Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 31-year-old man comes to the office due to exertional shortness of breath over the last year. The patient becomes short of breath after running 1-2 miles but feels mostly fine with daily activities. He has no chest pain, palpitations, or fainting spells. The patient also has no medical history and takes no medications. There is no family history of sudden death. Blood pressure is 147/90 mm Hg and pulse is 77/min. BMI is 22 kg/m2. The apical precordial impulse is hyperdynamic. S1 and S2 are normal and an S4 is heard. The patient has a 2/6 systolic murmur at the left sternal border, which increases with standing. The lungs are clear to auscultation. Echocardiography reveals an interventricular septal thickness of 1.8 cm (normal: <1.1) and a posterior left ventricular wall thickness of 0.9 cm (normal: <1.1). Left ventricular ejection fraction is 75%. There is systolic anterior motion of the mitral valve. At rest, the peak instantaneous left ventricular outflow gradient is 25 mm Hg; however, it is 65 mm Hg after exercise. Holter monitoring for 24 hours shows no abnormalities. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
A 25-year-old woman comes to the office with a 3-month history of fatigue, myalgias, arthralgias, and a 5-kg (11-lb) weight loss. She has also recently experienced increased leg pain with physical activity, which resolves with rest. The patient has no other medical conditions and takes no medications. Temperature is 37.6 C (99.7 F), and blood pressure is 160/90 mm Hg in the right arm and 120/80 mm Hg in the left. A bruit is heard over the left subclavian artery. Left radial pulse and dorsalis pedis pulses in both legs are weak. The remainder of the examination shows no abnormalities. Laboratory results reveal a hemoglobin level of 9.8 g/dL and an erythrocyte sedimentation rate of 110 mm/hr. Which of the following pathologic mechanisms most likely underlies this patient’s current condition?
CorrectIncorrect -
Question 3 of 40
3. Question
A 52-year-old man comes to the emergency department an hour after the onset of severe substernal chest pressure that lasted 30 minutes. The symptoms started when he was helping his brother move into his new house and were associated with mild dizziness and shortness of breath. His brother has coronary artery disease with stable angina and the patient took 3 of his brother’s nitroglycerin tablets sublingually before his pain eventually subsided. He is currently pain free. Medical history includes hypertension and hyperlipidemia. The patient’s daily medications include losartan, atorvastatin, and low-dose aspirin. Blood pressure is 152/93 mm Hg and pulse is 105/min. BMI is 32 kg/m2. The lungs are clear to auscultation bilaterally. Cardiac examination indicates a prominent point of maximal impulse that is displaced downward and to the left. Auscultation reveals regular, normal heart sounds with an audible S4. There are no murmurs. The rest of the physical examination is within normal limits. ECG shows sinus tachycardia and voltage criteria for left ventricular hypertrophy, similar to the patient’s ECG 6 months ago. His troponin level is normal. He says, “I feel fine! I just want to go home and I will see my primary care doctor.” Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
A 30-year-old Asian man comes to the clinic due to painful, ulcerated fingers. His symptoms began with pain and discoloration of the fingers several weeks ago, which progressed to ulceration at the fingertips. He also reports pain in the hands that occurs with activity and is relieved by rest. Medical history is unremarkable. The patient has smoked 2 packs of cigarettes a day for the last 5 years. He occasionally drinks alcohol but does not use illicit drugs. Vital signs are within normal limits. No heart murmurs are heard and the lungs are clear. Examination of the hands is shown in the exhibit. Radial pulses are diminished. There is erythema and tenderness along a superficial vein of the left forearm. Hemoglobin A1c and a fasting lipid panel are within normal limits. Which of the following pathologic findings is most likely to be seen within the affected vessels?
