Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 24-year-old woman is brought to the emergency department by her mother after an episode of witnessed seizure activity at home. The mother says the patient has a history of generalized tonic-clonic seizures. She had been seizure-free for the past 6 years and her antiepileptic medications were discontinued 2 years ago. Current medications include a daily multivitamin and an estrogen-progestin oral contraceptive pill. In the emergency department, the patient is given a loading dose of IV fosphenytoin and started on maintenance daily doses of oral phenytoin. Over the next 3 days, she has no seizures. On the fourth day, the patient develops a bothersome horizontal nystagmus. Her total phenytoin level on the same day is 20 µg/mL (normal: 10-20). Repeat blood work confirms the same level. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
An 85-year-old man is evaluated at a nursing home due to increasing agitation. The patient has dementia and has been residing at the facility for several years. At baseline, he can communicate his needs but does not recognize his caregivers and requires assistance with all activities of daily living. According to the staff, the patient usually becomes agitated in the evening. He has been receiving low doses of haloperidol or olanzapine as needed, but they have not controlled his symptoms, and the episodes of agitation have become somewhat more frequent recently. He has had no fever, cough, abdominal pain, urinary symptoms, or change in appetite. Medical records indicate a history of hypertension but no other medical conditions. The patient takes no additional medications. Temperature is 37 C (98.6 F), blood pressure is 130/70 mm Hg, and pulse is 78/min. He appears to be comfortable and is oriented to self only. Lungs are clear to auscultation, and heart sounds are normal. The abdomen is soft and nontender with normoactive bowel sounds. Neurologic examination shows mild resting hand tremors and rigidity of both arms. There is no extremity edema or rash. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
A 63-year-old man is brought to the emergency department due to sudden-onset speech slurring and right arm weakness. The symptoms began 90 minutes ago when he was giving a public speech at his local library. Medical history is significant for hypertension, obstructive sleep apnea, and erectile dysfunction. Temperature is 36.9 C (98.4 F), blood pressure is 240/130 mm Hg in both arms, pulse is 92/min, and respirations are 20/min. Cardiac telemetry reveals sinus rhythm. Finger-stick glucose level is 126 mg/dL. Serum chemistry, complete blood count, and coagulation panel are normal. Emergent noncontrast CT scan of the head reveals no abnormalities. Which of the following is the best initial step in management of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
A 25-year-old woman comes to the office due to episodes of bifrontal headaches, nausea, and blurred vision for the past 2 months. Blurred vision is occasionally accompanied by tunnel vision. Over-the-counter analgesic medications no longer relieve her headaches. The patient has no history of serious illness and takes no other medications. Menstrual cycles are irregular. She is not sexually active. The patient has had a 15-kg (33.1-lb) weight gain over the past year. BMI is 36 kg/m2. Temperature is 37 C (98.6 F), blood pressure is 124/78 mm Hg, pulse is 80/min, and respirations are 14/min. Pupils are equal and reactive to light. Funduscopic examination shows blurred optic discs. The remainder of the examination is normal. MRI of the head reveals no abnormalities. Lumbar puncture shows elevated opening pressure. In addition to recommendations regarding weight loss, treatment with a medication with which of the following mechanisms is most likely to relieve this patient’s symptoms?
CorrectIncorrect -
Question 5 of 40
5. Question
A 29-year-old man comes to the emergency department due to “shooting pains” in the bilateral lower extremities. The patient has not been feeling well for several days and has had progressively worsening back pain. He has a history of HIV, which was acquired via shared needles, but does not take antiretroviral therapy consistently. The patient still uses injection drugs occasionally but no longer shares needles. Temperature is 38 C (100.4 F), blood pressure is 116/68 mm Hg, and pulse is 98/min. The lungs are clear to auscultation, and heart sounds are normal with no murmurs. There is spinal tenderness to palpation over the T10 region. Neurologic examination reveals muscle strength of 4/5 in the bilateral lower extremities with upgoing bilateral plantar reflexes. What is the most likely cause of this patient’s current symptoms?
