Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 2 items.
A 52-year-old woman comes to the emergency department with left leg pain and swelling. She is a commercial truck driver and first noticed the swelling 3 days ago. The patient initially attributed the swelling to a long haul truck ride as she often gets mild “puffiness” of her ankles by the end of the day. However, the swelling has persisted and now involves her entire left leg below the knee. She has discomfort with walking but no chest pain, palpitations, syncope, or difficulty breathing. The patient has a history of hypothyroidism and hypertension and takes levothyroxine and hydrochlorothiazide. She has also been on menopausal hormone therapy using estrogen-progestin for intractable hot flashes. She smokes a pack of cigarettes daily and drinks 2 beers each night. Temperature is 37.2 C (99 F), blood pressure is 134/89 mm Hg, and pulse is 78/min. BMI is 31 kg/m2. Extremity examination reveals a normal right leg and pitting edema and warmth over the left lower leg. ECG shows normal sinus rhythm, and chest x-ray is normal with no infiltrates. Serum creatinine level is 0.7 mg/dL. Duplex ultrasound of the lower extremities reveals noncompressibility of the left popliteal and femoral veins.
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 2
The patient is started on rivaroxaban and scheduled to follow up with her primary care physician. She is counseled on smoking cessation and agrees to enroll in a smoking cessation clinic. The patient is also informed that her current menopausal hormone therapy (MHT) increases her risk of venous thromboembolism. She is concerned about experiencing hot flashes again. Which of the following is the most appropriate recommendation for treatment of this patient’s menopausal symptoms?
CorrectIncorrect -
Question 3 of 40
3. Question
A 32-year-old woman is brought to the emergency department after she passed out at a local bank. The patient had been standing in line for a long time when she felt warm and nauseated and then lost consciousness for a few seconds. She quickly returned to normal. Her friend, who witnessed the episode, saw no abnormal, jerky movements of the extremities. Toward the end of her usual 5-mile run earlier this morning, the patient felt slightly light-headed. She has no known medical conditions. Family history is significant for a paternal uncle who died from a “heart attack” at age 55. Supine blood pressure is 110/70 mm Hg and pulse is 75/min. Two minutes after the patient stands, blood pressure is 108/70 mm Hg and pulse is 88/min. No jugular venous distension is noted. There are no heart murmurs. An S3 is present. Peripheral pulses are full and symmetric. ECG shows normal sinus rhythm with T-wave inversion in lead V1. Chest x-ray reveals a normal heart size. Which of the following is most closely associated with this patient’s likely cause of syncope?
CorrectIncorrect -
Question 4 of 40
4. Question
A 62-year-old man with recently diagnosed diffuse large B-cell lymphoma is admitted to the hospital for chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisone plus rituximab (R-CHOP). Medical history also includes hypertension, type 2 diabetes mellitus, coronary artery disease, and heart failure with reduced ejection fraction. Pretreatment evaluation shows normal renal function, liver function, and uric acid levels. Echocardiography reveals a left ventricular ejection fraction of 45%. Intravenous fluids and allopurinol are administered prior to chemotherapy. After receiving chemotherapy, the patient experiences mild nausea that resolves with antiemetics. The next morning, he reports dyspnea and lightheadedness and becomes unresponsive with a loss of pulse while being evaluated. Electrocardiographic monitoring just prior to cardiac arrest is shown in the exhibit. Which of the following most likely directly contributed to this patient’s cardiac arrest?