 CorrectIncorrect
CorrectIncorrect -
Question 5 of 40
5. Question
A 62-year-old man comes to the office due to shortness of breath for the past 6 months. The patient, who describes his symptoms as progressive, has difficulty walking a block without becoming out of breath. He experiences chest tightness and midline “squeezing” that is relieved after 5 minutes of rest. He also has fatigue and poor sleep but no palpitations, orthopnea, cough, or syncope. His other medical problems include hypertension and gastroesophageal reflux disease. His medications are hydrochlorothiazide and famotidine. The patient has smoked a pack of cigarettes daily for 35 years and drinks 1 or 2 beers daily. His father has high blood pressure and had a stroke in his 60s, and his mother died of breast cancer. On physical examination, the patient appears comfortable at rest. Blood pressure is 136/78 mm Hg and pulse is 84/min and regular. BMI is 41 kg/m2. No cardiac murmurs are heard. The lungs are clear on auscultation. There is trace edema of the lower extremities bilaterally. Resting ECG shows normal sinus rhythm with no ST-segment or T-wave abnormalities. Exercise stress testing is performed and reveals a 1-mm ST depression in ECG leads I, aVL, V5, and V6 at minimal exertion. The patient is started on aspirin, atorvastatin, and metoprolol and counseled on smoking cessation. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
A 65-year-old man is brought to the emergency department after a syncopal episode. He was sitting at the kitchen table when his wife saw him suddenly slump over. She estimates he was unresponsive for 30 seconds. He felt “completely fine” after the incident and was not confused. The patient sustained no trauma and does not remember any symptoms prior to the event. He has a history of benign prostate hyperplasia, hypertension, and a myocardial infarction requiring stent placement 3 years ago. He takes aspirin, carvedilol, atorvastatin, ramipril, and tamsulosin. Temperature is 36.7 C (98 F), blood pressure is 130/80 mm Hg, pulse is 60/min, and respirations are 14/min. Pulse oximetry shows 96% on room air. Physical examination reveals moist mucous membranes, normal jugular venous pressure, clear lung fields, and normal first and second heart sounds. There is trace edema of the lower extremities bilaterally. Neurologic examination is within normal limits. Complete blood count, basic metabolic panel, troponin, and chest x-ray are normal. ECG reveals normal sinus rhythm, Q waves in leads V2 to V4, normal QRS complex duration, and normal QTc interval. Transthoracic echocardiogram shows an apical wall motion abnormality with ejection fraction of 40%. Which of the following is the most likely cause of this patient’s syncope?
CorrectIncorrect -
Question 7 of 40
7. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 72-year-old man comes to a rural health clinic due to intermittent leg pain. The patient reports a dull discomfort in his left lower calf with activity, causing him to stop and rest on the way to his mailbox, which is approximately 150 m (492 ft) from his house. The pain improves with rest and does not occur at night when he is lying in bed. Medical history is significant for hypertension and gout. Current medications include lisinopril and allopurinol. The patient has a 40-pack-year smoking history, but quit 5 years ago. Family history is significant for a stroke in his father and breast cancer in his mother. Blood pressure is 130/78 mm Hg and pulse is 75/min. The patient’s left foot is shiny and devoid of hair, but there are no lower extremity ulcerations. Strength and sensory examination of the left lower extremity is normal. The ankle-brachial index is 0.76 on the left and 1.05 on the right (normal: 1.0-1.4). Laboratory results are as follows:
Creatinine
1.0 mg/dL
Glucose
101 mg/dL
Total cholesterol
155 mg/dL
Low-density lipoprotein
93 mg/dL
High-density lipoprotein
58 mg/dL
Triglycerides
120 mg/dL
Alanine aminotransferase (SGPT)
25 U/L
Item 1 of 2
In addition to aspirin, which of the following medications is the most appropriate to add to this patient’s pharmacologic regimen?
CorrectIncorrect -
Question 8 of 40
8. Question
Item 2 of 2
Following medication adjustment, the patient is sent for CT angiography that shows 90% stenosis of the left superficial femoral artery and 80% stenosis of the left popliteal artery. Which of the following is the best additional recommendation for this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 62-year-old Caucasian man comes to the emergency department (ED) and complains of crushing substernal chest pain. The pain started one hour ago while he was shoveling snow on his driveway. At the onset of his pain, he took nitroglycerin sublingually, but the pain did not get any better and he was taken to the ED by his son. He has a history of coronary artery disease, hypertension, hyperlipidemia, and osteoarthritis. He is on daily aspirin, metoprolol, lisinopril, atorvastatin, and naproxen as needed. In the ED, his electrocardiogram reveals a normal sinus rhythm with no acute ST-T wave changes. He is given morphine for his pain, started on nitroglycerin drip, and admitted to the telemetry floor. The next day, an adenosine thallium stress test reveals a moderate size reversible perfusion defect in the lateral wall of the left ventricle. Which of the following coronary vessels is most likely to have a significant occlusion?
