Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 41-year-old woman, gravida 3 para 3, comes to the office due to a lump in her right breast. She noticed the mass last week. The lump has not grown, and there is no associated nipple discharge, breast pain, or skin rash. The patient has no chronic medical conditions. Menstrual periods are now regular, occurring every 28 days with 5 days of moderate bleeding. The patient is sexually active and underwent a bilateral tubal ligation with her last delivery. She takes ibuprofen occasionally and has no medication allergies. The patient does not use tobacco, alcohol, or recreational drugs. Her maternal grandmother died of breast cancer at age 62; family history is otherwise unremarkable. Vital signs are normal. BMI is 28 kg/m2. Examination reveals a firm, ill-defined, 2-cm mass in the upper outer quadrant of the right breast. Bilateral breasts have no nipple retraction or expressed discharge. No axillary or supraclavicular lymphadenopathy is present. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
A 32-year-old woman comes to the office due to heavy vaginal bleeding. For the past 6 months, the patient has had regular menses every 30 days, with 7 days of painful cramping, heavy vaginal bleeding, and passage of large clots. She uses both a tampon and a sanitary napkin simultaneously to prevent blood from staining her underwear and soaking through her clothes. The patient has had no intermenstrual bleeding or abnormal vaginal discharge. Her last menstrual period ended a week ago. Menses previously consisted of 5 days of mild cramping with moderate bleeding. The patient is sexually active and uses condoms and spermicide for contraception. She does not desire pregnancy now but would like to attempt to conceive in the next few years. Blood pressure is 100/70 mm Hg and pulse is 84/min. BMI is 23 kg/m2. Pelvic examination reveals a 14-week-sized, irregularly shaped uterus with no cervical motion tenderness or adnexal masses. Hemoglobin is 9.8 g/dL. A urine pregnancy test is negative. Pelvic ultrasound shows a large uterus with several subserosal and intramural leiomyomas; the endometrial stripe appears smooth and homogeneous. The patient asks what can be done to treat her condition. Which of the following is the most appropriate management at this time?
CorrectIncorrect -
Question 3 of 40
3. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 19-year-old woman comes to the student health center after a sexual assault 2 days ago. She has no fever, chills, abdominal pain, or abnormal vaginal discharge. The patient was sexually assaulted by a man she has seen multiple times who also attends the university. Menses are regular and occur every 29 days; her last menstrual period was 2 weeks ago. She has no known medical conditions and has had no surgeries. The patient takes no medications and has no drug allergies. She smokes cigarettes and drinks alcohol socially. There is no family history of illness. She is sexually active with a long-term male partner, and they use condoms for contraception. The patient has no history of sexually transmitted infections. Temperature is 36.7 C (98.1 F), blood pressure is 110/70 mm Hg, and pulse is 65/min. BMI is 20 kg/m2. The abdomen is soft and nontender, with no palpable masses. Bruises and abrasions are present over the inner thighs, perineum, and vulva. Pelvic examination reveals yellow vaginal discharge and a friable cervix that bleeds easily on contact. The vaginal mucosa is erythematous with no evidence of hematoma. The uterus is small and nontender on bimanual examination; no adnexal masses are palpated. Microscopy of the discharge shows an abundance of polymorphonuclear leukocytes. Urine pregnancy test is negative.
Item 1 of 2
A sexual assault forensic examination is performed, and evidence is collected. In addition to providing psychosocial support, which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
Item 2 of 2
The patient undergoes a sexually transmitted infection workup, which includes viral hepatitis, HIV, syphilis, chlamydia, and gonorrhea. She completed a hepatitis B vaccination series at age 18 prior to attending the university, and all other vaccines are up to date. Based on her history and examination, which of the following medications should be administered?
CorrectIncorrect -
Question 5 of 40
5. Question
A 26-year-old woman, gravida 1 para 1, comes to the office for a contraception counseling visit. The patient has been using a progestin-only pill for contraception since giving birth a year ago. She would like to switch to a combined hormonal contraceptive as she is no longer breastfeeding. The patient has no chronic medical conditions and takes no other daily medications. Vital signs and physical examination are unremarkable. Which of the following is the primary mechanism of pregnancy prevention when the patient switches to a combined hormonal contraceptive?