 CorrectIncorrect
CorrectIncorrect -
Question 5 of 40
5. Question
A 25-year-old man comes to the emergency department due to a sudden onset of left foot pain. The pain started suddenly an hour ago, when he was sitting at his desk, and has progressed gradually. He has no history of similar episodes or recent trauma to his left leg. On review of systems, the patient admits to tiredness and some weight loss over the last 2 months, which he attributes to stress. He has no significant medical history. He is a college student. The patient does not use tobacco, alcohol, or illicit drugs. His mother was diagnosed with “a blood clot” after elective knee-replacement surgery. Temperature is 37.2 C (99 F), blood pressure is 122/81 mm Hg, pulse is 86/min, and respirations are 14/min. Examination shows clear lung fields and a regular rhythm, with a low-pitched diastolic murmur over the cardiac apex. The abdomen is soft and nontender, with no palpable masses. Examination of the extremities reveals adequate bilateral femoral pulses. The left popliteal and dorsalis pedis pulses are absent. The left foot appears pale and is cooler than the right. Sensations on the left foot are intact, and the patient is able to voluntarily move the limb. There is no tenderness on palpation of the lower left leg or foot. Neurologic examination is within normal limits. Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 6 of 40
6. Question
A 34-year-old woman comes to the office due to intermittent palpitations for 2 weeks. The patient has no chest pain or shortness of breath. She was diagnosed with hypertrophic cardiomyopathy 10 years ago and hypothyroidism 5 years ago. The patient takes metoprolol and levothyroxine. Temperature is 37.1 C (98.8 F), blood pressure is 120/80 mm Hg, pulse is 65/min and regular, and respirations are 15/min. BMI is 27 kg/m2. Oxygen saturation is 98% on room air. Mucous membranes are moist. Jugular venous pressure is normal. The thyroid gland is symmetrically enlarged and nontender. The lungs are clear to auscultation. A grade 2/6 systolic murmur is heard best at the left sternal border. Complete blood count and serum chemistries are normal. Serum TSH concentration is 1.4 μU/mL. ECG shows normal sinus rhythm with T-wave inversions in the anterior leads, unchanged from 6 months ago. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
A 74-year-old man is brought to the emergency department after being involved in a major motor vehicle collision. According to the report from paramedics, he was a restrained passenger. The patient has superficial injuries to the lower extremities and blunt chest trauma. He has pain “all over” but is answering all questions appropriately. Initial blood pressure is 98/65 mm Hg, pulse is 105/min, and respirations are 18/min. Oxygen saturation is 100% on 40% oxygen via face mask. Examination shows some bruises over the anterior chest, clear lungs, and no murmurs or abnormal heart sounds. The abdomen is soft and nontender. Which of the following is the most appropriate next step in evaluation of this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
A 56-year-old woman comes to the emergency department due to 3 days of fever, chills, and retrosternal chest pain. She has end-stage kidney disease related to previous uncontrolled hypertension and receives intermittent hemodialysis through a tunneled catheter. Temperature is 39 C (102.2 F), blood pressure is 108/64 mm Hg, and pulse is 120/min. The patient is ill-appearing. The lungs are clear to auscultation, but a pericardial friction rub is present. Echocardiography reveals a moderate-sized pericardial effusion. Pericardiocentesis yields turbid fluid with a large number of neutrophils. Microbiologic analysis of this patient’s pericardial fluid is most likely to reveal which of the following pathogens?
CorrectIncorrect -
Question 9 of 40
9. Question
A 62-year-old man comes to the emergency department due to shortness of breath that started 2 days ago and has significantly worsened over the past several hours. He had to sleep in a recliner last night because he was unable to breathe while lying flat. In addition, the patient reports significant weight gain, abdominal distension, and lower extremity swelling. Medical history is significant for type 2 diabetes mellitus, obstructive sleep apnea, coronary artery disease, and heart failure with reduced ejection fraction. He was admitted to the hospital a year ago for treatment of heart failure. Blood pressure is 130/80 mm Hg and pulse is 90/min and regular. Which of the following has the highest specificity for determining the most likely diagnosis in this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
