Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 79-year-old woman is hospitalized after a fall that resulted in a left femoral neck fracture. She tripped over her dog while cleaning her home, hit her head on a bookshelf, and landed on her left side. Prior to this she had been in her usual state of health; her other medical issues include obesity, type 2 diabetes mellitus, hypertension, chronic kidney disease, and hypothyroidism. The patient lives at home by herself. She has smoked a pack of cigarettes daily for 38 years. She drinks alcohol every weekend. Results of the patient’s initial workup in the emergency department demonstrated the left femoral neck fracture, creatinine of 2.0 mg/dL, and a negative noncontrast head CT. She was admitted to the hospital and the following day underwent surgical repair. The procedure was uncomplicated. However, on postoperative day 3 the patient is noted to be uncomfortable and mildly agitated. She is unable to coherently explain her symptoms. Current medications include prophylactic subcutaneous heparin, insulin glargine, omeprazole, hydrocodone, and levothyroxine. Temperature is 37.7 C (99.9 F), blood pressure is 104/68 mm Hg, pulse is 114/min, and respirations are 28/min. Pulse oximetry is 86% on room air. Examination shows equal round and reactive pupils. Lung examination demonstrates decreased breath sounds at the bilateral bases. Heart rhythm is regular with normal S1 and S2. The surgical incision shows no surrounding erythema or purulent drainage. The patient follows commands and moves all extremities except the left leg. Laboratory results are as follows:
Complete blood count
Leukocytes
11,000/mm3
Hemoglobin
10.6 g/dL
Platelets
260,000/mm3
Serum chemistry
Sodium
134 mEq/L
Bicarbonate
24 mEq/L
Creatinine
2.2 mg/dL
Glucose
160 mg/dL
Troponin I is undetectable. Chest x-ray shows slight bibasilar atelectasis without focal consolidation, pleural effusion, or pulmonary edema. ECG shows sinus tachycardia but is otherwise unremarkable.
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 2
Ventilation-perfusion scan shows high probability for pulmonary embolism. The patient is started on intravenous heparin. The next day, the nurse reports that the patient has a fever. The patient still has some chest pain but her shortness of breath and mental status are improved. There is no cough, abdominal pain, nausea, vomiting, diarrhea, dysuria, urinary frequency, or headache. Temperature is 38.3 C (101 F), blood pressure is 121/73 mm Hg, pulse is 102/min, and respirations are 22/min. Oxygen saturation is 92% on 2 L of oxygen by nasal cannula. She does not appear ill. The lungs are clear to auscultation. The abdomen is soft and nontender. Neurologic examination is nonfocal. The operative site is healing well without erythema or purulence. The patient’s 2 peripheral IV lines have no evidence of infection. Indwelling urinary catheter is draining clear yellow urine. Laboratory results are as follows:
Leukocytes
10,800/mm3
Neutrophils
72%
Lymphocytes
21%
Monocytes
3%
Eosinophils
3%
Basophils
1%
Hemoglobin
10.6 g/dL
Platelets
280,000/mm3
Chest x-ray shows no new abnormalities. Urinalysis is normal. Blood cultures are sent. Which of the following would be the most appropriate next step for this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
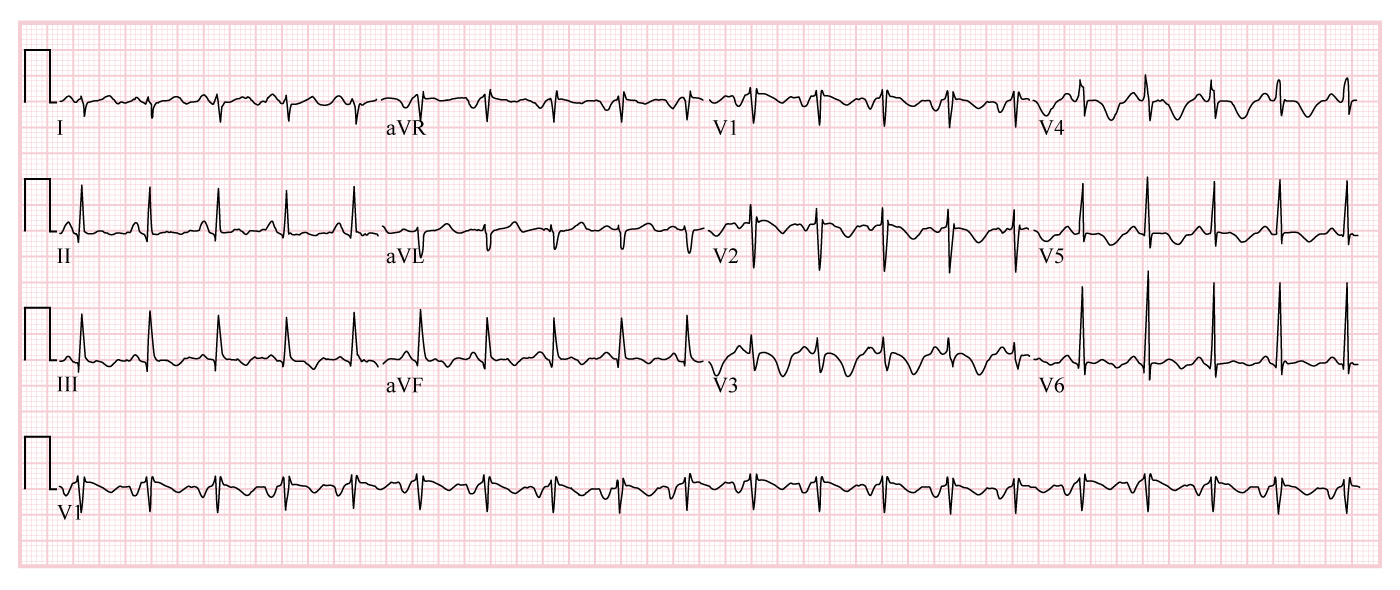
A 63-year-old woman is brought to the emergency department from a rehabilitation facility due to shortness of breath and global weakness. After eating lunch today, her breath suddenly felt “heavy.” She became lightheaded and too weak to stand, rendering her unable to engage with physical therapy. The patient had been at the facility for 5 days following a long intensive care stay for pneumonia and septic shock. Medical history includes hypertension and mild aortic stenosis seen on an echocardiogram 2 years ago. The patient has a 30-pack-year history. Temperature is 36.2 C (97.2 F), blood pressure is 73/58 mm Hg, pulse is 122/min and regular, and respirations are 36/min. Pulse oximetry reading is 75% on room air and improves to 93% with supplemental oxygen by non-rebreather mask. She appears restless but follows commands. The lungs are clear on auscultation. Cardiac examination demonstrates a regular tachycardic rhythm with an early-peaking grade 2/6 systolic ejection murmur. The abdomen is soft. The extremities are cool. Chest x-ray is clear. ECG is shown below.