CorrectIncorrect -
Question 10 of 40
10. Question
A 66-year-old woman with systolic left ventricular dysfunction comes to the emergency department due to dizziness, palpitations, and shortness of breath. The symptoms started 2 days ago and have become progressively worse. Her cardiologist prescribed an extra dose of oral furosemide yesterday, but her symptoms did not improve. Six weeks ago, she was admitted for acute decompensated heart failure that was thought to be precipitated by atrial fibrillation. The patient underwent electrical cardioversion and was diuresed with marked symptomatic improvement. She has a history of atrial fibrillation, hypertension, type 2 diabetes mellitus, coronary artery disease, ischemic cardiomyopathy with a 30% ejection fraction, and osteoarthritis. She underwent coronary artery bypass grafting 5 years ago. Her current medications include low-dose aspirin, metoprolol, lisinopril, rosuvastatin, long-acting insulin, rivaroxaban, furosemide, and ibuprofen as needed. The patient has been adherent to her medical regimen. She does not use tobacco or alcohol. Temperature is 36.7 C (98 F), blood pressure is 126/82 mm Hg, pulse is 132/min and irregular, and respirations are 19/min. Physical examination reveals bibasilar crackles on auscultation. There are irregularly irregular heart sounds with no audible murmurs. There is 1+ symmetric peripheral edema. ECG shows atrial fibrillation with rapid ventricular response. Serum creatinine level is 0.8 mg/dL. After initial treatment, electrical cardioversion is planned. Which of the following is the most appropriate medication for long-term management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 72-year-old man with diet-controlled diabetes mellitus comes to the emergency department due to chest pain for the past 4 hours. He has never had similar pain. The pain is accompanied by nausea and epigastric discomfort. ECG shows normal sinus rhythm and ST-segment elevations in leads II, III, and aVF. Sublingual nitroglycerin and intravenous morphine are administered, and the on-call interventional cardiologist is informed. Several minutes later, the patient says he feels lightheaded, nauseated, and weak. Blood pressure is 75/52 mm Hg, pulse is 60/min, and respirations are 15/min. The patient is diaphoretic, and his extremities are cold. The lungs are clear on auscultation, and no murmurs are heard on cardiac auscultation. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 12 of 40
12. Question
A 48-year-old woman is brought to the emergency department due to chest discomfort. She describes a pressure-like sensation behind the sternum lasting several hours. Yesterday, the patient was brought to the emergency department after a front-end motor vehicle collision in which she was a restrained passenger. She was assessed to have minor injuries and was discharged home. Her husband, who sustained a head injury in the collision, is in the hospital. The patient has hyperlipidemia and her only medication is an estrogen-containing oral contraceptive. Blood pressure is 135/90 mm Hg and pulse is 102/min and regular. Oxygen saturation is 99% on room air. BMI is 31 kg/m2. The lungs are clear on auscultation. ECG shows sinus tachycardia with 1-mm ST-segment elevation in leads V3 to V6. The QTc interval is 509 msec. Cardiac catheterization shows normal coronary arteries. Echocardiography is most likely to demonstrate which of the following?
CorrectIncorrect -
Question 13 of 40
13. Question
The following vignette applies to the next 2 items
A 3-week-old male infant with Down’s syndrome is brought by his parents to your office due to feeding difficulties. According to the mother, the infant becomes short of breath and his face turns blue during feeding, and when he cries. On chest auscultation, there is a harsh holosystolic murmur heard best over the lower left sternal border. There are no rales or wheezing over the lung fields.
Item 1 of 2
Which of the following is the most useful test for diagnostic evaluation?
CorrectIncorrect -
Question 14 of 40
14. Question
Item 2 of 2
In the long run, this infant is at increased risk of developing which of the following?
CorrectIncorrect -
Question 15 of 40
15. Question
A 38-year-old woman comes to the physician for a routine checkup. She has no current complaints. The patient’s past medical history is significant for hypertension and type 2 diabetes mellitus. Her medications include low-dose hydrochlorothiazide, lisinopril, metformin, and glyburide. She smokes 1/2 pack of cigarettes daily and drinks alcohol occasionally. Her last menstrual period was 2 weeks ago. Blood pressure is 130/85 mm Hg and pulse is 85/min. The patient’s body mass index is 32 kg/m2. The remainder of the physical examination is within normal limits. Her fasting blood glucose is 120 mg/dL and HbA1C level is 6.7%. Which of the following factors is the most significant predictor of future cardiovascular events in this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 27-year-old woman is brought to the emergency department due to a 4-hour history of chest pain that is localized to the middle of the chest and the upper sternal area. She describes it as “intense.” The patient has never before experienced a similar pain. She also describes some nausea and a mild occipital headache. She has had no vomiting, abdominal pain, or shortness of breath. A friend who accompanies her to the emergency department says that they attended a party and the patient smoked crack cocaine shortly prior to her episode of chest pain. She did not consume alcohol. The patient has a history of intravenous drug use. She was treated with antibiotics for upper extremity cellulitis 6 months ago. There is no family history of premature coronary artery disease. The patient does not take any medications and has no known drug allergies. On initial evaluation, temperature is 37.8 C (100 F), blood pressure is 204/102 mm Hg on the right arm and 210/104 mm Hg on the left arm, pulse is 102/min and regular, and respirations are 18/min. Oxygen saturation is 99% on room air. The patient appears thin, anxious, and agitated. Heart sounds are normal and no murmurs are heard. Lungs are clear to auscultation bilaterally. The abdomen is soft and nontender. Lower extremity pulses are full and symmetric. There is no peripheral edema. ECG shows sinus tachycardia but is otherwise unremarkable. Portable chest x-ray reveals clear lung fields. Finger-stick blood glucose level is 98 mg/dL.