The following vignette applies to the next 3 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
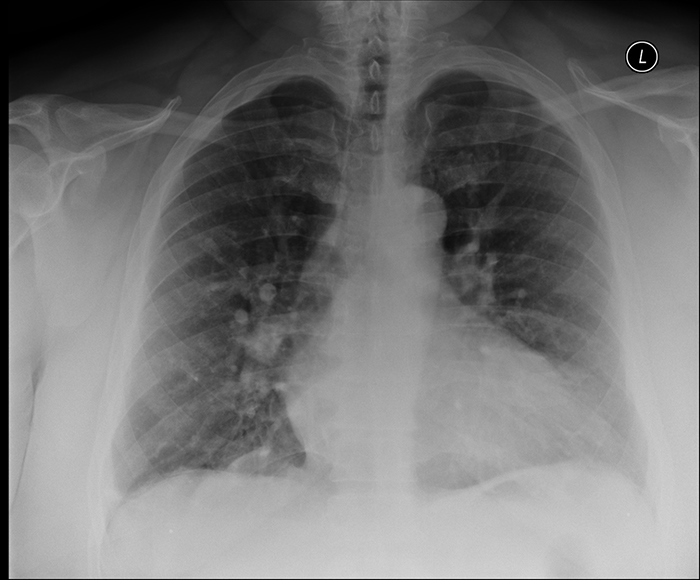
A 70-year-old woman is brought to the emergency department by her son for evaluation of shortness of breath. She has had a sensation of choking since last night. According to her son, for the past several weeks she has had a dry cough at night and has been taking over-the-counter cough drops. The patient has had no chest pain, palpitations, back pain, abdominal symptoms, or lightheadedness. She has a history of hypertension, hyperlipidemia, and type 2 diabetes mellitus. She has been refusing statin therapy, as she heard statins cause multiple side effects. The patient has also refused flu vaccinations over the last several years. Her only hospital admission occurred 6 years ago when she underwent a spinal fusion for lower back pain. She does not use tobacco, alcohol, or illicit drugs. Family history is not significant. Temperature is 36.1 C (97 F), blood pressure is 171/102 mm Hg, pulse is 92/min, and respirations are 34/min. Pulse oximetry is 85% on room air. BMI is 29 kg/m2. Bilateral crackles are heard on lung examination. There are no heart murmurs. ECG shows normal sinus rhythm, increased voltage in the precordial leads, and T-wave inversion in leads V5 and V6. Chest x-ray is shown in the exhibit. Oxygen is administered via 100% nonrebreather facemask.
Item 1 of 3
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
Item 2 of 3
The patient is placed on noninvasive positive pressure ventilation but still appears somewhat uncomfortable. Laboratory results are as follows:
Hemoglobin
11.4 g/dL
Platelets
180,000/mm3
Leukocytes
10,000/mm3
Sodium
131 mEq/L
Potassium
3.8 mEq/L
Creatinine
1.4 mg/dL
The first troponin I level is negative. Repeat blood pressure is 176/105 mm Hg, pulse is 82/min, and respirations are 24/min. Oxygen saturation is 94%. What is the best next step in management of this patient?
CorrectIncorrect -
Question 12 of 40
12. Question
Item 3 of 3
The patient is responding well to treatment. The second troponin I level is negative. Which of these tests is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
A 53-year-old man comes to the office due to newly diagnosed hypertension. The patient has no symptoms. Medical history is significant for type 2 diabetes mellitus. He has a 50-pack-year smoking history and has consumed 1 or 2 cans of beer daily for the past 25 years. Blood pressure is 150/95 mm Hg and pulse is 80/min. Height is 183 cm (6 ft) and weight is 109 kg (240.3 lb). BMI is 32.5 kg/m2. Physical examination is normal. The physician recommends medication and lifestyle changes to lower blood pressure and decrease the risk of future cardiovascular events. Which of the following nonpharmacologic measures would be the most effective in decreasing this patient’s blood pressure?
CorrectIncorrect -
Question 14 of 40
14. Question
The following vignette applies to the next 3 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 42-year-old man comes to the office due to a painless lump under the skin on his right upper back, which he first noticed 3 months ago. He is incidentally noted to have a blood pressure of 180/110 mm Hg. He has no symptoms. The patient has no history of hypertension or other medical conditions and has not seen a physician since high school. He takes no medications, does not use tobacco, and consumes 1 or 2 alcoholic beverages on weekends. Family history is notable for hypertension in his mother and end-stage renal disease in a maternal uncle. The patient exercised regularly until recently, when he started work as a supervisor at a warehouse. He eats fast food at least 3 days a week. Repeat blood pressure measurements after 15 minutes of rest are 180/105 mm Hg on the right arm and 185/110 mm Hg on the left. Temperature is 36.7 C (98.1 F), pulse is 68/min, and respirations are 12/min. BMI is 26.2 kg/m2. Cardiac examination reveals a diffuse and sustained apical impulse with normal heart sounds and no murmurs or gallops. There is a 3-cm, soft, mobile, nontender, subcutaneous mass consistent with a lipoma in the right scapular region. The remainder of the examination, including funduscopy, is normal. Blood cell counts, serum electrolytes, serum creatinine, blood glucose, and urinalysis are within normal limits. The ECG is shown in the exhibit.

