Time limit: 0
Quiz Summary
0 of 26 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 26 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 26
1. Question
A 32-year-old woman comes to the emergency department due to progressive weakness and shortness of breath over the past several weeks. The patient has had 2 prior pregnancies, most recently 2 years ago. She has smoked a pack of cigarettes a day since age 17 and uses methamphetamine. The patient has no family history of heart disease or sudden cardiac death. Temperature is 36.1 C (97 F), blood pressure is 88/60 mm Hg, pulse is 105/min and regular, and respirations are 22/min. Pulse oximetry is 91% on room air. The patient sits upright in bed and appears uncomfortable. Examination shows diffuse crackles throughout the lung fields. An apical impulse is palpated along the left anterior axillary line. An extra low-pitched sound in early diastole is best heard with the bell of the stethoscope placed on the apex. The patient’s legs are cool and pulses are diminished. There is 1+ bilateral peripheral edema. Laboratory results are as follows:
Sodium
134 mEq/L
Potassium
4.0 mEq/L
Chloride
100 mEq/L
Bicarbonate
18 mEq/L
Blood urea nitrogen
40 mg/dL
Creatinine
1.9 mg/dL
Calcium
8.6 mg/dL
Glucose
80 mg/dL
Pregnancy test is negative. In addition to other appropriate therapy, the patient is given an intravenous medication that acts primarily by stimulating beta-1 adrenergic receptors. Which of the following is the major result of therapy with this medication?
CorrectIncorrect -
Question 2 of 26
2. Question
A 62-year-old woman comes to the physician due to chest and epigastric discomfort over the last 6 months. She feels dull chest pressure while walking uphill at a fast pace. The patient says, “It is unusual. I feel this pressure only once in a while, even when doing the same thing. Sometimes it is worse when I walk fast after a heavy meal.” She has a history of nonulcer dyspepsia and acid reflux disease and occasionally takes over-the-counter omeprazole. She has no shortness of breath, palpitations, lightheadedness, lower extremity swelling, or syncope. The patient is physically active and has a very hectic social lifestyle. Medical history includes “borderline” hypertension and anxiety disorder. She stopped taking antihypertensive medications 5 years ago. She is a lifetime nonsmoker. The patient does not use alcohol or illicit drugs. Her mother suffered a stroke at age 70 and her father died of prostate cancer. Blood pressure is 145/90 mm Hg and pulse is 80/min and regular. BMI is 29 kg/m2. No heart murmurs are heard on cardiac auscultation. There are no carotid bruits. The lungs are clear and the rest of the physical examination is unremarkable. Resting ECG shows normal sinus rhythm, normal voltage, and T-wave flattening in leads V5 and V6. Laboratory studies show fasting blood glucose of 102 mg/dL and LDL cholesterol of 110 mg/dL. Which of the following is most appropriate management for this patient’s chest pain?
CorrectIncorrect -
Question 3 of 26
3. Question
A 45-year-old woman comes to the physician due to a 4-month history of vague abdominal pain that is unrelated to food intake. The pain occasionally occurs in the middle of the night. She has had loss of appetite during this period but no nausea, vomiting, weight loss, or blood in the stool. Three years ago, the patient had aortic valve replacement with a mechanical valve for bicuspid aortic valve and aortic root repair. Her only medication is daily warfarin. Recent laboratory results showed hemoglobin of 11.2 g/dL and an INR of 2.5. Echocardiography 4 weeks ago revealed normal left ventricular function and a normally functioning prosthetic aortic valve. She is scheduled for upper gastrointestinal endoscopy to evaluate her abdominal pain. The decision is made not to interrupt her anticoagulation. Which of the following is the best additional recommendation before this patient’s procedure?