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
Item 2 of 2
After 2 hours in the emergency department, the patient develops weakness in her right arm. Her chest pain is slightly improved, but still present at the middle and upper part of the sternum. She has been treated with lorazepam, morphine, and nitroglycerin infusion. Blood pressure is 133/80 mm Hg and pulse is 88/min and regular. Neurologic examination shows mild muscle weakness affecting the right upper and right lower extremities. Speech is normal. Repeat ECG shows normal sinus rhythm with no significant abnormalities. Laboratory results are as follows:
Leukocytes
11,000/mm3
Hemoglobin
12.2 g/dL
Platelets
220,000/mm3
Sodium
134 mEq/L
Potassium
4.1 mEq/L
Creatinine
0.8 mg/dL
Troponin
undetectable
Immediate noncontrast CT scan of the head reveals no evidence of bleeding. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 18 of 40
18. Question
A 21-year-old man is seen in the clinic for a routine checkup. He is a cyclist and was asked by his trainer to see a physician due to a “slow heartbeat.” The patient describes intense physical activity in preparation for tournaments and has no symptoms. Specifically, he has no chest pain, shortness of breath, lightheadedness, presyncope, or syncope. His family history is unremarkable. He does not take any medications or use performance-enhancing drugs. Blood pressure is 123/72 mm Hg and pulse is 46/min. No cardiac murmurs are heard in the supine or upright positions. There are no additional heart sounds. The lungs are clear on auscultation. Pulses are full and symmetric, and there is no peripheral edema. ECG shows sinus bradycardia at 48/min. The PR interval is prolonged at 250 msec, consistent with first-degree atrioventricular block. QRS complexes are normal with no repolarization abnormalities, and QTc interval duration is normal at 400 msec. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
A 60-year-old man is brought to the emergency department due to acute-onset shortness of breath. He has no chest pain. Medical history is significant for hypertension, coronary artery disease, and type 2 diabetes mellitus. Temperature is 36.7 C (98 F), blood pressure is 128/72 mm Hg, pulse is 116/min, and respirations are 28/min. On physical examination, the patient appears anxious and is diaphoretic. Jugular venous pressure is elevated to the angle of the jaw. Heart sounds are regular, and an S3 gallop is heard over the cardiac apex. Auscultation of the lungs reveals crackles to the midlung level bilaterally. Pitting edema is noted in both lower extremities. Which of the following is the best initial approach in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 56-year-old man comes to the emergency department due to palpitations and lightheadedness over the last 2 hours. He has a history of hypertension but no other cardiac conditions and never before had similar symptoms. The patient drinks 1 to 2 alcoholic beverages daily but does not smoke cigarettes or use illicit drugs. Blood pressure is 132/76 mm Hg and pulse is 116/min and irregular. Cardiopulmonary examination is normal, except for tachycardia. Resting ECG shows atrial fibrillation. The patient undergoes transesophageal echocardiography, which reveals normal cardiac anatomy and no intracardiac thrombi. Electrical cardioversion is performed. After the intervention, sinus rhythm is restored, and amiodarone therapy is begun to maintain normal sinus rhythm. Which of the following cardiac electrophysiologic changes are most likely to occur in this patient due to the medication?
 CorrectIncorrect
CorrectIncorrect -
Question 21 of 40
21. Question
A 72-year-old man comes to the office due to palpitations, fatigue, and dyspnea for the past 2 weeks. The patient experienced an episode of atrial fibrillation 4 years ago during hospitalization for pneumonia; the episode spontaneously resolved 2 days later. Since then, he has had 3 episodes of symptomatic atrial fibrillation that self-terminated within a week. Other medical history includes hypertension, type 2 diabetes mellitus, and chronic heart failure. Blood pressure is 130/84 mm Hg and pulse is 110/min. The lungs are clear to auscultation. Cardiac examination demonstrates tachycardia with irregularly irregular heartbeats. ECG confirms atrial fibrillation. The patient’s ventricular rate is controlled with beta blocker therapy, but the arrhythmia fails to resolve as in previous episodes. Which of the following factors is most likely involved in the progression of this patient’s arrhythmia?
CorrectIncorrect -
Question 22 of 40
22. Question
A 74-year-old woman is admitted to the hospital for an episode of paroxysmal atrial fibrillation that caused palpitations and dizziness. She is started on metoprolol and amiodarone. Her past medical history is also significant for recurrent deep venous thrombosis 6 months ago. The patient has been on chronic anticoagulation therapy with a stable dose of warfarin since then. Her primary care physician checks her International Normalized Ratio every month; it is 2.6 at the time of admission. Echocardiogram shows left atrial enlargement and left ventricular ejection fraction of 45%. She feels well the following day and is ready for discharge. Which of the following is the best management for this patient’s anticoagulation?