Item 1 of 3
In addition to providing reassurance regarding the patient’s skin lesion, which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 15 of 40
15. Question
Item 2 of 3
Which of the following is the best initial therapy for this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
Item 3 of 3
Which of the following additional tests is most appropriate for this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
A 54-year-old man is brought by his wife to the emergency department of a rural hospital due to chest discomfort. The pain began approximately an hour ago while he was mowing the lawn. He describes the chest pain as feeling “like a pickup truck is right on top of me.” The patient took an aspirin at home, but the pain has not improved. He has a history of hypertension, chronic constipation, and onychomycosis. He smokes a pack of cigarettes a day and consumes 1-3 alcoholic drinks a night; he does not use illicit drugs. Temperature is 37.7 C (99.9 F), blood pressure is 142/90 mm Hg, pulse is 106/min, and respirations are 21/min. Oxygen saturation is 96% on room air. Weight is 115 kg (253.5 lb) and height is 175 cm (5′ 9″). BMI is 37.4 kg/m2. The patient appears uncomfortable and is diaphoretic. There is diffuse mild chest tenderness to palpation. Cardiac auscultation reveals a low-pitched sound at the apex just before S1. No edema of the extremities is evident. The remainder of the examination is unremarkable. The patient is given nitroglycerin, which improves the pain but does not relieve it. Which of the following findings on ECG most strongly indicates the need for tenecteplase?
CorrectIncorrect -
Question 18 of 40
18. Question
A 62-year-old man is brought to the emergency department with substernal pain and mild shortness of breath over the last 2 hours. En route he was given sublingual nitroglycerin twice with significant relief of pain. He also received chewable aspirin. The patient currently rates the pain as 1-2 out of 10. His past medical history is significant for hypertension and active smoking. He has no history of bleeding. The patient’s father died of a heart attack at age 56. Blood pressure is 154/90 mm Hg and pulse is 110/min. He is not in respiratory distress. No murmurs are heard. Lungs are clear to auscultation. The initial electrocardiogram (ECG) is shown in the Exhibit. Which of the following is the best next step in management of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 19 of 40
19. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 28-year-old woman comes to the emergency department due to the abrupt onset of palpitations that started while she was watching television. She says, “I suddenly started to feel like my heart was racing.” The patient describes mild lightheadedness but no chest pain, shortness of breath, or syncope. In the past, she has experienced similar episodes of palpitations that were nonsustained and terminated abruptly. The patient has never sought medical care for these episodes and cannot identify any provoking factor. She saw a physician for anxiety when she was a teenager but does not remember if she received any therapy. The patient has no other medical problems and takes no medications. She does not use tobacco, alcohol, or illicit drugs. She jogs 2-3 miles a day. The patient has no family history of coronary artery disease, cardiomyopathy, blood clots, or sudden cardiac death. She appears mildly uncomfortable but not in any respiratory distress. Temperature is 36.7 C (98 F), blood pressure is 100/60 mm Hg, pulse is 172/min, and respirations are 20/min. Urine pregnancy test is negative. ECG is shown in the exhibit.

Item 1 of 2
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 20 of 40
20. Question
Item 2 of 2
The patient receives antiarrhythmic therapy, and her pulse immediately decreases from 172/min to 68/min. The palpitations resolve, and she states that she feels “normal now.” Cardiac examination reveals no murmurs or additional sounds. A 12-lead ECG is performed and is shown in the exhibit. Which of the following is the most likely diagnosis?
