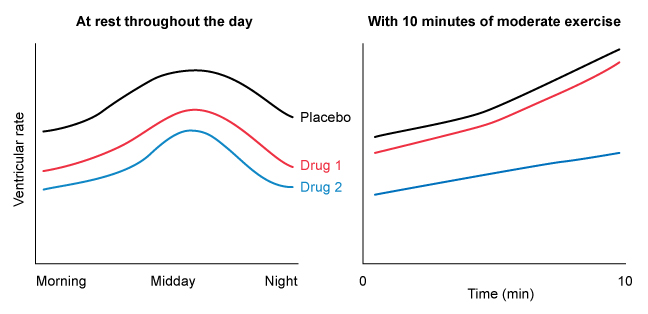 CorrectIncorrect
CorrectIncorrect -
Question 37 of 37
37. Question
A 58-year-old man with a history of hypertension and hyperlipidemia comes to the emergency department due to substernal chest pain that began 6 hours ago and has gradually worsened. Blood pressure is 104/72 mm Hg and pulse is 88/min. ECG shows normal sinus rhythm with ST-segment depression and T-wave inversion, and troponin levels are elevated. The patient is diagnosed with non–ST-segment elevation myocardial infarction and admitted to the hospital for medical management, with coronary angiography scheduled the following morning. That evening, telemetry monitoring shows a new Mobitz type 1 second-degree atrioventricular block. Which of the following arteries was most likely obstructed during this patient’s myocardial infarction?
CorrectIncorrect