CorrectIncorrect -
Question 4 of 26
4. Question
A 28-year-old man comes to the emergency department with palpitations. For the past 6 months, he has had palpitations that were intermittent and short-lived but seem persistent today. Past medical history is unremarkable. His BMI is 24 kg/m2. Cardiac auscultation reveals a II/VI mid-systolic murmur at the left upper sternal border. Electrocardiogram (ECG) shows atrial fibrillation with rapid ventricular response. Echocardiogram shows normal left ventricular size and function and right atrial and ventricular dilation. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 5 of 26
5. Question
A 62-year-old man is brought to the emergency department due to shortness of breath, chest pain, and palpitations that started earlier today. For the past month, he has had intermittent palpitations accompanied by shortness of breath. This time the symptoms persisted and he called 911. Medical problems include hypertension, obesity, chronic obstructive pulmonary disease, myocardial infarction, and carotid artery stenosis. The patient underwent coronary artery bypass grafting surgery 4 years ago. He follows up with a cardiologist twice a year, and there has been no recent change in his medical regimen. He is an ex-smoker and consumes no alcohol. He has no known drug allergies. On initial evaluation in the emergency department, he appears uncomfortable and tachypneic. Immediate ECG shows atrial fibrillation with a rapid ventricular response (140-150/min), narrow QRS complexes, and T-wave inversion in leads V4 to V6. The patient is connected to a cardiac monitor. While the team is securing intravenous access, the patient becomes unresponsive. He has no palpable pulses over the major arteries. The cardiac monitor continues to show a narrow-complex tachycardia consistent with atrial fibrillation. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 6 of 26
6. Question
A 46-year-old woman comes to the clinic for follow-up treatment of hypertension. The patient was diagnosed with hypertension 2 years ago and nonpharmacological management was initially advised. A year ago, she was started on valsartan and amlodipine after her blood pressure was measured at 144/86 mm Hg. A month after treatment initiation, she reported no adverse effect from the medication and blood pressure was 130/80 mm Hg. Since then, the patient has missed several follow-up appointments, which she attributes to being busy at work. She currently has no concerns and overall feels “great.” She has had no chest pain, headaches, lightheadedness, or syncope. The patient has no other medical issues and does not use tobacco or alcohol. She works as a salesperson and eats fast food a few times a month. Her mother died of a stroke at age 67. Today, blood pressure is 152/88 mm Hg in the right arm and 148/86 mm Hg in the left arm; pulse is 76/min and regular. Repeat blood pressure measurements after 15 minutes of rest are similar. BMI is 28 kg/m2. Estimated jugular venous pressure is normal. There are no carotid bruits. Heart sounds are normal with no murmurs. Lung examination is unremarkable. Peripheral pulses are full and symmetric. There is no peripheral edema. Laboratory results are as follows:
Sodium
140 mEq/L
Potassium
4.1 mEq/L
Creatinine
0.8 mEq/L
Total cholesterol
201 mg/dL
LDL cholesterol
128 mg/dL
ECG shows normal sinus rhythm with nonspecific T-wave changes. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 7 of 26
7. Question
A 56-year-old man comes to the emergency department due to chest pain that occurred at home. He was watching television when he developed left-sided chest pain described as dull and pressure-like. The pain progressively worsened and radiated to the throat but spontaneously resolved within 20 minutes. During the past week, the patient had 2 similar episodes with exertion at his job as a construction worker. He has had no palpitations, syncope, shortness of breath, or diaphoresis. He has a history of hypertension treated with lisinopril and is a lifetime nonsmoker. Family history is significant for stroke at a young age in a paternal uncle. The patient is currently free of chest pain and comfortable. Blood pressure is 150/80 mm Hg and pulse is 78/min. Physical examination is otherwise unremarkable. ECG shows sinus rhythm with T-wave inversion in leads V5 and V6. Chest x-ray is normal. Cardiac troponin I level is normal (<0.012 ng/dL). Aspirin, metoprolol, atorvastatin, clopidogrel, and subcutaneous enoxaparin are initiated. Eight hours later, he is still without chest pain. ECG is unchanged and repeat troponin I level is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 8 of 26
8. Question
A 44-year-old man comes to the urgent care clinic due to palpitations. The current episode started 2 hours ago and feels like “fluttering in the chest.” He has no chest pain, orthopnea, dizziness, syncope, or shortness of breath. The patient has had similar episodes in the past 6 months, but they usually last less than an hour and resolve spontaneously. He cannot identify any clear-cut precipitating factor for these episodes. He has a history of migraines and kidney stones. The patient does not use tobacco, alcohol, or illicit drugs. Family history is significant for liver cancer and renal failure. He works in an office and his lifestyle is mainly sedentary. On initial evaluation, he appears comfortable. Blood pressure is 124/82 mm Hg and pulse is 122/min. Oxygen saturation is 99% on room air. BMI is 31 kg/m2. Cardiac auscultation reveals no murmurs. The patient’s lungs are clear to auscultation and there is no peripheral edema. ECG shows atrial fibrillation with a rapid ventricular response. Complete blood count, basic metabolic panel, TSH level, and chest x-ray are normal. A transthoracic echocardiogram shows normal left ventricular size and function, mild enlargement of the left atrium, and no valvular abnormalities. The patient is given oral metoprolol and reports improvement of his symptoms after 2 hours. Repeat ECG shows normal sinus rhythm with a ventricular rate of 77/min at rest. There are no repolarization abnormalities and his QTc interval is 410 msec. In addition to oral metoprolol, which of the following is the most appropriate management for this patient?