CorrectIncorrect -
Question 23 of 40
23. Question
A 47-year-old man is brought to the emergency department 20 minutes after being struck by lightning. The patient was playing soccer when a thunderstorm suddenly developed; he was struck by cloud-to-ground lightning and thrown several feet. Other players realized the patient was in cardiac arrest and initiated chest compressions immediately. Paramedics arrived within 5 minutes and continued resuscitation using advanced cardiovascular life support guidelines. In the emergency department, the patient has no spontaneous pulse or respiration. The pupils are dilated and unresponsive to light. The electrical rhythm on the monitor is asystole. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 24 of 40
24. Question
A 22-year-old man comes to the clinic due to frequent headaches. He plays football on weekends but over the last 3 months has noticed a dry cough and decreased exercise tolerance due to shortness of breath. The patient has also had lower extremity swelling and says that his face feels “puffy.” He is a lifetime nonsmoker and does not use alcohol or illicit drugs. The patient’s mother was diagnosed with hypertension at age 45 and takes 2 antihypertensive medications; his father is healthy. The patient has no siblings. Blood pressure is 180/102 mm Hg in the right arm and 183/99 mm Hg in the left and pulse is 85/min and regular. BMI is 24 kg/m2. Upper and lower extremity pulses are equal. Bilateral lower extremity edema is present. The remainder of the physical examination is normal. ECG shows normal sinus rhythm. Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 25 of 40
25. Question
A 34-year-old man with no significant medical history comes to the office due to dyspnea and chest pain with exertion. The patient reports that the symptoms began 6 months ago, typically occurring during his morning jog and resolving after he stops to rest for a few minutes. He has had no cough, orthopnea, paroxysmal nocturnal dyspnea, or syncope. Family history is remarkable for the sudden death of his uncle while playing basketball at age 26. Temperature is 37 C (98.6 F), blood pressure is 120/78 mm Hg, and pulse is 72/min. Physical examination shows a 2/6 systolic murmur that increases in intensity with standing. ECG reveals left ventricular (LV) hypertrophy with lateral T-wave inversions. Echocardiography demonstrates small LV cavity size with LV wall thickening most prominent at the interventricular septum; resting LV outflow tract gradient is 30 mm Hg and ejection fraction is 65%. Twenty-four-hour Holter monitor shows occasional premature ventricular contractions with no other abnormalities. Which of the following is the strongest indication for placement of an implantable cardioverter-defibrillator in this patient?
CorrectIncorrect -
Question 26 of 40
26. Question
The following vignette applies to the next 2 items.
A 72-year-old man comes to the emergency department due to progressive shortness of breath and cough productive of yellowish sputum. The patient says, “I have been feeling breathless for the past several months while mowing the lawn or walking around the house, but it has been worse over the last 3 days.” He has had no chest pain or leg swelling but notes that his heart “has been racing.” The patient has a history of hypertension, peptic ulcer disease, and osteoarthritis. He was hospitalized for pneumonia a year ago and required intravenous antibiotics. Six months ago, the patient underwent a cardiac stress test for chest discomfort, which was unremarkable. The patient has smoked a pack of cigarettes daily for 45 years. Blood pressure is 160/90 mm Hg, pulse is 148/min, and respirations are 26/min. He is speaking in partial sentences and using accessory muscles of respiration but is alert and cooperative. There is no jugular venous distension or heart murmurs, rub, or gallops, but the heart sounds are irregular. Lung auscultation reveals bilateral rhonchi and expiratory wheezes. Arterial blood gases while breathing 2 L of oxygen via nasal cannula reveal PO2 of 66 mm Hg, PCO2 of 52 mm Hg, and pH 7.33. ECG shows narrow QRS complexes with distinct P waves of different morphologies and variable PR segments and R-R intervals. Chest x-ray reveals no pulmonary infiltrates or consolidation. Inhaled bronchodilators and systemic glucocorticoids are administered.
Item 1 of 2
Which of the following is the most appropriate additional step in management of this patient’s arrhythmia?