After administration of a 500-mL bolus of crystalloid resuscitation fluid, blood pressure is 75/57 mm Hg.
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
Item 2 of 2
Emergency bedside echocardiography and lower extremity venous ultrasonography are performed as part of a rapid ultrasound assessment of shock and hypotension. A noncompressible lumen-filling defect is seen in the left external iliac vein. Cardiac telemetry continues to show sinus tachycardia. Which of the following echocardiographic findings is most likely to be present?
CorrectIncorrect -
Question 5 of 40
5. Question
A 43-year-old man comes to the office with his wife for evaluation of his snoring. His wife reports that he snores loudly most nights and keeps her awake, but she has not observed him choke, gasp, or stop breathing while asleep. The patient is unaware of his snoring and reports no morning headaches, memory loss, or poor concentration. He occasionally falls asleep after lunch while seated at his desk. He reports no fatigue, weight gain, or constipation. His medical problems include seasonal allergies and hypothyroidism. The patient’s medications include intranasal fluticasone and levothyroxine. He drinks 12-24 ounces of beer daily, usually 1-2 hours before going to bed. He does not use tobacco or illicit drugs. Both his parents have hypertension. Temperature is 36.8 C (98.2 F), blood pressure is 125/75 mm Hg, pulse is 65/min, and respirations are 16/min. BMI is 26 kg/m2 and neck circumference is 39.4 cm (15.5 in). Physical examination reveals an alert, oriented, and cooperative man in no distress. Oropharyngeal examination is normal. No nasal polyps or septal deviation is seen, and the nares are normal in appearance. Cardiac examination reveals normal first and second heart sounds and no jugular venous distension. The lung fields are clear bilaterally. No edema or rashes are present. Laboratory results are as follows:
Leukocytes
4,100/mm3
Hemoglobin
14.4 g/dL
Platelets
320,000/mm3
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
A 55-year-old man comes to the emergency department after coughing up blood earlier this morning. The patient estimates that he coughed up 100 mL of blood at home and another 50 mL in the emergency department. He reports 4 hospital admissions for pneumonia in the past 18 months, but this is the first episode of hemoptysis. He has a chronic cough with yellow-green sputum production that is sometimes foul-smelling. The patient gets winded after climbing 2 flights of stairs or walking uphill. He is an ex-smoker with a 10-pack-year history. Physical examination is notable for crackles at the right lung base and scattered bilateral wheezes. There is no jugular venous distension or lower-extremity edema. What is the most likely mechanism of hemoptysis in this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
A 67-year-old man comes to the emergency department due to increasing shortness of breath over the past 4 days, accompanied by cough productive of greenish sputum. The patient has severe chronic obstructive pulmonary disease treated with tiotropium and budesonide/formoterol. Blood pressure is 152/90 mm Hg, pulse is 108/min, respirations are 22/min, and pulse oximetry shows 84% on room air. He is in mild respiratory distress, speaking in clipped sentences, with some accessory muscle usage. Chest auscultation reveals prolonged expiration with decreased breath sounds bilaterally. Pulse oximetry improves to 94% after he is placed on supplemental oxygen at 5 L/min. Which of the following mechanisms best explains this patient’s improved saturation following oxygen supplementation?
CorrectIncorrect -
Question 8 of 40
8. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 59-year-old man comes to the office due to cough and mild dyspnea. His symptoms began 10 days ago with nasal congestion and a sore throat, which improved spontaneously after a few days. However, the cough, productive of white sputum, has persisted. He has also had an episode of blood-streaked sputum. The patient has a history of hypertension and stable coronary artery disease. He is a current smoker with a 20-pack-year history. The patient is a car salesman and has not traveled recently. Temperature is 36.7 C (98.1 F), blood pressure is 110/72 mm Hg, and respirations are 18/min. Lung examination shows scattered wheezes bilaterally. Chest x-ray demonstrates no parenchymal infiltrate or consolidation, but a 2-cm peripherally located nodule is present in the left lower lobe. No prior chest imaging is available.