CorrectIncorrect -
Question 9 of 26
9. Question
A 74-year-old woman comes to the office for evaluation of increasing lower extremity swelling. The patient has a history of hypertension, obstructive sleep apnea, and mild, chronic lower extremity edema for several years. She reports “increased swelling and throbbing pain in my right leg” over the last 3 days. BMI is 40 kg/m2. She takes hydrochlorothiazide and lisinopril and uses continuous positive airway pressure at nighttime. Temperature is 36.5 C (97.7 F), blood pressure is 154/92 mm Hg, pulse is 76/min and regular, and respirations are 17/min. The patient is in no acute distress. Jugular venous pressure is elevated. The lungs are clear to auscultation. A loud P2 is present. There is 3+ edema in the right leg and 1+ edema in the left leg. There is no warmth, erythema, or tenderness to palpation of the lower extremities. Distal pulses are normal. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 10 of 26
10. Question
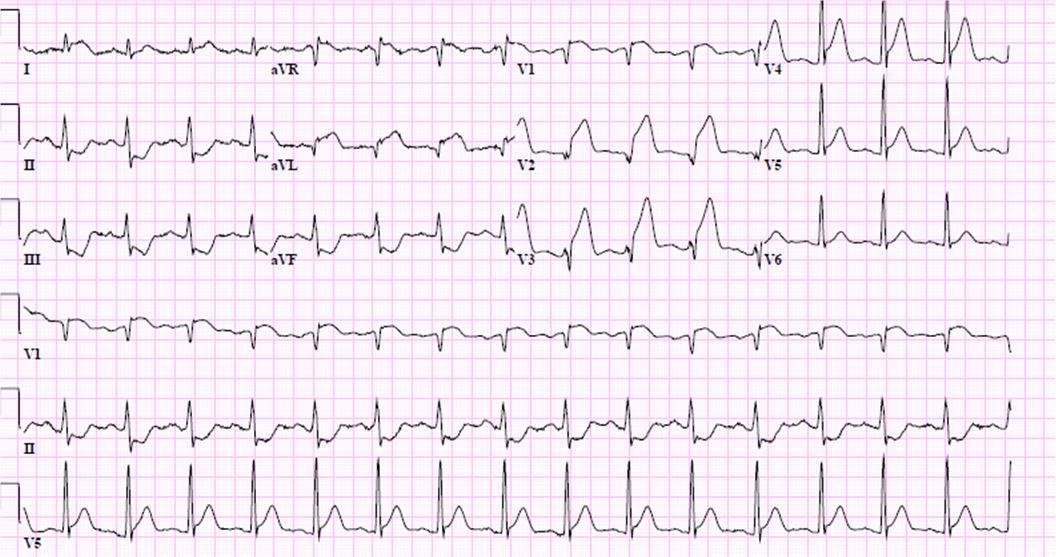
A 72-year-old man comes to the office due to palpitations and mild fatigue for the last 3 weeks. He has otherwise been feeling well. The patient walks 2 miles around his neighborhood twice per week with no chest pain or shortness of breath. Medical history is remarkable for benign prostatic hyperplasia, for which he takes terazosin. He drinks 1-2 cups of coffee every day and a glass of wine once or twice per month. Temperature is 37 C (98.6 F), blood pressure is 128/68 mm Hg, and pulse is 78/min and irregular. Physical examination reveals a 2/6 early-peaking systolic murmur at the right upper sternal border. Carotid pulses are prompt and full bilaterally. The lungs are clear to auscultation. There is no peripheral edema. ECG is shown in the exhibit. Which of the following is most likely the strongest risk factor for this patient’s presentation?