CorrectIncorrect -
Question 6 of 40
6. Question
A 26-year-old woman, gravida 0 para 0, comes to the community health center for an annual physical examination. She is concerned because her grandmother recently died of metastatic breast cancer at age 68. The patient states, “Ever since my grandmother died, I have been worried about breast cancer. I think I need a mammogram to ensure that I don’t have cancer.” She has no chronic medical conditions and has had no surgeries. Her periods are regular, every 28 days with 4 days of moderate bleeding; the last menstrual period was 2 weeks ago. Menarche was at age 13. The patient is sexually active without contraception and is planning a pregnancy within the year. Other than breast cancer in her paternal grandmother, family history is noncontributory. The patient takes a daily prenatal vitamin and does not use tobacco, alcohol, or recreational drugs. Temperature is 36.7 C (98 F), blood pressure is 110/70 mm Hg, and pulse is 70/min. BMI is 20 kg/m2. Breast examination shows no masses bilaterally, and the right breast is slightly larger than the left. No nipple discharge, skin dimpling, rash, or lymphadenopathy is present. She notes that the breast asymmetry has been present since puberty. Which of the following is the most appropriate response to this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
A 6-year-old girl is brought to the office by her parents for evaluation of breast development that her mother noticed while helping her daughter dress. The mother reports undergoing menarche at age 14 but says that her daughter had some spotting a month ago that resolved on its own. The girl has no chronic medical conditions and takes no daily medications. Height, weight, and BMI track along the >90th percentile, unchanged from previous visits. Physical examination shows Tanner stage 3 breast development and Tanner stage 1 pubic hair. The breasts have no palpable masses. External genitalia are normal. Radiographic imaging reveals advanced bone age. Laboratory results are as follows:
Endocrine
FSH, serum
0.5 mU/mL (normal: 0.72-5.33)
LH, serum
0.15 mU/mL (normal: ≤0.26)
Estradiol
95 pg/mL (normal: <5)
Testosterone
12 ng/dL (normal: ≤20)
Which of the following is the most appropriate next step in evaluation of this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
A 60-year-old woman comes to the office due to new-onset pelvic pressure. The patient reports increasing pelvic pressure over the last 3 months, now with associated urinary frequency. She has no abdominal pain, dysuria, or hematuria. The patient reports some dyspnea on exertion; review of systems is otherwise negative. The patient has a history of breast cancer at age 45; it was treated with radical mastectomy, chemotherapy, and adjuvant tamoxifen therapy. The cancer has since been in remission and she had a normal mammogram last year. The patient has no other chronic medical conditions. She underwent menopause 8 years ago and has had no episodes of postmenopausal vaginal bleeding. The patient has had no abnormal Pap tests, the last of which was 3 years ago. She does not use tobacco, alcohol, or illicit drugs. Blood pressure is 130/80 mm Hg, pulse is 80/min, and respirations are 18/min. BMI is 26 kg/m2. Decreased breath sounds are noted over the lower base of the right lung. Abdominal examination reveals normoactive bowel sounds and mild distension but no tenderness. On bimanual examination, a 12-week-sized, irregularly shaped uterus is noted, but there are no adnexal masses. Urinalysis is within normal limits. Pelvic ultrasound shows a dense focal mass measuring 9 cm in the anterior fundus of the uterus, normal ovaries bilaterally, and a moderate amount of free fluid in the posterior cul-de-sac. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 48-year-old woman comes to the office for the treatment of abnormal uterine bleeding. The patient has had menstrual bleeding every 2-3 weeks and often has 6-7 days of bleeding. She typically has to change her menstrual pad every 3 hours and occasionally passes multiple small blood clots. The patient has no associated fatigue, shortness of breath, or pelvic pain. The patient’s medical conditions include hypertension, atrial fibrillation, congestive heart failure, and type 2 diabetes mellitus. On pelvic examination, the uterus is slightly enlarged with an irregular fundal contour reaching just above the pubic symphysis. Hematocrit level is 36%. A complete work-up, including endometrial biopsy and pelvic ultrasound, is consistent with uterine fibroids. The patient demands a hysterectomy because she wants “to be completely done with this problem” and does not think that medical management will work for her. The physician states that the surgery is not indicated and refuses to perform the hysterectomy. Which of the following ethical principles is this physician employing by not performing surgery on this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
A 26-year-old woman is brought to the emergency department due to lower abdominal pain for the past 2 days. She reports intractable nausea and vomiting over the past day but has had no fever, chills, sick contacts, or diarrhea. The patient recently received an hCG injection for egg retrieval for infertility. Since the procedure, she has gained 3.6 kg (8 lb). The patient has a history of polycystic ovary syndrome and has had no surgeries. Blood pressure is 90/50 mm Hg and pulse is 110/min. BMI is 35 kg/m2. Physical examination shows a distended abdomen with normal bowel sounds and diffuse lower abdominal tenderness to deep palpation. There is no rebound, guarding, or costovertebral angle tenderness.