CorrectIncorrect -
Question 27 of 40
27. Question
Item 2 of 2
The patient’s dyspnea has improved after initial treatment in the emergency department, but he continues to have palpitations. Pulse is 125/min and irregular. Blood pressure is 140/88 mm Hg and respirations are 16/min. Oxygen saturation is 92% on 2 L oxygen via nasal cannula. ECG findings are unchanged from the time of admission. Laboratory results are as follows:
Complete blood count
Leukocytes
7,000/mm3
Hematocrit
50%
Platelets
320,000/mm3
Serum Chemistry
Sodium
125 mEq/L
Potassium
3.1 mEq/L
Chloride
80 mEq/L
Bicarbonate
33 mEq/L
Blood urea nitrogen
25 mg/dL
Creatinine
1.2 mg/dL
Calcium
10.1 mg/dL
Glucose
84 mg/dL
Magnesium
2.0 mEq/L
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 56-year-old man comes to the physician for an initial evaluation. He reports tiredness and decreased exercise tolerance over the past few weeks. He feels “out of breath” when he goes ballroom dancing with his wife, which has been a regular activity for them. He has not had any cough, orthopnea, wheezing, and lower extremity edema. The patient’s other medical problems include gastroesophageal reflux disease. Approximately a month ago he had a particularly severe episode of burning in the upper abdomen and chest, but he has not noted any dark stools or blood in the stool. He takes famotidine intermittently and uses ibuprofen periodically for pain in his left knee but is not taking any regular medications. He has a 30-pack-year smoking history and drinks 1-2 beers per night. The patient’s mother had diabetes mellitus and died of a stroke. His father died of colon cancer. His blood pressure is 144/89 mm Hg and pulse is 94/min and regular. BMI is 32 kg/m2. Examination shows normal jugular venous pressure and clear lungs. First and second heart sounds are normal. Deep palpation in the epigastric region elicits mild tenderness. Laboratory results are as follows:
Hemoglobin
12.2 g/dL
Mean corpuscular volume
82 μm3
Hemoglobin A1c
6.9%
Creatinine
1.5 mg/dL
Total cholesterol
251
Triglycerides
441
HDL
31
LDL
Calculation not performed
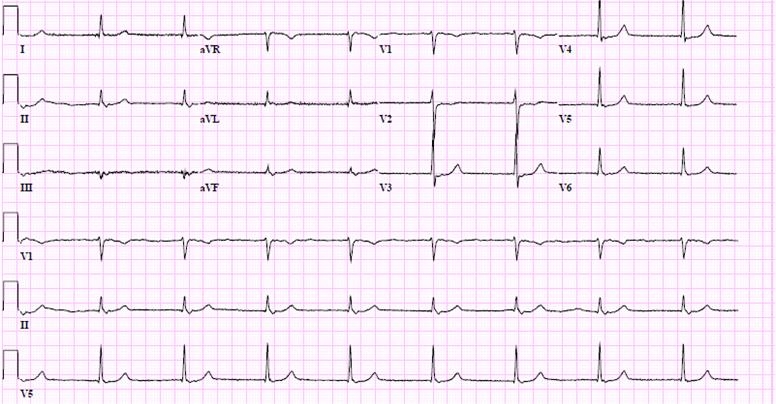
ECG is shown in the exhibit. Which of the following is the most appropriate next step in pharmacotherapy?
 CorrectIncorrect
CorrectIncorrect -
Question 29 of 40
29. Question
A 43-year-old, previously healthy woman is brought to the emergency department in severe respiratory distress. The patient’s shortness of breath began 2 days ago and has progressively worsened. Over the past 6 months she has had insomnia, loose stools, and lightheadedness. Temperature is 37.2 C (98.9 F), blood pressure is 166/90 mm Hg, pulse is 114/min, and respirations are 30/min. Pulse oximetry is 86% on nonrebreather mask. Examination shows marked respiratory distress with intercostal and supraclavicular retractions. The skin is diaphoretic and warm. Cardiopulmonary examination reveals diffuse rales, an S3, and a 2/6 systolic ejection murmur over the left sternal border. The extremities have 1+ pitting edema bilaterally. The patient is placed on positive airway pressure ventilation with improvement in oxygen saturation to 94%. ECG shows sinus tachycardia. Chest x-ray reveals a mildly enlarged cardiac silhouette with evidence of pulmonary congestion. Echocardiography shows pulmonary hypertension, left atrial enlargement, and a left ventricular ejection fraction of 75%; there are no wall motion abnormalities. Troponin I is 0.06 ng/mL (normal: <0.04 ng/mL). Which of the following will be most helpful in the diagnosis of this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 63-year-old man with hypertension comes to the clinic for follow-up. He was last seen a year ago and has been maintained on amlodipine for the past 3 years. The patient has no symptoms and describes good exercise tolerance. He takes rosuvastatin for hyperlipidemia. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 132/78 mm Hg, and pulse is 82/min and regular. Oxygen saturation is 99%. Examination reveals a 2/6 ejection-type systolic murmur at the right second intercostal space. The patient’s lungs are clear, and there is no peripheral edema. ECG shows normal sinus rhythm with nonspecific T wave abnormalities. He is referred for an echocardiogram, which reveals mild aortic sclerosis and left ventricular dilation with an ejection fraction of 35%. There are no regional wall motion abnormalities. Cardiac stress test is negative for ischemia. Which of the following is the best management for this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 42-year-old woman is brought to the emergency department