Item 1 of 2
Which of the following is the most appropriate initial step in management of this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
Item 2 of 2
CT scan of the chest confirms a 2.2-cm, peripherally located nodule in the left lower lobe surrounded by lung parenchyma. The nodule has spiculated borders and eccentric calcification on the periphery, and no lymphadenopathy is present. CT scan of the abdomen reveals no abnormalities of the liver or adrenal glands. Which of the following is the best next step in management of this patient’s lung lesion?
CorrectIncorrect -
Question 10 of 40
10. Question
A 67-year-old man comes to the emergency department due to 3 days of fever and cough productive of yellowish sputum. He has had no hemoptysis, weight loss, night sweats, or anorexia. He has not traveled recently and has not had exposure to anyone with similar symptoms. The patient was discharged from the hospital 3 weeks ago after an episode of community-acquired pneumonia involving the left lower lobe. He is a chronic smoker with a 45-pack-year smoking history. He drinks alcohol occasionally. Temperature is 38.1 C (100.6 F), blood pressure is 112/52 mm Hg, pulse is 98/min, and respirations are 22/min. Oxygen saturation is 90% on room air. Physical examination reveals decreased breath sounds and crackles over the left lower lobe. Chest x-ray is consistent with consolidation of the left lower lung zone. What is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 28-year-old woman comes to the office due to cough for the past 6 months. The patient reports intermittent spells of nonproductive cough. She has a sensation of chest tightness and often has “noisy breathing” during these episodes. The patient has noted the symptoms mostly occur at nighttime but also occasionally during the daytime. She reports no fever, chills, or chest pain. The patient has no prior medical conditions and takes no medications. She does not use tobacco, alcohol, or recreational drugs. The patient works as an attorney, has lived in the same house for several years, and has no pets. There is no significant family history. Vital signs are within normal limits. Lung examination reveals normal air movement without crackles, wheezing, or other adventitious sounds. Cardiovascular examination reveals normal heart sounds, no murmurs, and normal jugulovenous pressure. There is no extremity edema or rash. Spirometry is performed in the office and shows a normal FEV1, FVC, and FEV1/FVC ratio. Which of the following additional pulmonary function evaluations is most strongly indicated at this time?
CorrectIncorrect -
Question 12 of 40
12. Question
A 74-year-old man with a history of hypertension comes to the clinic asking advice about his recent memory problems. He is accompanied by his wife. The patient says, “I have always been very sharp but over the last year I have had difficulty remembering things. I missed a number of appointments and sometimes I feel embarrassed because I forget names of the people I meet.” His wife says he has been moody and irritable and that he complains of headaches; “He doesn’t sleep well at nights and we rarely have sex now. I don’t know if it’s old age or what.” The patient reports no nausea, vomiting, falls, weakness, weight loss, fevers, chills, vision changes, or incontinence. Other issues include obesity, diet-controlled type 2 diabetes mellitus, and coronary artery disease. Current medications include lisinopril, atorvastatin, aspirin, and carvedilol. He does not use alcohol, tobacco, or recreational drugs. Family history is unremarkable. Temperature is 36.7 C (98 F), blood pressure is 155/95 mm Hg, pulse is 62/min, and respirations are 14/min. BMI is 34 kg/m2 and neck circumference is 45.7 cm (18 in). Examination shows normal jugular venous pressure and no lymphadenopathy. Lung fields are clear, and S1 and S2 are normal. The abdomen is soft and nontender. Examination shows no edema. Mental status examination shows poor concentration and 3-object recall, while other aspects are normal. Cranial nerves are within normal limits. Muscle strength is 5/5 in both upper and lower extremities, and upper and lower limb deep tendon reflexes are 2+. Gait is normal. The patient’s complete blood count and metabolic panel are normal. Other laboratory results are as follows:
Vitamin B12, serum
550 pg/mL (normal: 200-800 pg/mL)
TSH
3.4 µU/mL
Which of the following is the best response to this patient’s concerns?
CorrectIncorrect -
Question 13 of 40
13. Question
A 28-year-old man comes to the clinic due to a nonproductive cough and chest tightness for the past 3 months. The cough is most prominent in the early morning when he jogs but also occurs at night. He has had no recent nasal symptoms, fever, malaise, or weight loss. He stopped smoking 3 years ago but had smoked half a pack a day for 5 years. He lives with his wife and 2 children and exercises regularly. He works as a technician for an air conditioning-repair company in Philadelphia. Temperature is 36.7 C (98.1 F), blood pressure is 130/80 mm Hg, pulse is 84/min, and respirations are 14/min. Oxygen saturation is 97% on room air. BMI is 26 kg/m2. There is no jugular venous distension and no pharyngeal erythema or exudates. No wheezes or rhonchi are heard in either lung. During the examination, coughing was induced when the patient was asked to do a forced expiration. Cardiac examination reveals normal heart sounds. The abdomen is soft and nontender; no masses are felt. There is no peripheral edema. What is the cause of this patient’s persistent cough?