Complete blood count
Hematocrit
46%
Leukocytes
16,000/mm3
Serum chemistry
Creatinine
1.4 mg/dL
Urine pregnancy test is positive. Transvaginal ultrasound shows bilateral ovarian enlargement with multiple cysts measuring up to 8 × 8 cm and intraabdominal fluid consistent with ascites. Doppler shows preserved blood flow to both ovaries. Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 11 of 40
11. Question
A 30-year-old woman, gravida 3 para 0 aborta 3, comes to the office due to a history of recurrent spontaneous abortions. The patient has had 3 first trimester spontaneous abortions in the past 2 years that did not require medical or surgical management. Her menses occur every 30 days and consist of 4-5 days of moderate bleeding and mild cramping. Her Pap tests have been normal, and she has never had a sexually transmitted infection. The patient has no chronic medical conditions and takes no medications. She had a laparoscopic right ovarian cystectomy at age 18 for a large, benign cyst. She drinks alcohol on special occasions, but does not use tobacco or recreational drugs. She practices yoga 4-5 times a week. Blood pressure is 120/70 mm Hg and pulse is 74/min. BMI is 26 kg/m2. Bimanual examination reveals a smooth, normal-sized, nontender uterus and no adnexal masses or tenderness. Speculum examination shows minimal physiologic cervical discharge and a cervix with no visible lesions. Laboratory evaluation is normal. A hysterosalpingogram shows a filling defect in the middle of the uterine cavity and bilaterally patent fallopian tubes. Her husband has a healthy daughter from a prior relationship and recently had a semen analysis that was normal. The patient asks what can be done to prevent another miscarriage. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 12 of 40
12. Question
An 86-year-old woman comes to the office due to a vaginal bulge and difficulty urinating. The patient first noticed the bulge several years ago but did not seek care. Over the last few months, as the bulge has enlarged, she has experienced increasing pelvic pressure. In addition, she now has to manually elevate the bulge to urinate. The patient has no vaginal bleeding or difficulty with defecation. She has chronic obstructive pulmonary disease managed with an inhaled combined long-acting beta agonist and corticosteroid. She had 2 vaginal deliveries in her early 20s; the second was complicated by a fourth-degree perineal laceration. The patient has a 50-pack-year smoking history, but quit 15 years ago; she does not use alcohol or illicit drugs. Blood pressure is 150/90 mm Hg, pulse is 78/min, respirations are 20/min, and pulse oximetry is 91% on room air. BMI is 34 kg/m2. Auscultation of the lungs reveals decreased breath sounds bilaterally. Pelvic examination reveals anterior vaginal wall prolapse and protrusion of the cervix through the vaginal introitus. During the examination, the uterus is elevated and the prolapse is reduced; the patient is asked to cough and no leakage of urine is observed. Post-void residual urine volume is 40 mL. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
A 41-year-old woman, gravida 1 para 1, comes to the office for persistent vaginal spotting and lower abdominal pain following an uncomplicated delivery 4 months ago. Since then, she has had bloody discharge of decreasing volume that has not completely resolved. For the past month, the patient has used a sanitary pad that is stained but not saturated with blood at the end of the day. The abdominal pain has been mild but constant and is minimally relieved by over-the-counter analgesics. The patient’s last Pap test, during her initial prenatal visit, was normal. Human papillomavirus testing at that time was negative. She is breastfeeding her infant, who is doing well. The patient is a former smoker who has not used alcohol since prior to pregnancy and does not use illicit drugs. Temperature is 36.7 C (98.1 F), blood pressure is 110/70 mm Hg, pulse is 68/min, and respirations are 18/min. BMI is 30 kg/m2. Abdominal examination reveals mild lower abdominal tenderness to deep palpation but no masses, rebound, or guarding. Pelvic examination reveals an enlarged uterus and no adnexal masses. Speculum examination shows a dark, irregular 2-cm lesion on the posterior fornix that bleeds after contact with an applicator, with scant blood in the vaginal vault. A urine pregnancy test is positive. Which of the following is the most likely diagnosis for this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 76-year-old woman, gravida 4 para 4, comes to the office with pelvic pressure and heaviness, lower back pain, and constipation. Her constipation has not improved with daily laxative use. She has no melena, hematochezia, or changes in stool caliber. The patient has hypertension and peptic ulcer disease controlled with oral medications. Surgical history is significant only for an appendectomy. A screening colonoscopy performed 2 years ago was negative. Her mother had coronary artery disease and died from a myocardial infarction. The patient has a 52-pack-year smoking history and occasionally drinks hard liquor. Temperature is 36.7 C (98 F), blood pressure is 140/90 mm Hg, and pulse is 72/min. Pulse oximetry is 98% on room air. BMI is 35 kg/m2. Cardiac examination reveals a normal rate and rhythm; there are no rubs, murmurs, or gallops. Pulmonary examination reveals decreased breath sounds in bilateral lung bases. On pelvic examination, a protrusion of the posterior vaginal wall expands with increased intraabdominal pressure and with standing. The patient is bothered by these symptoms. Which of the following is the most accurate statement regarding this patient’s condition?
CorrectIncorrect -
Question 15 of 40
15. Question
An 18-year-old woman is seen in the clinic for irregular menses. The patient reports menarche at age 15; she had a few irregular periods after menarche but has not had a menstrual cycle in the past 2 years. She has no abdominal pain, spotting, or vaginal discharge. The patient wears glasses for nearsightedness and has had no recent vision changes. She also has a history of recurrent otitis media requiring tympanostomy tubes. The patient takes no medications. Weight is 45 kg (99.2 lb). Height is 140 cm (4ft 7 in). BMI is 23 kg/m2. Temperature is 36.6 C (97.9 F), blood pressure is 110/70 mm Hg, pulse is 60/min, and respirations are 13/min. Cardiopulmonary examination is normal. External genitalia are normal with Tanner stage 3 breast and pubic hair development. Multiple small, hyperpigmented nevi are scattered on the face and extremities. Urine pregnancy test is negative. Which of the following laboratory results are most likely in this patient?