CorrectIncorrect -
Question 6 of 40
6. Question
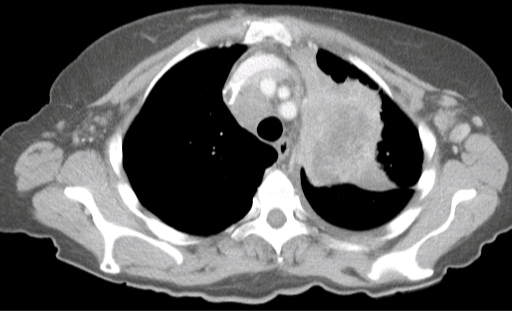
A 79-year-old man comes to the physician with his daughter for memory loss over the last 8-12 months. She initially noticed that he had trouble with forgetfulness, followed by distractibility and difficulty with word finding and object recognition. The patient is currently dependent on her for most independent activities of daily living, including transportation and finances. He is able to dress, bathe, and toilet himself. His gait has been unstable, and he sometimes seems to get “stuck in a chair.” On review of systems, he notes urinary urgency, frequency, and incontinence. He has a history of benign prostatic hyperplasia for which he takes tamsulosin. The patient has no tremor, problems with sleep, weakness, hallucinations, or sensory disturbances. On examination, his vital signs are normal. He is oriented to self only. On mental status examination, he has impairments in language, visuospatial skills, and executive function. His cranial nerves are intact. There is normal bulk and tone of the musculature. His gait is wide based and magnetic. He has decreased stride length and a slow turn requiring several steps. Laboratory results, including TSH and vitamin B12, are normal. Brain imaging is shown in the image below.

Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
A 32-year-old woman is hospitalized with left leg pain and swelling 2 weeks after an uneventful vaginal delivery of a healthy baby girl. She is diagnosed with a left lower extremity deep venous thrombosis and is started on intravenous heparin. A few hours later, she develops left-sided weakness and a facial droop. A non-contrast CT scan of the head reveals no intracranial bleeding but suggests an ischemic infarction in the territory of the right middle cerebral artery. Which of the following is most likely to reveal the cause of this patient’s symptoms?
CorrectIncorrect -
Question 8 of 40
8. Question
The following vignette applies to the next 2 items.
A 79-year-old man is brought to the office by his daughter. The patient has been having increasing difficulty caring for himself over the last 2 years. He is now dependent on his daughter for meal preparation, shopping, and cleaning. He will frequently go a week without bathing and often has difficulty dressing himself appropriately. The patient sometimes grows frustrated and shouts at his daughter but has never been physically violent. On direct questioning, he states that he feels fine, does not see any reason for coming to the office, and is quite suspicious of his daughter’s motives. The patient has lived alone since his wife died 5 years ago. He has hypertension, osteoarthritis, and a history of remitted major depressive disorder. Medications include hydrochlorothiazide and acetaminophen as needed. Neurologic examination is nonfocal.
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
Item 2 of 2
The patient scores 20 out of 30 on the Montreal Cognitive Assessment. Neuroimaging studies reveal diffuse cortical atrophy. The laboratory workup is unremarkable. Which of the following is the most appropriate next step in pharmacotherapy?
CorrectIncorrect -
Question 10 of 40
10. Question
The following vignette applies to the next 5 items.
A 22-year-old woman comes to the physician with her husband for intermittent dizziness, weakness, and unsteady gait for the last several weeks. She has also had visual loss and pain in the right eye that worsens with eye movement for the past 2 days. A year ago, the patient had tingling and numbness of her right hand accompanied by unsteadiness, which improved spontaneously after 3-4 days. She has no other medical problems and does not take any medications. The patient has no significant social or family history. Her temperature is 37.2 C (99 F), blood pressure is 122/80 mm Hg, pulse is 82/min, and respirations are 16/min. On neurologic examination, her right eye has diminished visual acuity and an afferent pupillary defect. She also has a right arm intention tremor. Both lower extremities have spastic paresis, hyperreflexia, and positive Babinski sign.