 CorrectIncorrect
CorrectIncorrect -
Question 11 of 26
11. Question
A 52-year-old woman comes to the emergency department due to increasing dyspnea and chest tightness over the past 2 weeks. She has a history of stage 4 chronic kidney disease due to chronic glomerulonephritis. Temperature is 36.6 C (97.8 F), blood pressure is 106/82 mm Hg, and pulse is 98/min. Systolic blood pressure decreases by 12 mm Hg during inspiration. Physical examination shows distant heart sounds and clear lungs. Echocardiography in this patient is most likely to reveal which of the following findings?
CorrectIncorrect -
Question 12 of 26
12. Question
A 22-year-old woman comes to the office due to worsening dyspnea. The patient has also experienced low-grade fevers, a 6.8-kg (15-lb) weight loss, and syncopal episodes over the last 3 months. Her shortness of breath worsens when sitting and improves when lying down. Medical history is insignificant. The patient does not use tobacco, alcohol, or illicit drugs. Temperature is 37.4 C (99.3 F), blood pressure is 115/72 mm Hg, pulse is 75/min and regular, and respirations are 12/min. The lungs are clear. Cardiac auscultation reveals a low-pitched, mid-diastolic rumble at the cardiac apex. The remainder of the physical examination is normal. ECG reveals left atrial enlargement, and echocardiography shows a large, pedunculated mass in the left atrium. Histologic analysis of this mass will most likely reveal which of the following?
CorrectIncorrect -
Question 13 of 26
13. Question
A 70-year-old man comes to the office for a preoperative medical evaluation. During screening colonoscopy, the patient was found to have localized colon cancer, and segmental colon resection is planned in a week. The patient has had no recent chest pain, dyspnea, palpitation, or syncope. He is able to walk 1-2 blocks on a level surface and climb a flight of stairs without difficulty. The patient has a history of hypertension, atrial fibrillation, and an episode of transient ischemic attack a year ago. Medications include amlodipine, metoprolol, and rivaroxaban. He does not use tobacco, alcohol, or illicit drugs. Blood pressure is 126/84 mm Hg and pulse is 76/min and irregular. Physical examination shows no abnormalities. Blood cell counts and serum chemistry studies are within normal limits. ECG reveals atrial fibrillation with a controlled ventricular response. Which of the following is the most appropriate recommendation for the preoperative management of this patient’s arrhythmia?
CorrectIncorrect -
Question 14 of 26
14. Question
A 56-year-old man is brought to the emergency department with a 4-hour history of crushing, substernal chest pain. His ECG shows a 3-mm ST-segment elevation in leads V2-V4. He is taken for coronary angiography and undergoes primary percutaneous coronary intervention with stenting of the occluded mid-left anterior descending artery. There is a 30%-40% stenosis of the right coronary artery that does not require intervention and no stenosis in the left circumflex artery. After the procedure, the patient is admitted to the coronary care unit. Echocardiogram shows mild anterior wall hypokinesis and a normal left ventricular ejection fraction. He remains chest pain free throughout his 3-day hospital stay. The patient is started on dual antiplatelet therapy. He begins a progressive supervised activity program, which is uneventful, and he is subsequently discharged home. At a follow-up appointment 3 weeks later, he reports that he has been walking for 20 minutes each day without any symptoms. The patient occasionally has some bleeding when brushing his teeth, but is otherwise asymptomatic. He asks whether it would be safe for him to resume sexual activity. Which of the following is the most appropriate recommendation?