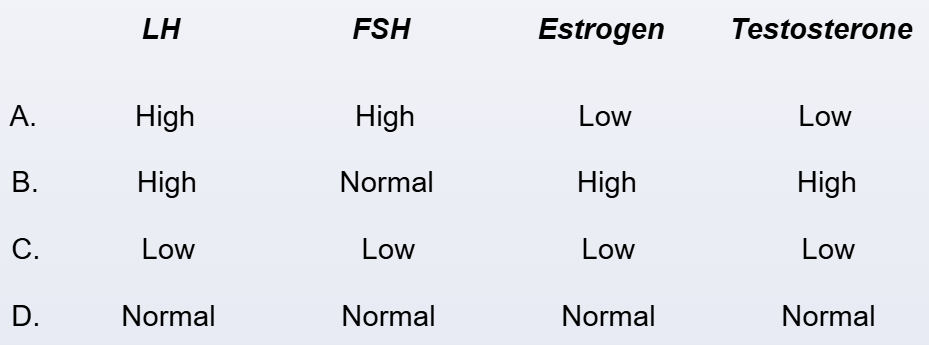 CorrectIncorrect
CorrectIncorrect -
Question 16 of 40
16. Question
A 52-year-old woman comes to the office for evaluation of menopause. The patient thought she was going through menopause after 8 months of amenorrhea and nightly hot flashes. However, in the past 4 months she has resumed heavy, irregular menstrual cycles and she is no longer having hot flashes. On review of systems, the patient reports some decreased energy, along with weight gain and abdominal bloating despite eating less. She has hypertension and type 2 diabetes mellitus that are well controlled on medication. The patient has had no prior surgeries. She had 2 vaginal deliveries in her 20s, followed by a tubal ligation. Vital signs are normal. BMI is 28 kg/m2. On physical examination, the patient has a distended abdomen with mild tenderness to palpation in the lower quadrants. The pelvic examination reveals rugated vaginal epithelium with no discharge. Pelvic ultrasound reveals a 5-cm complex adnexal mass with no free fluid in the pelvis. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
A 54-year-old postmenopausal woman comes to the office because she would like to undergo a hysterectomy for symptomatic uterine fibroids. Eight months ago, the patient was evaluated for pelvic fullness; pelvic examination showed an irregularly enlarged uterus palpated 4 cm below the umbilicus. Pelvic ultrasound at that time confirmed multiple large uterine fibroids and normal ovaries. The patient elected conservative management but now reports constant pelvic pressure with urinary frequency and constipation. Menopause was at age 51, but she has had no postmenopausal bleeding. She has had no prior surgeries. The patient has never had an abnormal Pap test, and her most recent cervical cancer screening was 2 years ago. Vital signs are normal. BMI is 27 kg/m2. Pelvic examination shows a palpable uterine fundus with an irregular contour 4 cm below the umbilicus, which is consistent with the previous examination. The right adnexum is approximately 5 cm in size, which was not present before. The left adnexum is normal. The cervix is smooth and nontender. The patient would like surgery for resolution of her symptoms. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 18 of 40
18. Question
A 30-year-old nulliparous woman comes to the office due to amenorrhea. Shortly after menarche at age 15, the patient began taking combined estrogen/progestin oral contraceptives for irregular menstrual cycles. While she was using contraception, her menstrual periods occurred every 28 days and consisted of 3-4 days of light bleeding. The patient stopped using contraception a year ago to conceive, and since then has not had a menstrual period. She has hot flashes several times a day and often awakens at night with profuse sweating. The patient has no chronic medical conditions and has had no previous surgeries. She takes a daily multivitamin and acetaminophen occasionally for headaches. Her sister (age 40) has 2 children and has regular monthly menses. Blood pressure is 110/70 mm Hg, weight is 65 kg (143.3 lb), and height is 152.5 cm (5 ft). Laboratory results are as follows:
FSH
42 mU/mL
Estradiol, serum
15 pg/mL (normal premenopausal: 30-400)
Prolactin
6 ng/mL
TSH
1.3 µU/m
Urine pregnancy test
negative
Pelvic ultrasound shows a normal uterus with a thin endometrial stripe and small ovaries bilaterally. Which of the following is the best next step in diagnosis of this patient’s condition?