Item 1 of 5
Which of the following is the most appropriate test to confirm the diagnosis in this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
Item 2 of 5
Appropriate investigation has confirmed the most likely diagnosis. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 12 of 40
12. Question
Item 3 of 5
The patient has marked symptomatic improvement within a few days of initial treatment and is scheduled for physical therapy. Which of the following is the most appropriate long-term pharmacotherapy for this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
Item 4 of 5
Four months later, the patient comes to the physician for a routine visit and asks for advice regarding pregnancy. She has been taking her medication regularly. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 14 of 40
14. Question
Item 5 of 5
The patient returns to the physician due to painful muscle spasms. She has frequent episodes of pain and stiffness in both legs, especially when rising from her bed. She has tried home stretching exercise without significant relief. The patient is afebrile and has no new neurological deficits. Increased muscle tone is noted in the lower extremities. Laboratory evaluation, including electrolytes, is normal. Which of the following is the most appropriate next step in managing this patient’s current symptoms?
CorrectIncorrect -
Question 15 of 40
15. Question
A 22-year-old Caucasian female is brought to your office by her boyfriend after he found her unconscious on the bed. He says that he is unaware of her past medical history, but remembers one similar episode that resolved completely. Her temperature is 36.7 C (98 F), blood pressure is 130/80 mm Hg, pulse is 90/min, and respirations are 18/min. The patient is unresponsive to verbal and tactile stimuli. Physical examination reveals a symmetric decrease in muscular tone and normal deep tendon reflexes. Pupils are symmetric, 5mm, and reactive to light. Irrigation of the right external auditory canal with cold water reveals a transient, conjugate, slow deviation of gaze to the right, followed by saccadic correction to the midline. Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 16 of 40
16. Question
A 63-year-old Caucasian male is being evaluated for difficulty sleeping and morning headaches. He has been sleeping upright for the last two months because he gets short of breath while lying flat. He has also had mild dysphagia and difficulty walking for the last six months. He denies any chest pain, palpitations, wheezing, cough, or lower extremity swelling. His blood pressure is 127/86 mmHg and heart rate is 96/min, regular in rhythm. His BMI is 27 kg/m2. Physical examination reveals some lower extremity muscle atrophy and tongue fasciculations. There are minimal crackles at the right lung base. His forced vital capacity is 57% of the predicted value while upright and 42% of the predicted value while supine. Which of the following is the most likely cause of this patient’s dyspnea?
CorrectIncorrect -
Question 17 of 40
17. Question
A 65-year-old woman comes to the office with several months of progressive cough and generalized weakness. The patient has limited mobility and shortness of breath due to osteoarthritis and chronic obstructive pulmonary disease, respectively. She also has difficulty standing from a chair, combing her hair, and putting dishes in overhead cabinets. The patient’s medical history includes hypertension and hyperlipidemia. She quit smoking cigarettes 2 years ago but previously smoked 3 packs daily since age 20. Blood pressure is 112/70 mm Hg, and pulse is 92/min. BMI is 17 kg/m2. Physical examination shows moderate weakness in the proximal muscles of her upper and lower limbs and loss of deep tendon reflexes. CT scan of the chest is shown below.
Which of the following is the most likely cause of this patient’s weakness?