CorrectIncorrect -
Question 14 of 40
14. Question
A 76-year-old man comes to the emergency department due to shortness of breath, fatigue, cough, and fever over the last 2 days. The patient’s medical problems include chronic obstructive pulmonary disease, osteoarthritis, and hypertension. Temperature is 38.6 C (101.5 F), blood pressure is 110/60 mm Hg, pulse is 110/min, and respirations are 20/min. Oxygen saturation is 87% on ambient air. Chest x-ray reveals left lower lobe and right middle lobe consolidation. The patient is admitted to the hospital for community-acquired pneumonia and treated with azithromycin and ceftriaxone. His dyspnea is relieved by bronchodilator therapy. The patient’s condition improves after 2 days of treatment. Temperature is now 37.8 C (100.0 F), blood pressure is 125/70 mm Hg, pulse is 85/min, and oxygen saturation is 91% on ambient air. No jugular venous distension is present, and mucous membranes are moist. Newly decreased breath sounds are noted over the left lower lung field. Heart rate is regular and without murmurs. No edema is present. A repeat chest x-ray reveals the following:
A bedside ultrasound shows the pleural effusion to be free-flowing and without loculations. The patient undergoes a left-sided diagnostic thoracentesis with approximately 100 mL of pale yellow fluid removed. Subsequent fluid analysis reveals a protein level of 4.0 mg/dL (serum level 6.6 mg/dL), lactate dehydrogenase (LDH) of 120 U/L (serum level 160 U/L), and pH of 7.31. Gram stain of the pleural fluid is negative; culture is pending. The patient asks what is going to be done about the “fluid on his lung.” Which of the following is the most appropriate response to the patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 66-year-old man comes to the office for follow-up of chronic obstructive pulmonary disease. He reports breathlessness with daily activities such as unloading groceries and showering, and rarely leaves the house due to dyspnea. The patient also experiences frightening moments of panic, struggling to regain his breath after overexerting himself. He has stopped volunteering at his church due to concern about “losing control” of his breathing in public. Over the previous year, the patient had 3 acute exacerbations treated with outpatient oral corticosteroids and one hospitalization for acute hypercapnic respiratory failure that resolved after several days of noninvasive ventilation. He is on long-term oxygen therapy. The patient smoked about 1 pack of cigarettes daily for 40 years and quit 10 years ago. Additional medical history includes atrial fibrillation, coronary artery disease, and a stable 4.5-cm abdominal aortic aneurysm. Temperature is 36.7 C (98.1 F), blood pressure is 140/96 mm Hg, pulse is 82/min, and respirations are 20/min. Oxygen saturation is 86% on room air and 93% on 2 L/min oxygen via nasal cannula. BMI is 31.5 kg/m2. Results of pulmonary function testing are shown below.
Forced vital capacity (FVC)
67%
Forced expiratory volume in 1 second (FEV1)
42%
FEV1/FVC ratio (FEV1%)
61%
Which of the following features most strongly indicates an increased risk of mortality for this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
A 46-year-old man comes to the office due to a 3-day history of cough, wheezing, and shortness of breath. Symptoms started a week ago with nasal congestion, sore throat, and body aches. The cough is productive of thin, whitish sputum. The patient has no fever, chills, chest pain, or abdominal pain. He has asthma managed with budesonide-formoterol as needed. Since yesterday, he has used the inhaler multiple times without significant symptom relief. His other medical condition is hypertension. He does not use tobacco, alcohol, or illicit drugs. Temperature is 36.7 C (98.1 F), blood pressure is 138/74 mm Hg, pulse is 86/min, and respirations are 20/min. Pulse oximetry is 96% on room air. The patient speaks in full sentences. He appears mildly uncomfortable but does not use accessory respiratory muscles. Jugular venous pressure is normal. There is no nasal sinus tenderness. The pharyngeal mucosa is without exudates. Bilateral expiratory wheezing with prolonged expiration is noted. Inspiratory breath sounds are normal. Heart sounds are normal. Peak expiratory flow is 30% lower than his prior baseline. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
The following vignette applies to the next 2 items.
A 59-year-old man comes to the office for a routine wellness examination. The patient’s medical history includes chronic bronchitis, hypertension, hypertriglyceridemia, and basal cell carcinoma. He smokes a pack of cigarettes per day, with a total 40-pack-year history. The patient typically consumes 1 or 2 cans of beer each night. Family medical history is remarkable for heart disease and diabetes mellitus. The patient had a normal screening colonoscopy 5 years ago. A chest x-ray from a year ago shows changes consistent with chronic bronchitis.
Item 1 of 2
The patient asks if he is at increased risk for lung cancer because of his smoking history. What is the most appropriate response by the physician?CorrectIncorrect -
Question 18 of 40
18. Question
Item 2 of 2
The patient says he enjoys smoking very much and is reluctant to stop because he has smoked since age 19. He asks about the benefits of smoking cessation. What is the most appropriate response by the physician?CorrectIncorrect -
Question 19 of 40
19. Question
The following vignette applies to the next 2 items.