by paramedics for evaluation of a day of mental status changes. She has a history of hypothyroidism, major depression, and chronic back pain. Her medications include levothyroxine, amitriptyline, and daily oxycodone. The patient is markedly confused and agitated and talks to herself. Her temperature is 38.9 C (102 F), blood pressure is 92/52 mm Hg, pulse is 110/min, and respirations are 22/min. There is marked flushing, mydriasis, and hyperreflexia. Her electrocardiogram shows sinus tachycardia with a wide QRS interval. She is started on sodium bicarbonate infusion. Which of the following is the primary therapeutic goal of sodium bicarbonate in this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 28-year-old woman comes to the office due to exertional dyspnea for the last 2 weeks. She has a history of rheumatic mitral stenosis with an estimated mitral valve area of 1.5 cm2, which was documented on her most recent echocardiogram 4 months ago. The patient’s exercise tolerance is about 5 blocks of brisk walking at baseline but is currently about 1 block. She has had no recent upper respiratory infection, sore throat, cough, hemoptysis, orthopnea, lower extremity pain or swelling, palpitations, syncope, or chest pain. Medical history is otherwise unremarkable, and she takes no medications. The patient does not use tobacco or alcohol and lives with her husband. Blood pressure is 108/67 mm Hg, and pulse is 92/min and regular. A diastolic rumble is heard at the apex in the left lateral decubitus position. The lungs are clear on auscultation. Which of the following is the best next step in evaluation of this patient’s symptoms?
CorrectIncorrect -
Question 33 of 40
33. Question
A 62-year-old woman comes to the physician due to lower extremity edema. She has never had such edema before. She has no dyspnea, cough, or palpitations. Her concurrent medical problems include hypertension, type 2 diabetes mellitus, and chronic bronchitis. She smokes 1.5 packs of cigarettes a day but does not use alcohol or illicit drugs. She brings in a shopping bag of medications, including a variety of antihypertensive and antidiabetic medications, but is uncertain which ones she takes and which she does not. Her blood pressure is 140/90 mm Hg and pulse is 65/min. Physical examination shows symmetric lower extremity edema but is otherwise unremarkable. Which of the following is the most likely potential cause of this patient’s condition?
CorrectIncorrect -
Question 34 of 40
34. Question
A 72-year-old man is referred for preoperative evaluation for abdominal aortic aneurysm repair. He has had no chest pain, palpitations, shortness of breath, or syncope. The aneurysm was initially identified on routine screening when the patient was age 65. Since then, he has undergone yearly surveillance ultrasounds. The most recent study demonstrated an aneurysm with a diameter of 5.5 cm, an increase of 4 mm from the measurement at the ultrasound performed a year prior. He is not a candidate for minimally invasive endovascular stent graft repair due to the juxtarenal location of the aneurysm and need for left renal artery reimplantation. The patient has a history of hypertension, hyperlipidemia, type 2 diabetes mellitus, and mild aortic stenosis. Medications include aspirin, valsartan, amlodipine, high-intensity atorvastatin, metformin, and long-acting insulin. He is a former smoker but quit 15 years ago when he was diagnosed with diabetes. He does not drink alcohol and has no history of illicit drug use. The patient reports no difficulty with managing his activities of daily living, including briskly climbing up and down stairs in his 2-story home. A younger brother recently underwent coronary artery bypass graft surgery. Temperature is 36.7 C (98 F), blood pressure is 142/80 mm Hg, pulse is 70/min, and respirations are 14/min. Pulse oximetry shows 99% on room air. Weight is 100 kg (220.5 lb) and height is 177.5 cm (5 ft 10 in). BMI is 30 kg/m2. Examination shows normal jugular venous pressure. Carotid pulses are 2+ and brisk bilaterally. The lungs are clear. On cardiac auscultation, S1 and S2 are normal and there is a soft midpeaking systolic murmur. A pulsatile mass is palpable on abdominal examination. There is trace pretibial edema bilaterally. On preoperative laboratory testing, the complete blood count is within normal limits. Glucose is 156 mg/dL and creatinine is 1.3 mg/dL. ECG shows normal sinus rhythm with nonspecific T-wave changes. Chest x-ray demonstrates a tortuous thoracic aorta but is otherwise normal. Which of the following is the most appropriate course of action?