CorrectIncorrect -
Question 18 of 40
18. Question
A 60-year-old man is brought to the office by his wife due to behavior changes over the past year. The patient’s wife says that her husband started to become emotionally “cold” and less affectionate toward her but has received several complaints at work for flirting with customers. She says, “He doesn’t care about anything anymore and could even lose his job. We rarely leave the house now because he keeps urinating in the street right in front of people.” Over the past 6 months, the patient has had restless sleep and has begun to exhibit memory difficulties, including getting lost a few times while driving home from work. His wife also notes that he never used to like sweets but can now eat an entire box of chocolates and still want more. Family medical history is significant for major depressive disorder in his father, who completed suicide at age 45. Medical history includes hypertension and hyperlipidemia. Vital signs are within normal limits. Cardiopulmonary examination is normal. Neurologic examination shows 3+ reflexes in the upper and lower extremities, and fasciculations are observed in the left arm. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 19 of 40
19. Question
A 61-year-old military veteran comes to the emergency department for a sudden onset of difficulty speaking and right arm tingling. The symptoms started abruptly 2 hours ago, when he was practicing for a speech. The patient states, “After this started, I had trouble finding the words I wanted to say. I’m worried because I give motivational speeches for a living.” He does not have visual changes or muscle weakness. Medical history includes hypertension. The patient takes lisinopril, hydrochlorothiazide, and a daily baby aspirin. He smokes 5-10 cigarettes a day. Temperature is 37.2 C (99 F), blood pressure is 160/84 mm Hg, pulse is 74/min, and respirations are 16/min. The patient is awake and alert, pupils are normal, and visual fields are intact. He can speak in full sentences but has difficulty finding certain words. The patient is unable to name several of the objects shown to him. He follows commands without hesitation. Strength is 5/5 in his upper and lower extremities. Sensation is normal. Finger-to-nose and heel-to-shin tests are normal. Blood glucose is normal. Noncontrast CT scan of the head is normal, and CT angiography of the head and neck demonstrates no large-vessel occlusion. Which of the following is the most accurate statement regarding thrombolytic therapy in this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 62-year-old man comes to the office due to occasional episodes of double vision over the last 2 months. The patient has no headaches, nausea, vomiting, or imbalance and has had no falls. Medical history includes type 2 diabetes mellitus, hyperlipidemia, and a transient ischemic attack 6 months ago for which he underwent a left carotid endarterectomy. Medications include metformin, atorvastatin, and aspirin. Blood pressure is 124/78 mm Hg and pulse is 86/min. On examination, mild ptosis is present on the left side. There is weakness of abduction and adduction of the left eye. Pupillary reflexes are normal. Visual acuity is 20/20 with the patient’s glasses; visual fields are full in both eyes. Muscle strength is 5/5 in the extremities. Deep tendon reflexes and sensation are normal. Hemoglobin A1c is 7.3%. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 21 of 40
21. Question
A 64-year-old man comes to the office due to slowing of his movements and gait instability that has contributed to several recent falls. The patient was diagnosed with Parkinson disease a year ago. On physical examination, there is a resting tremor involving the right hand and rigidity during passive flexion and extension of the right upper limb. The patient is started on therapy with pramipexole. Which of the following best describes the mechanism of action of this medication?
CorrectIncorrect -
Question 22 of 40
22. Question
A 58-year-old man is brought to the emergency department due to acute left-sided weakness that began an hour ago. The patient was typing on his computer at work when he suddenly was unable to use his left hand. As he tried to stand up, he fell due to left leg weakness. He has not had any visual changes or difficulty with speech. He has no significant medical history and takes no medications. He consumes 3 or 4 alcoholic beverages daily and does not use tobacco. Temperature is 37.2 C (99 F), blood pressure is 135/80 mm Hg, pulse is 120/min, and respirations are 14/min. The patient is awake and alert. Visual fields are intact. There is a left-sided facial droop, and strength is 3/5 in the left arm and leg; sensation is intact. There is no aphasia or evidence of neglect. Heart sounds are rapid and irregular. Noncontrast CT scan of the head is normal, and simultaneous CT angiogram reveals no large vessel occlusion. ECG is shown in exhibit. What is the best next step in management of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 14-year-old girl is brought to the office due to recurrent headaches. The headaches began 2 weeks ago while she was studying for end-of-semester examinations. Since then, the patient has had headaches almost daily but has been able to continue school and other daily activities. The headaches are of moderate intensity, bifrontal, nonthrobbing, exacerbated by loud noise, and relieved by sleep and ibuprofen. The patient has had no nausea or vomiting. Her mother has a history of migraine. Vital signs are within normal limits. BMI is 28 kg/m2. Nasal and oropharyngeal mucosae and tympanic membranes are normal. Neurologic examination shows normal bilateral pupillary response and normal motor strength, sensation, and deep tendon reflexes. There is no neck rigidity. Which of the following is the most likely cause of this patient’s headaches?