A 38-year-old woman comes to the office due to worsening asthma symptoms for 2-3 days. She has shortness of breath, wheezing, and productive cough. The patient describes thick sputum that was blood-tinged yesterday. She was diagnosed with asthma 12 years ago but says that it had not been this bad until last year. For the past year the patient has had 2 hospitalizations for asthma exacerbations but has never been intubated. She completed a course of oral prednisone and azithromycin 2 months ago. Current medications include a daily fluticasone inhaler and as-needed albuterol inhaler. The patient reports no decrease in appetite or weight loss and has not travelled outside of her home state of New Jersey in the past 2 years. She works as a school teacher and does not use tobacco, alcohol, or illicit drugs. The patient has no second-hand tobacco exposure and no known allergies. Her grandmother also has asthma. Temperature is 37 C (98.6 F), blood pressure is 123/80 mm Hg, pulse is 94/min, and respirations are 16/min. Pulse oximetry shows 95% on room air. Pulmonary examination reveals scattered wheezes. Heart sounds are normal. There is no clubbing, peripheral edema, or skin rashes. Complete blood count shows the following:
Hemoglobin
13.0 g/dL
Platelets
200,000/mm3
Leukocytes
11,500/mm3
Neutrophils
65%
Lymphocytes
22%
Eosinophils
10%
Monocytes
3%
Item 1 of 2
Chest x-ray reveals patchy bilateral upper lobe infiltrates and prominent bronchial markings. Which of the following is the best next step in diagnosing the cause of this patient’s worsening symptoms?
CorrectIncorrect -
Question 20 of 40
20. Question
Item 2 of 2
Further laboratory evaluation of the patient shows a serum total IgE level of >1,000 ng/mL. High-resolution CT scan of the lungs confirms the presence of bilateral upper lobe infiltrates and central bronchiectasis. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 21 of 40
21. Question
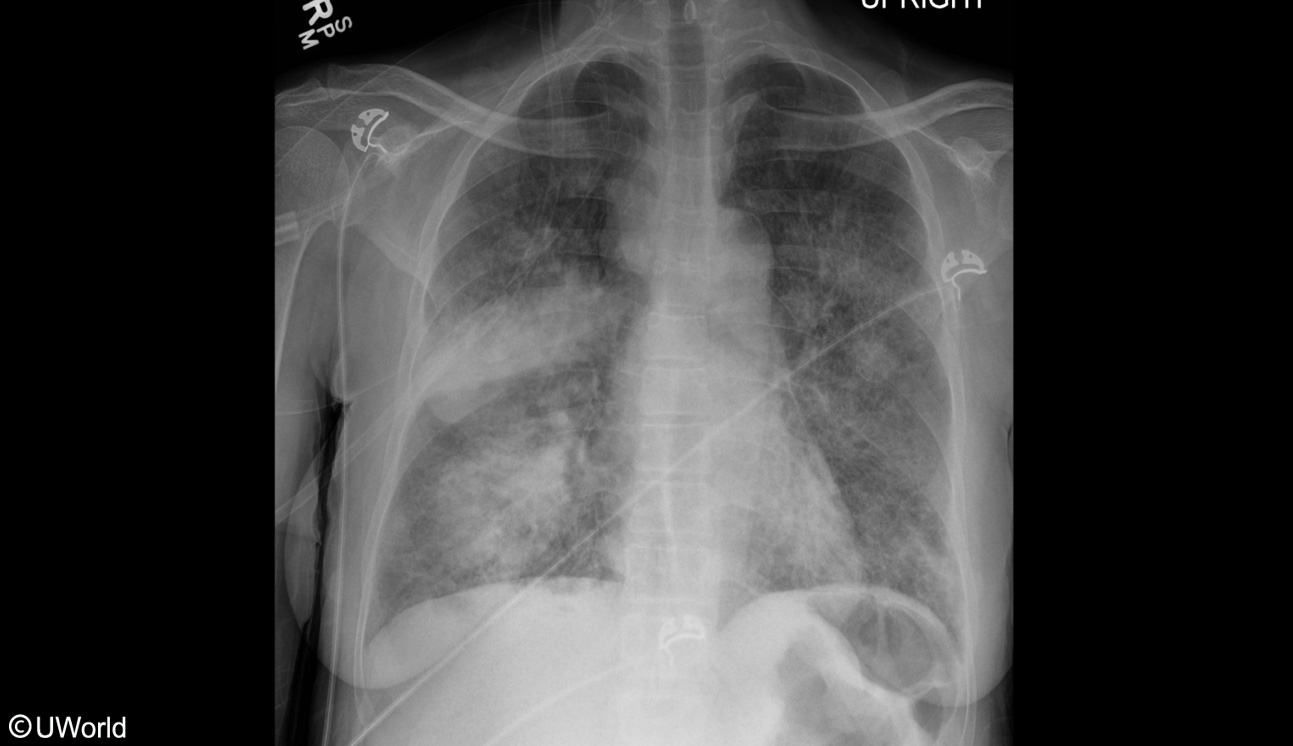
A 58-year-old woman comes to the emergency department due to fever, confusion, and malaise beginning 24 hours ago. The patient has an 8-year history of rheumatoid arthritis. Current medications include methotrexate, low-dose prednisone, as well as indomethacin as needed. Temperature is 38.9 C (102 F), pulse is 109/min, blood pressure is 73/40 mm Hg, respirations are 24/min, and oxygen saturation is 92% on 6 L/min oxygen. Weight is 80 kg (176 lb). Physical examination shows an ill-appearing woman with dorsocervical and central fat deposition but slim extremities. Mucous membranes appear moist. Laboratory studies reveal a leukocyte count of 22,000/mm3, serum creatinine of 1.7 mg/dL, and blood glucose level of 228 mg/dL. Chest x-ray is shown in the image below:
Broad spectrum antibiotics are initiated. The patient remains hypotensive after rapid administration of 2.5 L crystalloid fluid and continuous infusions of norepinephrine. A second vasopressor agent is added. Which of the following is the most appropriate recommendation regarding glucocorticoid therapy for this patient?