CorrectIncorrect -
Question 15 of 26
15. Question
A 62-year-old woman comes to the office due to episodic tightness over her anterior chest for the past 6 months. It sometimes occurs while the patient is walking or climbing stairs, but several episodes have occurred while sitting at her desk at work, which she attributes to stress. The discomfort usually lasts 5-10 minutes and feels like muscle cramps. She has had no shortness of breath, palpitations, lightheadedness, syncope, or lower-extremity swelling. The patient has a history of diet-controlled diabetes mellitus diagnosed 20 years ago and anxiety disorder. She takes low-dose aspirin, lisinopril, and atorvastatin. She is a lifetime nonsmoker and drinks 1 or 2 glasses of wine during social gatherings. The patient has no known drug allergies. Her father was diagnosed with a myocardial infarction at age 60, and her mother died from a hemorrhagic stroke. Blood pressure is 125/80 mm Hg and pulse is 72/min. BMI is 29 kg/m2. Physical examination shows no abnormalities. ECG shows normal sinus rhythm with no abnormal repolarization changes. Serum creatinine is 1.1 mg/dL and hemoglobin A1c is 6.5%. Lipid panel shows LDL of 134 mg/dL and HDL of 45 mg/dL. The patient undergoes exercise stress testing. She exercises for 8 minutes without chest discomfort, and exercise ECG shows no abnormal ST-segment changes. Which of the following should be communicated to the patient regarding her stress testing results?
CorrectIncorrect -
Question 16 of 26
16. Question
A 57-year-old woman comes to the office for follow-up. The patient has a history of bicuspid aortic valve stenosis and underwent aortic valve replacement with a bileaflet mechanical valve 3 months ago. She had no operative complications and has had an uneventful postoperative course. The patient takes warfarin to prevent prosthetic valve thrombosis and reports feeling bothered by frequent laboratory testing and dietary restrictions to follow while taking warfarin. She has no other medical conditions. Vital signs are within normal limits. Physical examination demonstrates a mechanical heart valve sound with no murmur. The most recent echocardiography revealed a mildly enlarged left atrium, left ventricular ejection fraction of 60%, normally functioning mechanical aortic valve, and normal aortic root size. Which of the following is the best antithrombotic recommendation for this patient?
CorrectIncorrect -
Question 17 of 26
17. Question
A 63-year-old man comes to the office due to shortness of breath on mild exertion over the last 6 months. He has no chest pain, syncope, palpitations, or weight loss. The patient has ischemic cardiomyopathy, and he underwent coronary artery bypass grafting a year ago. He is receiving guideline-based optimal pharmacotherapy for heart failure. He appears comfortable at rest with no significant respiratory distress. Blood pressure is 122/80 mm Hg and pulse is 62/min and regular. Oxygen saturation is 96% on room air. S3 is heard at the apex. Scattered bibasilar crackles are heard at the lung bases. Abdominal examination is unremarkable. There is 1+ lower extremity edema bilaterally. Laboratory results are as follows:
Sodium
131 mEq/L
Potassium
4.2 mEq/L
Creatinine
1.2 mg/dL
Magnesium
2.5 mEq/L
Transthoracic echocardiography shows left ventricular dilation with a left ventricular ejection fraction of 25%. Which of the following ECG findings would be an indication for further management in this patient?
CorrectIncorrect -
Question 18 of 26
18. Question
A 65-year-old man is brought to the emergency department due to a 2-hour history of sharp, stabbing chest pain under his sternum. The patient was working outside in the yard when the symptoms started. The pain reached its maximum intensity within a few minutes and is now radiating to his upper back and shoulders. His medical history is significant for hypertension for the past 10 years. The patient has smoked 1.5 packs of cigarettes daily for the last 40 years. Blood pressure is 185/104 mm Hg in the right arm and 120/62 mm Hg in the left arm, pulse is 106/min and regular, and respirations are 18/min. Lungs are clear to auscultation bilaterally. Cardiovascular examination reveals a regular heart rhythm with an early diastolic murmur heard at the right sternal border. ECG shows sinus tachycardia and T-wave inversion in leads V5 and V6. Bedside transesophageal echocardiography confirms ascending aortic dissection with extension into the left subclavian artery. In addition to pain control, what is the best next step in management of this patient?