CorrectIncorrect -
Question 24 of 40
24. Question
A 58-year-old man comes to the emergency department due to a 2-day history of progressively increasing right-sided headache, a daylong history of diplopia, and a droopy right eyelid. Medical history is significant for hypertension, for which the patient takes amlodipine. He has smoked 1 pack a day for 30 years. Temperature is 37.1 C (98.8 F), blood pressure is 140/72 mm Hg, and pulse is 86/min. The patient is alert and oriented with normal mental status. There is mild neck stiffness. The skin is well perfused with no rashes. There is partial ptosis of the right eye with deficits in right eye adduction, abduction, elevation, and depression. Left eye movements and the rest of the neurologic examination, including cranial nerves, visual fields, upper and lower extremity strength and sensation, and reflexes, are normal. Cardiovascular, respiratory, abdominal, and ENT examinations are also normal. Complete blood count is normal. What is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 62-year-old hospitalized woman is evaluated for muscle weakness. The patient was admitted 2 weeks ago due to septic shock from acute pyelonephritis. She was treated in the intensive care unit with intravenous fluids, vasopressors, and broad-spectrum antibiotics. The patient was also mechanically ventilated due to respiratory failure. Her hemodynamic status and infection gradually improved, but she has had difficulty being taken off the ventilator due to respiratory muscle weakness. She is also noted to have significant extremity weakness. Physical examination shows diffuse mild atrophy of the extremity muscles. Bilateral upper and lower extremity deep tendon reflexes are decreased. Which of the following is the most likely cause of this patient’s current condition?
CorrectIncorrect -
Question 26 of 40
26. Question
An 81-year-old woman is brought to the office for assessment of behavioral changes over the past 10 months. The patient moved to a nursing home a year ago, and initially enjoyed playing simple card games there with other residents. Now she either seems uninterested in playing or quickly becomes upset during games, repeating, “I can’t, I can’t, I can’t.” She also becomes easily irritable and pushes staff away when they try to help her dress or comb her hair. The patient has had increasing difficulty recalling recent events and has started accusing staff of stealing her jewelry. Sleep and appetite are unchanged. The patient has a history of hypertension and noninsulin-dependent diabetes mellitus, as well as postpartum depression in her 20s. Temperature is 37 C (98.6 F), blood pressure is 140/90 mm Hg, and pulse is 86/min. Physical examination is unremarkable. She is oriented to person and place but not to time or day. Short-term recall is very poor. Her mood is “OK.” Laboratory results, including electrolytes, complete blood count, thyroid function tests, and vitamin B12, are normal. Rapid plasma reagin is negative; fluorescent treponemal antibody absorption test is nonreactive. MRI of the brain reveals mild generalized cortical atrophy and slightly reduced hippocampal volume. Which of the following is the most appropriate statement regarding this patient’s prognosis?
CorrectIncorrect -
Question 27 of 40
27. Question
A 21-year-old man comes to the clinic due to weakness and gait disturbance. For the past few months, he has noticed difficulty opening the lids on jars, along with trouble releasing his grip afterward. The patient has also tripped and fallen several times, particularly when walking up stairs. He has no known chronic medical conditions and takes no medications. Vital signs are normal. The patient has male pattern baldness. Cardiopulmonary examination is unremarkable. The abdomen is soft with no organomegaly. A muscle biopsy shows muscle atrophy involving mostly type 1 fibers. This patient most likely has a form of which of the following neuromuscular diseases?