 CorrectIncorrect
CorrectIncorrect -
Question 21 of 40
21. Question
A 66-year-old man comes to the office for evaluation of progressive shortness of breath for the past 2 months. The patient used to walk nearly a mile a day without difficulty. More recently, however, he feels “out of breath” and tires easily after walking a few blocks. The patient has gained 4 kg (8.8 lb) over a similar period. He has also had a persistent, dry cough that is worse at night when he is lying in bed. The patient has had no fever, chills, or night sweats. He has a history of hypertension. He is a former smoker who quit 5 years ago. Until 4 years ago, the patient worked as an engineer at a local steel mill. Temperature is 36.1 C (97 F), blood pressure is 154/90 mm Hg, pulse is 92/min and regular, and respirations are 20/min. Pulse oximetry is 94% on room air. BMI is 47.4 kg/m2. The lungs are clear on auscultation. S1 and S2 are normal, and the point of maximal impulse is not palpable due to the patient’s body habitus. The abdomen is soft and nontender. There is 1+ pretibial edema bilaterally. Initial complete blood count and complete metabolic panel are unremarkable. B-type natriuretic peptide is 95 pg/mL (normal: 100-400). ECG shows normal sinus rhythm with evidence of left atrial enlargement. Chest x-ray is shown in the exhibit. Echocardiography reveals concentric left ventricular hypertrophy, left atrial enlargement, and a left ventricular ejection fraction of 60%. Which of the following is the most likely cause of this patient’s current symptoms?
 CorrectIncorrect
CorrectIncorrect -
Question 22 of 40
22. Question
A 31-year-old man is evaluated for a murmur. He has no other symptoms and his past medical history is unremarkable. He jogs 3 times per week and rides a bicycle on the weekend. His blood pressure is 122/70 mm Hg on the right arm and 125/75 mm Hg in both ankles. On physical examination, a harsh, 4/6 holosystolic murmur is heard at the 4th left intercostal space close to the sternal border accompanied by a thrill. The rest of the physical examination is within normal limits. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 23 of 40
23. Question
A 62-year-old man comes to the emergency department due to dyspnea that started 2 days ago and has worsened significantly over the past several hours. The patient was unable to lie flat last night and had to sleep in a chair. Medical history is significant for hypertension, type 2 diabetes mellitus, and coronary artery disease. Medications include aspirin, atorvastatin, lisinopril, and metformin. Blood pressure is 160/100 mm Hg and pulse is 90/min and regular. Crackles are heard at the lung bases bilaterally. No murmurs are heard on cardiac auscultation, but a soft extra heart sound is heard at the cardiac apex just after an S2. This extra heart sound corresponds with which of the following events of the cardiac cycle?
CorrectIncorrect -
Question 24 of 40
24. Question
The following vignette applies to the next 2 items
A 70-year-old man comes to the hospital due to fever, lethargy, productive cough, and shortness of breath. He has type 2 diabetes mellitus, hypertension, paroxysmal atrial fibrillation, and peripheral vascular disease. His medications include warfarin, sotalol, insulin detemir, and lisinopril. Chest x-ray shows infiltrates in the left lung base. He is admitted and treated with azithromycin, ceftriaxone, and oxygen therapy.
Item 1 of 2
On the second day of hospitalization, he has 2 episodes of loss of consciousness associated with seizure-like activity. The telemetry strips during one of these episodes is shown in the exhibit. Which of the following is most likely to provoke a recurrent event in this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 25 of 40
25. Question
Item 2 of 2
On examination, the patient is now awake and alert but oriented only to person. His blood pressure is 120/70 mm Hg, pulse is 65/min, and respirations are 14/min. Laboratory tests ordered 30 minutes before the first event are shown below.
Serum chemistry
Sodium
144 mEq/L
Potassium
4.5 mEq/L
Chloride
108 mEq/L
Bicarbonate
20 mEq/L
Blood urea nitrogen
20 mg/dL
Creatinine
1.1 mg/dL
Calcium
9.6 mg/dL
Blood glucose
240 mg/dL
Magnesium
1.8 mg/dL
Phosphorus
3.5 mg/dL
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 26 of 40
26. Question
A 61-year-old woman comes to the physician due to mild exertional dyspnea. She has difficulty going up the stairs and feels very tired by the end of the day. She has no chest pain, orthopnea, lower extremity swelling, or syncope. The patient is being treated for locally advanced HER2-positive breast cancer. She underwent left-sided mastectomy and received adjuvant chemotherapy with docetaxel and carboplatin in addition to trastuzumab 6 months ago. Preoperative evaluation showed normal cardiac function. Currently, the patient receives periodic trastuzumab infusions. Echocardiogram shows a left ventricular ejection fraction of 30%. The patient wonders if her symptoms are related to cancer therapy and wants to know her long-term prognosis. What is the best response to this patient’s concerns?