CorrectIncorrect -
Question 19 of 26
19. Question
A 55-year-old woman comes to the office for a preventive visit. She has no concerns at this time. The patient experienced a myocardial infarction 2 years ago. Current medications are metoprolol and aspirin. The patient does not smoke or use alcohol. Blood pressure is 125/80 mm Hg and pulse is 65/min. Physical examination is unremarkable. Fasting blood glucose level is 100 mg/dL. Laboratory results are as follows:
Total cholesterol
240 mg/dL
HDL cholesterol
40 mg/dL
LDL cholesterol
140 mg/dL
Triglycerides
400 mg/dL
The initiation of which of the following medications is most appropriate in this patient?
CorrectIncorrect -
Question 20 of 26
20. Question
A 36-year-old woman comes to the emergency department due to dry cough, wheezing, and shortness of breath that began 2 days ago and has progressively worsened. Medical history is remarkable for asthma that has been well controlled with an albuterol inhaler as needed. The patient also has hypertrophic cardiomyopathy that was diagnosed 3 years ago. Echocardiography 2 months ago showed dynamic left ventricular outflow obstruction causing exertional symptoms, and the patient was started on metoprolol at that time. Temperature is 37.1 C (98.8 F), blood pressure is 122/78 mm Hg, pulse is 90/min, and respirations are 24/min. Lung auscultation reveals poor air movement and moderate wheezing. Chest x-ray shows hyperinflation and is otherwise unremarkable. She is diagnosed with an acute asthma exacerbation. Metoprolol is stopped and she is started on intravenous corticosteroids and inhaled bronchodilators. Once the patient’s asthma exacerbation is stabilized, what is the best next step in management of her hypertrophic cardiomyopathy?
CorrectIncorrect -
Question 21 of 26
21. Question
A 64-year-old man comes to the office due to shortness of breath for the last 6 months. He describes his lifestyle as active but says, “I can’t catch my breath when I walk fast or climb the stairs. Six months ago, I felt completely fine.” He has no symptoms at rest or at night, and he has had no palpitations, chest pain, lightheadedness, syncope, or lower extremity swelling. The patient has a history of hypertension and diet-controlled type 2 diabetes mellitus. He also takes over-the-counter antacid for occasional heartburn. He is a lifetime nonsmoker and drinks beer over the weekend. The patient has no family history of heart attacks or sudden cardiac death, but his grandfather had a stroke in his 60s. Blood pressure is 149/86 mm Hg and pulse is 88/min and regular. Oxygen saturation is 97% on room air. Lungs are clear on auscultation. No heart murmurs are heard. There is no peripheral edema. ECG shows normal sinus rhythm, voltage criteria for left ventricular hypertrophy, and T-wave inversion in leads V5 and V6. Creatinine is 0.9 mg/dL and complete blood count is unremarkable. Echocardiogram shows a dilated left ventricle with ejection fraction of 38%. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 22 of 26
22. Question
A 29-year-old man comes to the emergency department due to sudden-onset chest pain over the past hour. He says, “I have this pressure and squeezing in my chest that does not go away.” He has never before had such symptoms. His medical history is insignificant. The patient smokes 2 packs of cigarettes daily and consumes alcohol occasionally. He uses cocaine and had “one shot” several hours ago. His family history is significant for a stroke in his father and a heart attack in his mother. Temperature is 36.7 C (98 F), blood pressure is 140/90 mm Hg, pulse is 112/min, and respirations are 24/min. ECG shows 2-mm ST-segment elevation in leads I, aVL, and V4-V6. The patient receives oxygen by mask, aspirin, and diazepam. He is given sublingual nitroglycerin and started on nitroglycerin infusion. Portable chest x-ray reveals a normal heart contour and clear lung fields. Twenty minutes later, he still has chest pain and his ECG is unchanged. The patient requests that he be given something to alleviate his chest discomfort. His initial troponin I level is undetectable. What is the best next step in management of this patient?