CorrectIncorrect -
Question 28 of 40
28. Question
A 71-year-old man is brought to the emergency department by his daughter for evaluation of an episode of slurred speech and right upper extremity weakness. The symptoms began approximately 3 hours ago and lasted an hour. He had no associated headache, chest pain, palpitations, shortness of breath, or syncope. The patient has had no similar episodes in the past. He now feels well. Medical history is significant for hypertension. He has a 60-pack-year smoking history but quit 8 years ago. The patient’s mother had atrial fibrillation. Blood pressure is 162/96 mm Hg and pulse is 92/min. BMI is 33 kg/m2. Auscultation of the upper anterior cervical triangle on the left side of the neck reveals a bruit. Neurologic examination is normal. No lower extremity edema is present. Low-density lipoprotein cholesterol is 110 mg/dL. ECG shows normal sinus rhythm and nonspecific ST-segment and T-wave changes. MRI of the brain shows mild age-related changes but no areas of restricted diffusion. MR angiogram reveals 75% stenosis of the proximal left internal carotid artery and normal intracerebral vessels. Echocardiography shows left ventricular hypertrophy, normal left ventricular function, and mild left atrial enlargement. A patent foramen ovale is detected via agitated saline study. Lower extremity ultrasound is negative for deep vein thrombosis. He is started on aspirin and rosuvastatin. Which of the following is the best management strategy for this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
A 66-year-old man comes to the emergency department with progressive lower back pain, urinary incontinence, and decreased appetite for the past 2 days. The patient was recently diagnosed with L4-L5 disc herniation and received an epidural injection for radicular pain 2 weeks ago. Other medical concerns include type 2 diabetes mellitus and hypertension. Temperature is 38.3 C (100.9 F), blood pressure is 136/88 mm Hg, pulse is 96/min, and respirations are 14/min. The patient is alert and oriented. Physical examination shows poor dentition, tenderness on palpation of the lumbar spine, and absent deep tendon reflexes in both lower extremities. Rectal examination shows decreased rectal sphincter tone and an enlarged, smooth prostate. Laboratory results are as follows:
Leukocytes
25,000/mm3
Segmented neutrophils
69%
Bands
7%
Erythrocyte sedimentation rate
104 mm/hr
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 68-year-old man comes to the office due to worsening back pain. The patient has a history of severe lumbar degenerative disc disease that limits his daily activities. He declined surgery, and treatment with nonpharmacologic interventions and nonopioid analgesics have not adequately controlled the pain. The patient began taking long-acting oxycodone 5 months ago with good pain control. Over the past 2 months, he reports progressive worsening of the pain despite a modest increase in dose. The patient also takes acetaminophen for breakthrough pain and an osmotic laxative for constipation. Physical examination shows lower paraspinous tenderness but no lower extremity neurologic deficits. Spine imaging shows no significant changes from previous studies. Which of the following is the most likely reason for decreased analgesic efficacy in this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 52-year-old woman comes to the emergency department due to recurrent right lower extremity swelling, pain, and erythema. The patient’s medical history includes type 2 diabetes mellitus and depression. Her medications include metformin, paroxetine, and a multivitamin. The patient is diagnosed with cellulitis, admitted to the hospital, and started on antibiotics. She is continued on her home medications. Three days later, the patient becomes agitated and delirious with severe abdominal cramps and diarrhea. Her temperature is 39.2 C (102.6 F), blood pressure is 180/100 mm Hg, and heart rate is 120/min and regular. On examination, the patient is diaphoretic and tremulous, and her pupils are dilated. Bilateral hyperreflexia and ankle clonus are present. She begins to have seizures. Which of the following antibiotics was the patient most likely given to treat the cellulitis?
CorrectIncorrect -
Question 32 of 40
32. Question
A 35-year-old woman is brought to the emergency department due to a 4-day history of headache, dizziness, and loss of balance resulting in multiple falls. She reports marked fatigue, urinary frequency, nocturia, and the perception of a band-like tightness around her umbilical region. Temperature is 36.9 C (98.4 F), blood pressure is 114/76 mm Hg, and pulse is 76/min. BMI is 27 kg/m2. Examination shows slow eye adduction and lateral gaze nystagmus bilaterally. Funduscopy is normal. Finger-nose testing demonstrates dysmetria on the left. Speech is dysarthric. Muscle strength is 5/5 in the upper extremities and 4/5 in the lower extremities. Muscle tone is increased in the lower extremities. Deep tendon reflexes are 2+ in the upper extremities and 3+ in the lower extremities. Babinski sign is present bilaterally. Sensations are decreased on the right side of the face and below T10. Gait is unsteady and spastic. Examination of this patient’s cerebrospinal fluid is most likely to show which of the following?
CorrectIncorrect -
Question 33 of 40
33. Question
The following vignette applies to the next 2 items.