CorrectIncorrect -
Question 22 of 40
22. Question
The following vignette applies to the next 3 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
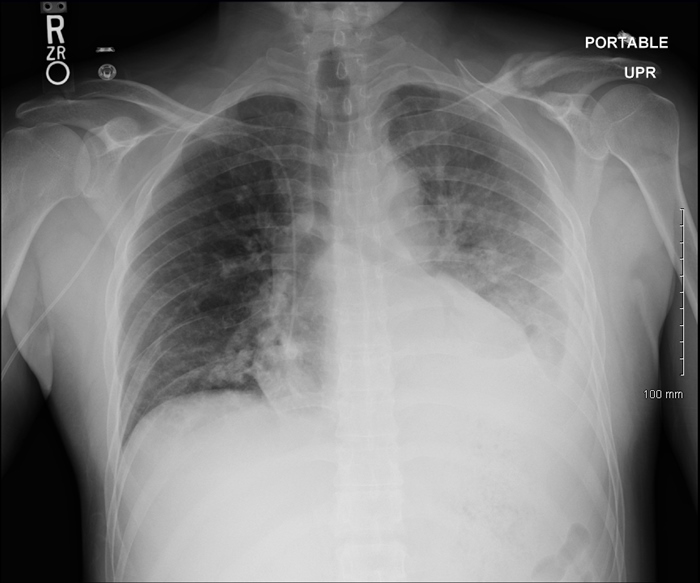
A 66-year-old woman is evaluated at the bedside for shortness of breath and anxiety that began suddenly in the early morning. The patient was admitted to the hospital 4 days ago after she slipped and fell on her icy driveway, resulting in a displaced femoral neck fracture. She underwent immediate orthopedic repair. The patient has no chest pain, cough, or hemoptysis. Medical history is significant for hypertension and dyslipidemia. Blood pressure is 118/62 mm Hg, pulse is 122/min, and respirations are 28/min. Pulse oximetry readings are 88% on room air and 93% on 2 L/min of oxygen. Cardiopulmonary examination reveals regular tachycardia and tachypnea but is otherwise unremarkable. Portable chest x-ray is shown in the exhibit. ECG demonstrates sinus tachycardia with an incomplete right bundle-branch block and T-wave inversions in leads III and V1 through V4. Serum chemistry values are within normal limits, and cardiac troponin I level is 2.78 ng/mL (normal: <0.01).

Item 1 of 3
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
Item 2 of 3
CT angiography reveals bilateral segmental pulmonary emboli, a small right-sided pleural effusion, and a wedge-shaped consolidation in the right lower lobe. Therapeutic anticoagulation is initiated with intravenous unfractionated heparin. Blood pressure is 121/79 mm Hg and pulse is 118/min and regular. In addition to the elevated cardiac troponin I level, the patient’s plasma B-type natriuretic peptide level is 524 pg/mL (normal: <100). Arterial blood gas analysis reveals pH 7.49, PaCO2 26 mm Hg, and an elevated alveolar-arterial oxygen gradient. Echocardiography shows moderate hypokinesis and dilation of the right ventricle, normal left ventricular ejection fraction, and no regional wall motion abnormalities. The estimated pulmonary artery systolic pressure is 50 mm Hg. Which of the following best signifies an increased risk of clinical deterioration in this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
Item 3 of 3
The following day, the patient’s shortness of breath is improved. She continues to receive the heparin infusion, and the activated PTT is in a therapeutic range. The surgical site is healing appropriately. Plans for oral anticoagulation after discharge are being discussed. The patient reports no chest pain or dizziness. Prior to morning rounds, however, she expectorates approximately 1 teaspoon of dark blood. Temperature is 37.6 C (99.7 F), blood pressure is 136/79 mm Hg, pulse is 82/min, and respirations are 20/min. Pulse oximetry reading is 94% on 2 L/min oxygen. Chest x-ray is unchanged. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 75-year-old man is admitted to the intensive care unit due to septic shock and acute respiratory distress syndrome. The patient’s medical history is significant for relapsed refractory multiple myeloma and malignant bone pain requiring long-term opioid therapy. Despite a prolonged course of mechanical ventilation, his condition deteriorates; he is transitioned to comfort-oriented care in accordance with his advance directive. The patient is extubated to a simple oxygen face mask. Morphine is administered intravenously to ease air hunger, and glycopyrrolate is given to reduce heavy secretions. Thirty minutes later, he is gurgling loudly. Pulse is 118/min and respirations are 8/min. Oxygen saturation is 90%. Examination reveals a cachectic, obtunded man with irregular, rattling respirations. Pupils are pinpoint bilaterally. Skin is diaphoretic. In addition to suctioning the oropharynx, what is the most appropriate next step in management at this time?