CorrectIncorrect -
Question 19 of 40
19. Question
A 33-year-old woman comes to the emergency department due to abdominal pain. The pain began 2 weeks ago and was initially mild, episodic, confined to the right lower quadrant, and resolved spontaneously without intervention. For the past 6 hours, the pain has been severe, constant, unrelieved by ibuprofen or acetaminophen, and radiating to the right flank. The pain is now accompanied by constant nausea and multiple episodes of emesis. The patient has had no diarrhea or recent travel. She has no chronic medical conditions but did have an appendectomy. The patient was treated for Chlamydia trachomatis cervicitis as a teenager. She is not currently sexually active. She does not use tobacco, alcohol, or illicit drugs. Temperature is 38 C (100.4 F), blood pressure is 130/80 mm Hg, pulse is 83/min, and respirations are 16/min. Abdominal examination shows tenderness and guarding in the right lower quadrant but no suprapubic or costovertebral angle tenderness. Pelvic examination shows a small, nontender, retroverted uterus and a tender right adnexal mass. Speculum examination is normal. Urine pregnancy test is negative. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 65-year-old postmenopausal woman comes to the office for evaluation of dyspareunia. The patient recently became sexually active after 7 years of abstinence after the death of her husband. She has a new partner and has pain with intercourse but has had no postcoital or postmenopausal bleeding. The patient was last seen in the office 10 years ago when she underwent treatment for biopsy-proven lichen sclerosus. Her symptoms improved after she was treated with high-dose topical corticosteroids. Pap test at that time was normal. The patient has type 2 diabetes mellitus and hypertension, for which she takes metformin and an ACE inhibitor. She had 3 vaginal deliveries when she was in her 20s. The patient stopped smoking 5 years ago and does not use alcohol or illicit drugs. Family history is noncontributory. Blood pressure is 128/82 mm Hg and pulse is 72/min. BMI is 28 kg/m2. Pelvic examination shows a raised, pigmented lesion over the clitoral hood and extending to the right labium majus. Multiple areas of excoriations are noted throughout the vulva. There is no palpable inguinal lymphadenopathy. Speculum examination reveals an atrophic vagina and a cervix with no visible lesions. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 21 of 40
21. Question
A 22-year-old woman comes to the office with right lower quadrant pain for the past 3 weeks. The pain is exacerbated with bowel movements, but there is no associated nausea, vomiting, diarrhea, constipation, or melena. She has no chronic medical conditions and has never had surgery. Family history is noncontributory. The patient has regular menstrual periods every 28-30 days. She is sexually active and uses condoms for contraception. She does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 110/70 mm Hg, and pulse is 80/min. BMI is 24 kg/m2. Physical examination shows a well-appearing woman in no apparent distress. The abdomen is soft with normal bowel sounds. There is tenderness to deep palpation in the right lower quadrant without rebound or guarding. The uterus is small, nontender, and anteverted; there is no cervical discharge or cervical motion tenderness. The right adnexa is enlarged and tender. There is nodularity and tenderness on rectovaginal examination. This patient is at increased risk for which of the following conditions?
CorrectIncorrect -
Question 22 of 40
22. Question
A 28-year-old woman comes to the office with 2 days of vaginal spotting. The patient has no fever, chills, nausea, vomiting, or cramping. Her last menstrual period was 6 weeks ago, and she had a positive home pregnancy test yesterday. The patient has no chronic medical conditions or previous surgeries. She is sexually active with a new male partner and uses condoms for contraception. The patient previously used a copper intrauterine device for contraception but had it removed due to increased pain and heavy menstrual bleeding. Recent nucleic acid amplification testing for chlamydia and gonorrhea was negative. The patient does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 108/68 mm Hg, and pulse is 81/min. The abdomen is soft and nontender with no guarding or rebound. Pelvic examination reveals dark red blood in the posterior vaginal fornix and a closed cervix. On bimanual examination, there is mild left adnexal tenderness with fullness but no cervical motion tenderness. The uterus is small and nontender. Quantitative β-hCG is 3,700 IU/L. Transvaginal ultrasound reveals a 4.6-cm left adnexal complex mass and a thickened endometrium. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 52-year-old woman, gravida 3 para 3, comes to the office with irregular vaginal bleeding for the past 8 months. She has had vaginal bleeding for the last 10 days, with passage of large clots on the first 2 days. Today, she has minimal spotting. Previously, menses were regular and occurred every 30 days with 4 days of bleeding. She also has frequent hot flashes, difficulty sleeping, and occasional headaches. The patient was diagnosed with type 2 diabetes mellitus 16 years ago and has good blood glucose control with insulin therapy. She had a tubal ligation after her last pregnancy. The patient’s last Pap test was 2 years ago, and there is no history of abnormal results. She has not been sexually active for several years. Family history is significant for breast cancer in her maternal aunt at age 72 but is otherwise noncontributory. She does not use tobacco and has no drug allergies. Blood pressure is 130/80 mm Hg, pulse is 78/min, and respirations are 16/min. BMI is 35 kg/m2. Pelvic examination shows a small amount of dark red blood in the vaginal vault and a multiparous cervix without any visible lesions. On bimanual examination, there is a small, mobile, anteverted uterus with no cervical motion tenderness. There are no adnexal masses. Hemoglobin is 12 g/dL. The patient asks for an explanation of her symptoms and what should be done for evaluation. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 24 of 40
24. Question