CorrectIncorrect -
Question 35 of 40
35. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 55-year-old man comes to the emergency department due to sudden onset of retrosternal chest pain. The pain began 10 hours ago and has been mostly constant, although he describes it as “being bad and then getting a little better.” The patient has had no lightheadedness, syncope, or shortness of breath. ECG shows normal sinus rhythm with 2-mm ST-segment elevation in leads V2 to V5. He is taken emergently for cardiac catheterization and undergoes percutaneous coronary intervention with stent placement to the left anterior descending artery. After the procedure, the ST-segment changes improve and he has complete resolution of the chest pain. On the third night, just prior to discharge, he calls for the nurse due to the sudden onset of sharp, retrosternal chest pain. The patient first noticed the pain while turning around in bed; it worsens with deep breathing. Temperature is 37.8 C (100 F), blood pressure is 134/80 mm Hg, heart rate is 108/min, and respirations are 22/min. Physical examination reveals regular heart sounds and clear lung fields. There is a scratchy sound heard during ventricular systole along the left sternal border. Abdominal palpation reveals no localized tenderness. ECG shows sinus tachycardia with Q waves and T-wave inversion in leads V2 to V5.
Item 1 of 2
Which of the following is the most likely cause of this patient’s recurrent symptoms?
CorrectIncorrect -
Question 36 of 40
36. Question
Item 2 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
A 72-year-old man with a history of type 2 diabetes mellitus, hypertension, chronic kidney disease, and heart failure comes to the office to establish care after moving to a new city to be nearer to family. The patient’s conditions are treated with multiple medications, and he had previously been followed by a cardiologist and nephrologist. He can walk several blocks before becoming short of breath but is asymptomatic at rest. The patient eats at a local steakhouse at least once a month. He expresses sadness and isolation due to his declining physical condition but states that he looks forward to now being nearer to his daughter and grandchildren. His last echocardiography, performed a year ago during a brief hospitalization for heart failure, revealed an ejection fraction of 37%. Physical examination is notable for 1+ pedal edema, mild jugular venous distension, and occasional lung crackles. In addition to refilling of medications and arrangement for appropriate referrals and follow-up, which of the following strategies is most effective in reducing hospitalizations due to heart failure in this patient?
CorrectIncorrect -
Question 38 of 40
38. Question
A 63-year-old man comes to the emergency department due to chest pain that occurred 2 hours ago when he was shopping for groceries. The patient experienced left-sided chest discomfort that was dull in nature and lasted 15 minutes. He had no shortness of breath, diaphoresis, palpitations, or lightheadedness. He has had no previous chest pain other than a similar episode 2 days ago when he was at home washing dishes. The pain at that time lasted 10 minutes and resolved spontaneously. The patient has hypertension and takes valsartan and amlodipine. Medical history also includes gout, peptic ulcer disease, kidney stones, and severe osteoarthritis of the right knee. He was offered knee replacement 2 years ago but refused. The patient walks with a cane. He has no known drug allergies. He is a lifetime nonsmoker. His father had a myocardial infarction at age 53 and his younger brother is healthy. The patient appears comfortable and has no complaints. Blood pressure is 147/90 mm Hg, and pulse is 82/min and regular. He has no heart murmurs or additional sounds. There are no carotid bruits. The lungs are clear on auscultation. There is no peripheral edema. ECG shows normal sinus rhythm without repolarization changes. Complete blood count and basic metabolic panel are unremarkable. Chest x-ray is normal. Two sets of cardiac troponin I drawn 4 hours apart are undetectable. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 57-year-old man with a history of coronary artery disease is brought to the emergency department due to dizziness and unsteadiness while standing. The patient had an episode of syncope 2 hours ago. He has had no chest pain, shortness of breath, nausea, vomiting, or diaphoresis. Medical history includes hypertension, hyperlipidemia, asthma, and chronic kidney disease. The patient had a stent placed in his left circumflex artery 3 years ago. He was hospitalized for pneumonia 6 months ago. Medications include atenolol, lisinopril, aspirin, atorvastatin, amlodipine, and fluticasone inhaler. The patient’s dose of atenolol was increased recently due to occasional palpitations. He uses an albuterol inhaler before exercise and is a former smoker with a 25 pack-year history. ECG in the emergency department is shown in the exhibit. Which of the following is most appropriate in the treatment for this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 40 of 40
40. Question
A 44-year-old woman comes to the emergency department due to sudden-onset dyspnea and palpitations. The patient does not have chest pain but feels her heart pounding in her chest. She is otherwise healthy and does not have any other medical conditions. The patient’s maternal uncle died suddenly at age 42. Blood pressure is 110/60 mm Hg and pulse is 170/min. Lungs are clear to auscultation. Cardiac examination is notable for a rapid heart rate but is otherwise unremarkable. ECG rhythm strip is shown in the exhibit. Which of the following is the best next step in management?
 CorrectIncorrect
CorrectIncorrect