CorrectIncorrect -
Question 27 of 40
27. Question
A 60-year-old man undergoes imaging that reveals a 3.5-cm abdominal aortic aneurysm. The finding is incidental; he has no associated symptoms. Medical history is significant for hypertension, type 2 diabetes mellitus, hypercholesterolemia, and hypothyroidism. Current medications include aspirin, metformin, glipizide, chlorthalidone, lisinopril, atorvastatin, and levothyroxine. The patient has a 40-pack-year history and continues to smoke 1-2 packs a day. He drinks 3 or 4 glasses of wine daily. Blood pressure is 160/90 mm Hg and pulse is 80/min. Cardiopulmonary examination is normal. Laboratory results are as follows:
Serum creatinine
1.3 mg/dL
LDL
150 mg/dL
Hemoglobin A1c
8.5%
Serum TSH
3.0 µU/mL
Which of the following interventions would most effectively decrease the likelihood of expansion of this patient’s aortic aneurysm?
CorrectIncorrect -
Question 28 of 40
28. Question
A 68-year-old woman comes to the office due to a month-long history of worsening fatigue, shortness of breath, and dry cough. The patient has symptoms that worsen with exertion and when lying flat. She has had no chest pain, palpitations, or lightheadedness. The patient has a history of hypertension and breast cancer that is in remission after surgery and doxorubicin-based chemotherapy 15 years ago. She does not use tobacco, alcohol, or illicit drugs. Blood pressure is 110/62 mm Hg and pulse is 94/min. Physical examination shows crackles at the lung bases and bilateral pedal edema. Which of the following sets of findings are most likely present in this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 29 of 40
29. Question
A 51-year-old man comes to the office for a follow-up visit. He has no concerns. His medical conditions include type 2 diabetes mellitus, hypertension, and obesity. The patient does not use tobacco, alcohol, or illicit drugs. His mother and maternal grandfather also had diabetes. His current medications include aspirin, glyburide, metformin, and lisinopril. Blood pressure is 144/79 mm Hg and pulse is 88/min. Weight is 120 kg (265 lb). Examination shows no abnormalities. Laboratory results are as follows:
Total cholesterol
230 mg/dL
LDL
135 mg/dL
HDL
60 mg/dL
Triglycerides
190 mg/dL
Glucose
118 mg/dL
Hemoglobin A1c
6.8%
Alanine aminotransferase (SPGT)
22 U/L
Which of the following is the most appropriate therapy to prevent atherosclerotic cardiovascular disease in this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 72-year-old man is brought to the emergency department after an episode of syncope during a family gathering. The patient was sitting in his chair after dinner and passed out briefly. There are no apparent injuries and no seizure-like activity was observed. His granddaughter says that he has had frequent episodes of dizziness in the last 2 weeks. These episodes are sometimes accompanied by confusion and are not related to physical activity or changes in position. The patient’s other medical problems include coronary artery disease and hypertension. He does not use alcohol or tobacco. His medications include aspirin, lisinopril, atorvastatin, and isosorbide mononitrate. Blood pressure is 105/60 mm Hg and respirations are 14/min. The patient is fully alert and oriented. Examination reveals no neck bruits. Lung fields are clear, and no cardiac murmurs are heard. Neurologic examination is within normal limits. ECG is shown in the exhibit. Serum potassium is 4.1 mEq/L and serum creatinine is 1.1 mg/dL. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 39-year-old man comes to the emergency department due to an episode of chest pain. He says, “I had dinner and 2 hours later started to get this discomfort in the middle of the chest. It felt dull and annoying.” The pain lasted for 2 hours, waxed and waned in intensity, and did not radiate. The patient did not have any back pain, dyspnea, palpitations, or lightheadedness, and has never had similar pain episodes. After the pain subsided, his wife insisted that he go to the emergency department. Currently, he has no pain or discomfort and wants to return home. The patient does have occasional heartburn and takes over-the-counter antacids. Medical history is otherwise unremarkable. The patient has smoked a pack of cigarettes a day for the past 10 years. He does not drink alcohol or use illicit drugs. He has no known medication allergies. His father died suddenly in his sleep at age 55. His older brother is healthy. Blood pressure is 138/86 mm Hg and pulse is 89/min and regular. BMI is 28 kg/m2. There are no heart murmurs or additional sounds. No carotid bruits are heard. Abdominal examination is unremarkable. ECG shows normal sinus rhythm with nonspecific T-wave changes in leads II and III. Chest x-ray is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 24-year-old man is evaluated due to a syncopal episode that occurred immediately after he completed a 13-mile half-marathon. The patient felt light-headed and then passed out. He was immediately placed in a supine position and regained consciousness after 2-3 minutes. The patient has no chest pain, palpitations, or shortness of breath. He has never had a similar episode. There is no family history of sudden death. The patient does not use alcohol or illicit drugs. Temperature is 37 C (98.6 F), blood pressure is 98/56 mm Hg, pulse is 80/min, and respirations are 14/min. Complete physical examination and ECG show no abnormalities. Which of the following is the most likely mechanism of this patient’s syncope?