CorrectIncorrect -
Question 26 of 40
26. Question
A 68-year-old man with chronic obstructive pulmonary disease (COPD) comes to the clinic due to a 9-kg (20-lb) weight loss over the last 2 years. He describes his appetite as “all right” but does say that he is eating less. The patient reports poor taste, fatigue, chronic dyspnea, productive cough, and occasional nausea. He also reports insomnia most nights of the week with poor concentration during the day. He has no night sweats, fevers, chills, dysphagia, change in bowel habits, blood in the stool, or dysphoria. He has had 3 hospitalizations for COPD exacerbation over the past 2 years during which he was treated with short courses of prednisone. The patient has smoked 2 packs of cigarettes daily for 42 years. He reports feeling “bad” for smoking all these years and is trying to quit but says, “It’s just very hard.” The patient lives alone and often feels lonely. His other medical problems include hypertension and hyperlipidemia. His last colonoscopy was 5 years ago and included removal of 2 hyperplastic polyps. He does not use alcohol or recreational drugs. Family history is not significant. Temperature is 36.7 C (98 F), blood pressure is 130/80 mm Hg, pulse is 80/min, and respirations are 18/min. BMI is 17 kg/m2. Pulse oximetry shows 91% on ambient air. Physical examination reveals moist mucous membranes, normal jugular venous pressure, and distant S1 and S2. Lung examination reveals prolonged expiration, increased resonance to percussion bilaterally, and increased anterior-to-posterior diameter of the chest. The abdomen is soft and nontender. There is no hepatomegaly, splenomegaly, or masses. Testing of the stool for occult blood is negative. No edema or lymphadenopathy is present. Neurologic examination is within normal limits. The patient’s affect is normal. Laboratory results are as follows:
Complete blood count
Leukocytes
3,800/mm3
Hemoglobin
13.1 g/dL
Platelets
180,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
4.2 mEq/L
Creatinine
0.6 mg/dL
Calcium
9.2 mg/dL
Liver function studies
Total protein
7.0 g/dL
Albumin
3.7 g/dL
Total bilirubin
0.3 mg/dL
Alkaline phosphatase
70 U/L
Aspartate aminotransferase
12 U/L
Alanine aminotransferase
24 U/L
Hemoglobin A1c
5.4%
Thyroid-stimulating hormone
2.4 µU/mL
Erythrocyte sedimentation rate
17 mm/h
Chest x-ray reveals hyperexpansion of bilateral lung fields with diaphragmatic flattening. Which of the following is the most likely cause of this patient’s weight loss?
CorrectIncorrect -
Question 27 of 40
27. Question
A 38-year-old woman in the intensive care unit is evaluated for worsening hypoxia. The patient was admitted a week ago due to dyspnea and nonproductive cough. At that time, diffuse crackles were found on lung examination, and chest x-ray revealed bilateral infiltrates. The patient smoked crack cocaine and used intravenous heroin prior to symptom onset. She required endotracheal intubation due to hypoxic respiratory failure and has been mechanically ventilated. Her respiratory condition has gradually improved over the past week, but in the last 2 days she has required a higher fraction of inspired oxygen. The patient has also had increased tracheobronchial secretions. Temperature is 38.9 C (102 F), blood pressure is 112/71 mm Hg, pulse is 114/min, and respirations are 22/min. Central venous pressure is 8 cm H2O. Lung auscultation reveals bilateral crackles. Heart sounds are normal with no murmur or gallop. The abdomen is soft and nondistended with normoactive bowel sounds. She has no dependent edema or skin rash. Ventilator settings, arterial blood gases, and laboratory results are as follows:
Two days ago
Today
Ventilator settings
Tidal volume
380 mL
380 mL
Fraction of inspired oxygen
40%
70%
Positive end-expiratory pressure
5 cm H2O
10 cm H2O
Arterial blood gases
pH
7.40
7.45
PaO2
90 mm Hg
60 mm Hg
PaCO2
38 mm Hg
32 mm Hg
Leukocytes
11,000/mm3
18,000/mm3
Repeat chest x-ray reveals asymmetric worsening of the lung infiltrate. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 39-year-old woman comes to the office due to a nagging cough. Two weeks ago, the patient had a mild upper respiratory illness which resolved spontaneously after several days. Since then, she has had cough that is productive of minimal clear sputum. The patient has had no shortness of breath or chest pain. She took unexpired, leftover dextromethorphan for 2 days. The patient’s only other medical condition is major depression, for which she takes sertraline. She does not use tobacco, alcohol, or illicit drugs. Vital signs and physical examination show no abnormalities. Use of dextromethorphan is most concerning for which of the following in this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
The following vignette applies to the next 2 items
A 60-year-old Caucasian man is admitted to the hospital with an episode of bacterial pneumonia. Upon review of his past medical history, you notice that he has had three recent admissions within the past seven months for bacterial pneumonia. All the episodes were successfully treated with intravenous antibiotics. Previous chest x-ray comparisons reveal that the infiltrate always occurs at the right middle lobe and leaves a persistent scar. The scar was not noted on the chest x-ray prior to the episodes of pneumonia. He has a 50-pack year history of smoking. He quit smoking 10 years ago.
Item 1 of 2
Which of the following is the most likely cause of the patient’s recurrent pneumonia?