A 52-year-old woman comes to the office for a routine health maintenance examination. The patient is due for breast and cervical cancer screening. Her last menstrual period was 3 weeks ago, but over the last year she has had longer intervals between menses. Previously, the patient had monthly cycles with 4 days of moderate bleeding. All her friends are now in menopause, and she is wondering if these menstrual changes suggest a similar transition for her. The patient is feeling well and has had no recent weight loss, appetite changes, bloating, or hot flashes. Vital signs are normal. BMI is 23 kg/m2. Cardiopulmonary examination is normal. The abdomen is soft and nontender. On speculum examination, the cervix appears stenotic but is without lesions. Bimanual examination shows a small mobile uterus. The ovaries are not palpated. Which of the following is the most appropriate management of this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 25-year-old woman comes to the office due to amenorrhea. The patient has had no changes in vision or cold or heat intolerance and no abnormal vaginal discharge. Her last menstrual period was 2 months ago. Menarche was at age 12; the patient’s menstrual cycles are normally 28 days long with 3-4 days of light bleeding. Medical history is significant for type 1 diabetes mellitus and epilepsy. Three months ago, the patient was hospitalized for generalized tonic-clonic seizures, and phenytoin was added to her medication regimen. She has had no seizure activity since. Blood glucose levels are well controlled with insulin. The patient is sexually active and uses combined estrogen/progestin oral contraceptive pills. Four years ago, she underwent dilation and curettage for the termination of a pregnancy complicated by hemorrhage, requiring a blood transfusion. The patient does not use tobacco, alcohol, or illicit drugs. Temperature is 36.7 C (98.1 F), blood pressure is 110/60 mm Hg, pulse is 76/min, and respirations are 12/min. BMI is 22 kg/m2. There is minimal facial acne. Visual fields are intact. The thyroid is not enlarged with no palpable masses. The breasts are mildly tender to palpation; there are no masses or nipple discharge. The abdomen is soft and nontender, with no palpable masses. Pelvic examination shows a mobile uterus with no adnexal masses. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 26 of 40
26. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 63-year-old woman, gravida 3 para 3, comes to the office for urinary incontinence. The patient has been experiencing involuntary leakage of urine that occurs after a strong sensation “that I really have to go.” After the sensation occurs, “I can never get to the bathroom in time.” The patient reports that her symptoms started over 2 years ago. The leakage was initially occasional but now occurs 2 or 3 times a day and soaks an entire pad. The patient’s symptoms occur randomly and she now avoids leaving the house. She has hypertension controlled on an ACE inhibitor. She has had no surgery. The patient’s deliveries were all vaginal; her Pap tests have been normal. She drinks 8 ounces of water 3 or 4 times a day but limits water intake in the evening; on weekends she drinks a cup of caffeinated coffee with breakfast. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 130/80 mm Hg and pulse is 72/min. BMI is 23 kg/m2. Speculum examination shows a pale vagina without rugae. Bimanual examination reveals a small, mobile uterus and no adnexal masses. No leakage of urine occurs when the patient coughs with a full bladder. After voiding, the patient is catheterized and 30 mL of urine are drained from the bladder. Urinalysis is within normal limits.
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
Item 2 of 2
The patient returns to the office 10 weeks later for follow-up. She reports no response to the initial therapy. Repeat urinalysis is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 48-year-old woman comes to the office because she thinks she is starting to go through menopause. Over the last year, the patient has developed intermittent hot flushes, and her menstrual periods are becoming more unpredictable. She has 1 or 2 hot flushes a day and occasionally wakes from sleep due to sweating. During this time, menstrual periods started occurring every 5-6 weeks, but now, the patient has bleeding 1-2 weeks after a previous cycle. Medical history is significant for hypertension and hyperlipidemia. Her only surgeries are 2 cesarean deliveries and a bilateral tubal ligation with her last delivery. Family history is significant for breast cancer diagnosed in her mother and maternal aunt in their 50s. Temperature is 36.7 C (98.1 F), blood pressure is 130/80 mm Hg, and pulse is 78/min. BMI is 31 kg/m2. On pelvic examination, the uterus is anteverted and anteflexed. The ovaries are nonpalpable. The cervix has no bleeding from the os and no lesions. The patient states that the hot flushes are tolerable, but she would like a progestin-releasing intrauterine device (IUD) to reduce her menstrual bleeding. Which of the following is the most appropriate recommendation for this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
A 46-year-old woman, gravida 3 para 3, comes to the office due to left nipple discharge. She reports that the discharge began 1 month ago, is present almost daily, and stains her undergarments. It is typically yellow, thin, and sticky but occasionally leaves rust-colored stains on her bra. The patient has no chronic medical conditions and takes no daily medications. Menses are regular, and her last menstrual period was 3 weeks ago. The patient’s youngest child was born 6 years ago by cesarean delivery; bilateral tubal ligation was performed with the delivery. All 3 of her children were breastfed. There is no family history of breast cancer in her first-degree relatives. Temperature is 37.2 C (99 F), blood pressure is 130/86 mm Hg, and pulse is 70/min. BMI is 33 kg/m2. Serous discharge is expressed from the left nipple. No palpable masses, skin discoloration or retraction, or axillary lymphadenopathy is present. The right breast has no expressed nipple discharge, masses, or lymphadenopathy. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 51-year-old woman comes to the office due to bilateral nipple discharge that she first noticed 3 weeks ago. The discharge occurs only with manipulation of the nipples and is not bloody or rust colored. The patient has had no breast pain, masses, or skin changes. A mammogram 6 months ago was normal. Since menopause at age 50, she has taken soy and vitamin E for frequent hot flashes. In addition, she has hypertension that is well controlled by a single medication. The patient drinks a glass of wine occasionally and does not use tobacco or recreational drugs. Her grandmother died from metastatic breast cancer at age 85. Blood pressure is 140/80 mm Hg and pulse is 80/min. BMI is 27 kg/m2. Bilateral breast examination reveals no masses, tenderness, or skin changes. A clear yellow discharge is expressed from both nipples. There is no axillary or supraclavicular lymphadenopathy. Laboratory results are as follows:
Endocrine
β-hCG
<3 IU/L
Prolactin, serum
6 ng/mL
TSH
2.4 µU/mL