CorrectIncorrect -
Question 33 of 40
33. Question
A 55-year-old man is brought to the emergency department due to shortness of breath and weakness. The symptoms have been present for approximately 3 weeks but have rapidly progressed over the last 2 days. He felt too weak to get up to use the bathroom today. The patient was diagnosed with non-small cell lung cancer 2 years ago. At that time, he underwent surgical resection, followed by cisplatin-based combination chemotherapy. Since then, he has had follow-up CT scans every 6 months without evidence of recurrence. His last scan was 5 months ago. Other medical history includes mitral valve prolapse, for which he has been followed with echocardiography every 3 years. The patient used to take antibiotics prior to dental procedures but stopped a few years ago when his cardiologist advised him that it was no longer necessary. He currently takes no medications. His mother died of congestive heart failure at age 80 and his father has emphysema. The patient does not use tobacco, alcohol, or illicit drugs. He formerly worked as a diesel mechanic but retired at the time of his cancer diagnosis. Temperature is 37.8 C (100 F), blood pressure is 85/60 mm Hg, and pulse is 110/min and regular. Cardiac auscultation reveals distant heart sounds. The lungs are clear to auscultation. He has 1+ pitting lower extremity edema bilaterally. Bedside echocardiography shows moderate pericardial effusion. Which of the following best confirms the need for immediate invasive management in this patient?
CorrectIncorrect -
Question 34 of 40
34. Question
A 68-year-old white male with a history of paroxysmal atrial fibrillation, hypertension, and hypercholesterolemia is brought to the physician’s office by his daughter because of nausea, anorexia, and confusion. His daughter states that he was admitted at an outside hospital two weeks ago because of uncontrolled hypertension and palpitations. He was started on a new medication. Prior to the recent hospitalization, he was taking digoxin, warfarin, simvastatin, and hydrochlorothiazide. His physical examination shows an irregular heart rate, but is otherwise unremarkable. His blood pressure is 130/80 mmHg, pulse rate is 50/minute and irregular, temperature 37.2C (99F), and respirations are 14/minute. Which of the following is the most likely medication that is contributing to his symptoms?
CorrectIncorrect -
Question 35 of 40
35. Question
A 70-year-old man is brought to the emergency department by his wife after an episode of syncope while working in his garden. He regained consciousness immediately and initially refused to go to the hospital saying, “I feel fine.” The patient has never experienced syncope before. According to his wife, he has always been physically active but lately has had increased fatigability; he seems to work less in the garden and spends more time indoors watching television. Medical history is significant for type 2 diabetes mellitus and gout. His only current medication is metformin. He is a lifetime nonsmoker and does not drink alcohol. Blood pressure is 100/80 mm Hg and pulse is 90/min. BMI is 28 kg/m2. Both carotid pulses are delayed. Lungs are clear on auscultation. A harsh crescendo-decrescendo murmur is heard at the base of the heart. The second heart sound is soft with an inaudible A2 component. There is no peripheral edema. ECG shows normal sinus rhythm, left ventricular hypertrophy, and secondary ST-segment and T-wave changes. Echocardiography shows concentric left ventricular hypertrophy with severe calcification of the aortic valve. The estimated aortic valve area is 0.78 cm2 and the mean transvalvular gradient is 50 mm Hg. Laboratory studies show normal complete blood count and serum creatinine of 0.8 mg/dL. Which of the following is the best statement about this patient’s condition?