A 65-year-old man was admitted to the intensive care unit after going into cardiac arrest when alone at home. Cardiopulmonary resuscitation and advanced cardiac life support were performed extensively in the field, and return of spontaneous circulation was eventually achieved. Two days later, he remains intubated and is on full ventilator support. The patient is unresponsive to verbal and tactile stimuli. His temperature is 37.2 C (99 F), blood pressure is 110/70 mm Hg, and pulse is 70/min. The treating physician discusses with the patient’s family the possibility of brain death.
Item 1 of 2
Which of the following is most consistent with the criteria for brain death?
CorrectIncorrect -
Question 34 of 40
34. Question
Item 2 of 2
The patient is diagnosed with brain death based on apnea testing and in accordance with local regulations. The physician explains this finding to the patient’s family and discusses withdrawing of mechanical ventilator support. Everyone in the family appears to understand and agrees to proceed with withdrawing ventilatory support. A relative then walks into the patient’s room and notices some movements in the patient’s legs and toes. The relative believes the patient is not dead and gets angry with the treating physician. Which of the following is the most appropriate response to the relative’s reaction?
CorrectIncorrect -
Question 35 of 40
35. Question
A 32-year-old man comes to the office for a routine follow-up visit. He was diagnosed with epilepsy three years ago, and has been taking carbamazepine 800 mg/day ever since. He does not use tobacco, alcohol or recreational drugs. His family history is not significant. Physical examination shows no abnormalities. The patient is concerned about the potential side effects of his medication. Which of the following complications is this patient at greatest risk for?
CorrectIncorrect -
Question 36 of 40
36. Question
The following vignette applies to the next 2 items
A 62-year-old Caucasian man comes to the physician because of progressive weight loss and right lower extremity weakness for the last two months. On further questioning, he tells you that he has been having frequent leg cramps in the right leg. These cramps are most prominent in the morning, after he wakes up. He also has difficulty with swallowing and chewing. He denies any problems with bowel or bladder function. His other medical problems include hypertension and hypercholesterolemia. He does not use tobacco. His family history is not significant. His vital signs are within normal limits. The physical examination reveals weakness in his right lower leg, atrophy and fasciculation of the thigh and calf muscles, a hyperactive knee jerk, and tongue fasciculations. The rest of his neurological examination, including the sensory examination, is normal.
Item 1 of 2
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 37 of 40
37. Question
Item 2 of 2
Which of the following treatment has been shown to be beneficial in these patients?
CorrectIncorrect -
Question 38 of 40
38. Question
The following vignette applies to the next 2 items.
A 78-year-old woman is brought to the office by her son due to progressive forgetfulness over the last year. She has been less active than normal and is having some difficulty walking. The patient has no urinary incontinence. Medical history is significant for exertional angina and hypertension. She has recently been depending on her son to manage her medications, which include metoprolol, amlodipine, rosuvastatin, and aspirin. She does not smoke or consume alcohol. Her father had hypertension and stroke, and her mother had Alzheimer dementia. The patient is oriented to person and place, but not time. She has difficulty with 3-word recall. Her gait is slightly unstable, and she has problems balancing when she closes her eyes. Examination of the lower extremities shows decreased vibratory sensation, spastic paresis, and hyperreflexia bilaterally.
Item 1 of 2
What is the most likely cause of this patient’s condition?CorrectIncorrect -
Question 39 of 40
39. Question
Item 2 of 2
Further evaluation of the patient shows mild indirect hyperbilirubinemia. Which of the following is the most likely explanation of this finding?CorrectIncorrect -
Question 40 of 40
40. Question
A 78-year-old woman is brought to the emergency department after her neighbor found her slumped over on her front porch bench, unable to speak or walk. The neighbor reports that, 2 hours prior, he had seen the patient walking to her mailbox. He spoke with her for a few minutes, and she seemed normal at that time. The patient lives alone but has an adult daughter in another town. Vital signs are normal. Neurologic examination demonstrates right-sided hemiparesis and aphasia. The patient is a candidate for thrombolysis but does not appear to understand when the risks and benefits of thrombolysis are discussed. The daughter could not be reached by phone on the initial attempt. Which of the following is the most appropriate next step regarding consent for thrombolysis in this patient?
CorrectIncorrect