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 17-year-old girl, gravida 0 para 0, comes to the office for routine examination and an oral contraception prescription. Her menses occur every 28 days and her last menstrual period was 3 weeks ago. She is feeling well and is preparing to leave for college in 5 months. The patient has no chronic medical conditions or previous surgeries. She has no history of migraine headaches or thromboembolism. The patient is up to date on all vaccinations. Her maternal grandmother has hepatitis B; family history is otherwise noncontributory. The patient currently takes no medications and does not use tobacco, alcohol, or illicit drugs. She has no known drug allergies. She has been sexually active with one partner for the past 2 years and uses condoms for contraception. Temperature is 37.2 C (99 F), blood pressure is 110/70 mm Hg, and pulse is 72/min. Weight is 60 kg (132.3 lb) and height is 162.5 cm (5 ft 4 in). Cardiopulmonary examination is normal. The abdomen is soft and nontender with no hepatosplenomegaly. On pelvic examination, no vulvar or cervical lesions and no cervical discharge are present. On bimanual examination, the uterus is small and without cervical motion tenderness. Bilateral adnexa are small, mobile, and nontender. In addition to an oral contraception prescription, which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 29-year-old woman comes to the emergency department with lower abdominal pain that woke her up 7 hours ago and has not been relieved by acetaminophen. Movement and deep inspiration make the pain worse. The patient has no chronic medical conditions. She underwent a laparoscopic appendectomy at age 14. She is sexually active and uses condoms for contraception. The patient’s last menstrual period was 5 weeks ago, but she has had intermittent vaginal spotting the last few days. She smokes a pack of cigarettes daily but does not use alcohol or illicit drugs. The patient has no known drug allergies. Temperature is 37.2 C (99 F), blood pressure is 84/60 mm Hg, pulse is 124/min, and respirations are 18/min. Cardiac examination shows tachycardia with a normal rhythm; there are no murmurs. The lungs are clear to auscultation bilaterally. Bowel sounds are decreased, and the abdomen is diffusely tender and rigid, with rebound and guarding. Pelvic examination shows cervical motion tenderness and diffuse uterine and adnexal tenderness. Laboratory results are as follows:
Hematocrit
30%
Leukocytes
11,000/mm3
β-hCG
1,100 IU/L (normal range: variable based on gestational age)
Blood type
B, Rh positive
In addition to appropriate supportive care, which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 33 of 40
33. Question
A 33-year-old woman comes to the office to discuss contraception. The patient and her boyfriend have been using condoms and the morning-after pill occasionally to prevent pregnancy. She most recently used emergency contraception a week ago. The patient used combined oral contraceptive pills in her early 20s and would like to restart them. Her medical conditions include occasional headaches; she describes them as throbbing pain on the right side of her face preceded by “flickering zigzags” in her peripheral vision. During the headache, she has light sensitivity and facial numbness. The patient has had no previous surgeries. Her menses are regular; her last menstrual period was 3 weeks ago. The patient’s mother has epithelial ovarian cancer diagnosed at age 59 and is undergoing chemotherapy. Her maternal grandmother also had ovarian cancer and died at age 56. The patient smokes 1-2 cigarettes daily but does not use alcohol or recreational drugs. She has no known medication allergies. Blood pressure is 130/80 mm Hg and pulse is 76/min. BMI is 33 kg/m2. Physical examination is normal. Which of the following is a contraindication to this patient’s use of a combined hormonal contraception method?
CorrectIncorrect -
Question 34 of 40
34. Question
A 28-year-old woman with polycystic ovary syndrome (PCOS) comes to the office for worsening acne and facial hair. The patient was diagnosed with PCOS 2 years ago after presenting with irregular menses, hirsutism, and multiple peripheral ovarian cysts on pelvic ultrasonography. Eight months ago, she stopped her oral contraceptives and started a weight-loss program to try for pregnancy. Despite a 6.8-kg (15-lb) weight loss, the patient has not conceived and has experienced an increase in the severity of both her acne and hair on her chin and upper lip. Her only medication is a prenatal vitamin. Vital signs are normal. BMI is 36 kg/m2. On physical examination, multiple coarse hairs are seen on the chin and upper lip, and bitemporal hair thinning is present. There is nodulocystic acne on the cheeks, back, and upper chest. Pelvic examination shows minimal vaginal rugation, and a normal-appearing cervix. Bimanual examination is limited secondary to body habitus, but a small, mobile uterus with left lateral fullness is palpated. Urine pregnancy test is negative. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 35 of 40
35. Question
A 23-year-old woman comes to the office with worsening fever, chills, and lower abdominal pain for 3 days. The patient has been taking nonsteroidal anti-inflammatories for pain relief. She also has increasing malodorous vaginal discharge. The patient has a history of 2 episodes of pelvic inflammatory disease that required hospitalization and intravenous antibiotic treatment. She has smoked a pack of cigarettes daily for 7 years and consumes 1 or 2 beers daily. The patient has had 6 sexual partners over the last 6 months. She had an intrauterine device (IUD) placed a year ago and inconsistently uses barrier contraception. The patient has no known drug allergies. Temperature is 38.3 C (100.9 F), blood pressure is 110/70 mm Hg, pulse is 100/min, and respirations are 20/min. Weight is 60 kg (132.3 lb) and height is 157.5 cm (5 ft 2 in). Examination shows a soft, nondistended abdomen with mild rigidity and rebound tenderness in the lower abdomen; bowel sounds are present. There is no hepatosplenomegaly. No lesions are present on the vulva or vagina. Pelvic examination reveals cervical motion and bilateral adnexal tenderness as well as purulent discharge from the cervical os. The IUD strings are visible at the external cervical os. Laboratory results are as follows:
Hemoglobin
12.4 g/dL
Platelets
200,000/mm3
Leukocytes
14,000/mm3
Urinalysis shows 50+/hpf of WBCs. Urine pregnancy test is negative. Nucleic acid amplification testing is positive for Neisseria gonorrhoeae. Pelvic ultrasound reveals a dilated fallopian tube filled with debris. Which of the following is the strongest risk factor for this patient’s condition?