CorrectIncorrect -
Question 36 of 40
36. Question
A 74-year-old hospitalized woman is seen for preoperative medical evaluation. The patient was admitted due to a right ankle injury after stepping off a curb and falling. She did not hit her head or lose consciousness during the event. The patient has had no recent chest pain, dyspnea, palpitation, or syncope. Prior to the injury, she was able to walk 1-2 blocks on a flat level and climb a flight of stairs without difficulty. Medical history is significant for hypertension, paroxysmal atrial fibrillation, osteoporosis, and mild cognitive impairment. Medications are amlodipine, metoprolol, rivaroxaban, alendronate, and vitamin D supplements. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 136/88 mm Hg and pulse is 88/min and irregular. Physical examination shows clear lungs and no heart murmurs. Right ankle x-rays reveal a bimalleolar fracture. ECG shows atrial fibrillation with normal ventricular rate. Blood cell count, serum chemistry studies, prothrombin time, and activated partial thromboplastin time are within normal limits. Orthopedic consultation has been obtained, and an operative repair of the fracture is planned in the next 48 hours. In addition to rivaroxaban discontinuation, which of the following is the most appropriate preoperative recommendation regarding this patient’s arrhythmia?
CorrectIncorrect -
Question 37 of 40
37. Question
A 45-year-old woman who recently immigrated to the United States is hospitalized with exertional dyspnea and fatigue. She has no significant past medical history and takes no medications. The patient’s blood pressure is 110/80 mm Hg and heart rate is 90/min and regular. After cardiopulmonary examination, the physician suspects mitral stenosis. Which of the following is the most useful measure for assessing the degree of mitral stenosis?
CorrectIncorrect -
Question 38 of 40
38. Question
An 80-year-old man is admitted to the cardiac care unit after undergoing a complicated percutaneous coronary intervention procedure. He has chest discomfort and shortness of breath. Blood pressure is 82/50 mm Hg and pulse is 114/min and regular. Hemodynamic readings from the pulmonary artery catheter are shown below.
Right atrial pressure
12 mm Hg (normal: 1-6)
Right ventricular pressure
42/16 mm Hg (normal: 15-30/1-6)
Pulmonary artery pressure
45/20 mm Hg (normal: 15-30/6-12)
Pulmonary capillary wedge pressure
25 mm Hg (normal: 6-12)
Cardiac index
1.6 L/min/m2 (normal: 2.8-4.2)
Systemic vascular resistance
1,420 dyne-sec/cm5 (normal: 800-1,200)
Which of the following is the most likely cause of this patient’s hypotension?
CorrectIncorrect -
Question 39 of 40
39. Question
A 67-year-old man comes to the office due to fatigue and lower extremity edema. Nine months ago, he underwent coronary artery bypass graft surgery and mitral valve repair. His postoperative course was complicated by paroxysmal atrial fibrillation treated with amiodarone and anticoagulation. He also has diet-controlled type 2 diabetes mellitus. The patient is a former smoker with a 35-pack-year history. Blood pressure is 132/77 mm Hg and pulse is 102/min. Jugular venous pressure is estimated at 16 cm H2O. Cardiac auscultation demonstrates an early diastolic high-pitch sound. The lungs are clear to auscultation. There is significant ascites and bilateral lower extremity edema. ECG shows sinus tachycardia. Echocardiography reveals enlarged atria, normal left ventricular wall thickness and right ventricular size, and a left ventricular ejection fraction of 65%. There is mild mitral regurgitation. Chest x-ray reveals normal heart size, clear lung fields, and patchy calcifications along the left heart border. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 40 of 40
40. Question
A 30-year-old man comes to the office for a routine annual office visit. He has no symptoms and has good exercise tolerance. There is no family history of cardiovascular disease. The patient does not use tobacco, alcohol, or recreational drugs. Vital signs are within normal limits. Eye examination shows no evidence of retinopathy. The lungs are clear. S1 and S2 are normal, and an S4 is present. A grade 2/6 crescendo-decrescendo systolic murmur is heard at the lower left sternal border. The murmur does not radiate to the carotid arteries. Performing a passive leg raise while the patient is recumbent decreases murmur intensity. Rapid upstrokes of the peripheral pulses are present. Echocardiography is requested. Which of the following is the most accurate statement about the prognosis of this patient?
CorrectIncorrect