CorrectIncorrect -
Question 23 of 26
23. Question
A 42-year-old man is brought to the emergency department due to 4 hours of chest tightness and shortness of breath. He has not had similar symptoms before. He returned to the United States from a business trip to Paris a week ago. He thinks that his symptoms are due to an upper respiratory infection, which he suspects he contracted from recirculated air on the plane. The patient takes no medications and does not use alcohol or illicit drugs. He has a 20-pack-year smoking history. Blood pressure is 152/99 mm Hg and pulse is 92/min. BMI is 32 kg/m2. ECG is shown in the exhibit. Which of the following is the most appropriate next step in management of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 24 of 26
24. Question
A 66-year-old woman comes to the office to follow up for heart failure. Four weeks ago, she was diagnosed with new onset heart failure with reduced ejection fraction of 30%. At that time, ECG showed normal sinus rhythm, narrow QRS complexes, and T-wave inversion in the lateral leads. Coronary angiogram revealed no significant coronary artery disease. She is feeling better except for mild exertional fatigue. The patient typically uses 2 pillows to sleep and gets up once at night to urinate. She has no lightheadedness. Her only other medical condition is type 2 diabetes mellitus. Current medical therapy is sacubitril-valsartan, metoprolol succinate, and furosemide. Blood pressure is 109/60 mm Hg, pulse is 62/min, and respirations are 12/min. Pulse oximetry shows 98% on room air. Examination shows normal jugular venous pressure, clear lungs, and a 2/6 pansystolic murmur at the apex. The abdomen is soft and nontender. She has no peripheral edema. Laboratory results are as follows:
Serum chemistry
Sodium
142 mEq/L
Potassium
4.1 mEq/L
Chloride
106 mEq/L
Bicarbonate
28 mEq/L
Blood urea nitrogen
19 mg/dL
Creatinine
1.0 mg/dL
Calcium
9.6 mg/dL
Glucose
100 mg/dL
Which of the following is the most appropriate next step in pharmacotherapy management of this patient?
CorrectIncorrect -
Question 25 of 26
25. Question
A 55-year-old woman comes to the physician for a routine preventive examination. Her only symptoms are minor aches and pains in various muscles. She has been diagnosed with irritable bowel syndrome, fibromyalgia, depression, and rheumatic heart disease. Current medications include fluoxetine and ibuprofen. Temperature is 37.0 C (98.6 F), blood pressure is 128/86 mm Hg, pulse is 80/min, and respirations are 14/min. Heart auscultation shows a low-pitched, rumbling diastolic murmur preceded by an opening snap. The affected cardiac valve is best auscultated at which of the following regions?
CorrectIncorrect -
Question 26 of 26
26. Question
A 67-year-old man undergoes coronary angiography due to stable angina and a positive stress test. Medical history is notable for type 2 diabetes mellitus, hypertension, and peripheral arterial disease. Access is obtained through the right femoral artery, and a high-grade lesion is diagnosed in the mid left anterior descending artery. A drug-eluting stent is successfully placed. After the procedure, the femoral arterial sheath is removed and manual compression is applied. The patient is discharged the next morning. Two days later, he comes to the office for follow-up due to right groin pain and discomfort that he thought would be gone by now. He has no chest pain, dyspnea, lightheadedness, or abdominal pain. The patient has been taking dual antiplatelet therapy prescribed on discharge. Blood pressure is 118/74 mm Hg and pulse is 82/min. Physical examination shows mild swelling and bruising of the right groin with accentuated pulsation. Skin color and perfusion are normal over both lower extremities. Popliteal and dorsalis pedis pulses are symmetric. Which of the following is the best next step in management of this patient?
CorrectIncorrect