CorrectIncorrect -
Question 36 of 40
36. Question
A 74-year-old woman, gravida 5 para 5, comes to the office due to vaginal spotting and discharge for several months. The patient reports a mass coming out of her vagina. She is now having difficulty defecating; increased straining causes the mass to increase in size. The patient has hypertension, type 2 diabetes mellitus, and New York Heart Association (NYHA) class III heart failure. Her last hemoglobin A1c was 11.8. She had 5 spontaneous vaginal deliveries and has no history of abnormal Pap tests. The patient has a 40-pack-year history. Blood pressure is 150/90 mm Hg, pulse is 84/min, and respirations are 16/min. Oxygen saturation is 89% on room air. BMI is 41 kg/m2. Cardiopulmonary examination reveals decreased breath sounds bilaterally. The abdomen is nontender and has no palpable masses. Pelvic examination reveals the cervix at the level of the vaginal introitus. The vaginal mucosa is thin with small, minor areas of excoriation and erosion. Ultrasonography reveals a thin endometrial stripe. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
A 17-year-old girl comes to the office for an annual physical examination. The patient learned about the association between sexual activity and cervical cancer and wonders when she should undergo Pap testing. She became sexually active 2 years ago and has had 4 sexual partners. The patient received the human papillomavirus vaccination series at age 11. She uses condoms and depot medroxyprogesterone acetate for contraception and has gained 5 kg (11 lb) during the 2 years she has taken the medication. The patient has been amenorrheic for over a year. She had a negative screen for sexually transmitted infections a year ago. The patient has seasonal allergies but no other chronic medical conditions. She does not use tobacco, alcohol, or illicit drugs. Vital signs and general physical examination are within normal limits. A urine gonorrhea and chlamydia nucleic acid amplification test is collected. Urine pregnancy test is negative. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 38 of 40
38. Question
A 36-year-old woman comes to the office for evaluation of vulvar lesions. She noticed the vulvar bumps 6 months ago, and they have slowly increased in size and number; she has had no associated bleeding or pruritus. The patient was diagnosed with HIV last year and was prescribed antiretroviral therapy, but she has been taking the medication only intermittently. Her most recent CD4 count was 320/mm3. She is sexually active with a male partner who also has HIV. The patient has no pain with intercourse or postcoital bleeding. On pelvic examination, there are multiple raised nodules throughout the posterior vulva that are nontender and nonfriable. There is scant physiologic vaginal discharge and no visible cervical lesions. The uterus is mobile and there are no adnexal masses. Which of the following is the most appropriate next step in management of this patient’s lesions?
CorrectIncorrect -
Question 39 of 40
39. Question
A 20-year-old woman comes to the office for a routine check-up. The patient has regular monthly menses, and no chronic medical conditions or prior surgeries. She smokes a half pack of cigarettes daily and does not use alcohol or recreational drugs. The patient is sexually active and has had 3 male partners in the past year. She uses barrier contraception methods intermittently, and her only medication is a combination oral contraceptive pill. BMI is 34 kg/m2. Pelvic examination shows several 3- to 4-mm projections on the posterior wall of the vagina and perianal area. The projections bleed easily when touched and turn white on acetic acid application. The remainder of the physical examination is normal. The examination findings are discussed with the patient, and she states that she has had some vaginal pruritus and bleeding for the past few months, which have been embarrassing to her. Which of the following is the most appropriate management option for this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 20-year-old woman comes to the office due to increasing vaginal discharge and vulvar pruritus. The patient has had vaginal discharge for the past 4 days. She is sexually active with multiple partners and uses oral contraceptive pills. Vital signs are normal. Pelvic examination is performed, and wet mount microscopy of a vaginal swab is shown in the exhibit. Which of the following is the most appropriate pharmacotherapy for this patient?
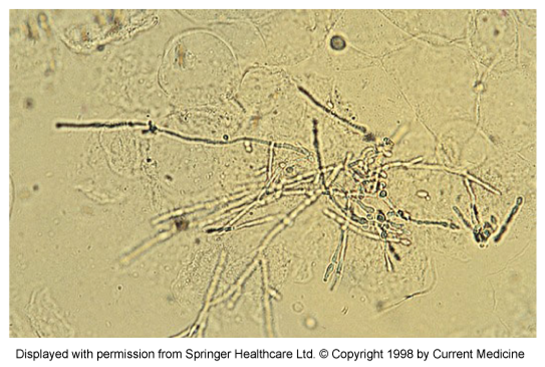 CorrectIncorrect
CorrectIncorrect