CorrectIncorrect -
Question 30 of 40
30. Question
Item 2 of 2
Which of the following is the most likely to definitively confirm the diagnosis in this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
The following vignette applies to the next 2 items
A 61-year-old Caucasian female presents to her primary care physician complaining, “I feel terrible lately, coughing much worse than normal. Just very nauseated and tired. My head is pounding and my husband says I’m especially irritable.” She also attests to a gradual increase in thirst and a generalized weakness. She has a history of mitral valve prolapse and well-controlled hypertension. Her only medications at this time are atenolol and a multivitamin. From the age of 19, she has smoked one pack of cigarettes per day. She drinks socially on the weekends. Physical examination reveals a thin, pale woman who is mildly wheezing but otherwise appears normal. Chest x-ray shows a four centimeter perihilar mass and increased hilar opacity.
Serum electrolytes
Sodium
124 mEq/L
Potassium
3.5 mEq/L
Bicarbonate
22 mEq/L
BUN
18 mg/dL
Creatinine
0.8 mg/dL
Item 1 of 2
What is the most likely diagnosis?
CorrectIncorrect -
Question 32 of 40
32. Question
Item 2 of 2
What is the most appropriate means of correcting this patient’s hyponatremia?
CorrectIncorrect -
Question 33 of 40
33. Question
A 64-year-old man comes to the emergency department with a 3-day history of fever, shortness of breath, and worsening productive cough. The patient also reports sharp, intermittent, right-sided chest pain. He has a history of hypertension and type 2 diabetes mellitus. The patient has smoked a pack of cigarettes daily for 20 years. Temperature is 38.9 C (102 F), blood pressure is 110/60 mm Hg, pulse is 114/min, and respirations are 32/min. The patient’s pulse oximetry shows 86% on room air. Examination reveals diffuse crackles over the lung fields. Heart sounds are regular with no murmurs or gallops. Chest x-ray reveals bilateral consolidation and infiltrates. He is started on empiric intravenous antibiotics after obtaining cultures but requires endotracheal intubation due to respiratory failure. Which of the following is most reliable for confirming tracheal (rather than esophageal) endotracheal tube placement in this patient?
CorrectIncorrect -
Question 34 of 40
34. Question
A 66-year-old man comes to the office due to 3 months of slowly worsening nonproductive cough and shortness of breath. He has also had night sweats, excessive fatigue, and sharp, episodic right-sided chest pain. The patient has lost approximately 5 kg (11 lb) during this period. He has a history of hypertension and takes chlorthalidone. He has smoked a half-pack of cigarettes daily for the past 50 years. The patient worked in a shipbuilding factory until his early 40s and then began working in the automobile industry. Temperature is 36.7 C (98 F), blood pressure is 130/80 mm Hg, pulse is 84/min, and respirations are 14/min. No jugular venous distension or lymphadenopathy is present. There is dullness to percussion and decreased breath sounds over the right lower chest. Heart sounds are normal with no murmur. The abdomen is soft and nontender with no hepatosplenomegaly. No edema is present. Chest imaging reveals a moderate right-sided pleural effusion with irregular pleural thickening and calcifications, but no lung parenchymal abnormalities. A thoracentesis is performed and yields serosanguineous pleural fluid; pleural fluid analysis reveals the following:
Cell count
Erythrocytes
350/mm³
Leukocytes
1,200/mm³
Lymphocytes
65%
Total protein
3.5 g/dL (serum protein = 5 g/dL)
Glucose
40 mg/dL (serum glucose = 110 mg/dL)
Lactate dehydrogenase
840 U/L
Triglycerides
35 mg/dL
pH
7.2
Cytology
negative for malignant cells
Which of the following is the most likely cause of this patient’s pleural effusion?
CorrectIncorrect -
Question 35 of 40
35. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 40-year-old woman is brought to the emergency department by paramedics after a motor vehicle collision. She was driving and wearing a seatbelt when her car was hit by another vehicle from the opposite direction. Her car went off the road and hit a tree. When paramedics arrived at the scene, the patient was noted to have an open femur fracture but was alert and oriented. Her medical issues include hyperlipidemia and mitral valve prolapse with mild regurgitation. She takes no medications. The patient undergoes open reduction and internal fixation of the femur fracture. She receives intravenous fluids and pain control postoperatively. The next morning she experiences left-sided chest discomfort and shortness of breath. Temperature is 37.6 C (99.7 F), blood pressure is 120/70 mm Hg, pulse is 100/min, and respirations are 30/min. Pulse oximetry shows 84% on room air. Physical examination reveals an area of tenderness over the left chest wall where the seatbelt was placed. On pulmonary examination, the patient has rales over the left upper lung. A 2/6 holosystolic murmur is present over the cardiac apex. Laboratory results are as follows:
Complete blood count
Leukocytes
7,500/mm3
Hemoglobin
10.8 g/dL
Platelets
202,000/mm3
Serum chemistry
Creatinine
0.8 mg/dL
ECG shows sinus tachycardia with no ST-segment or T-wave changes. Chest x-ray shows irregular opacification predominantly of the left upper lung.
Item 1 of 2
What is the most likely cause of this patient’s respiratory symptoms?
CorrectIncorrect -
Question 36 of 40
36. Question
Item 2 of 2
Adequate pain control and supplemental oxygen by nasal cannula is provided and the patient’s respiratory distress improves. Pulse oximetry shows 96% on 3 L/min supplemental oxygen. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
A 71-year-old man is admitted to the intensive care unit due to influenza complicated by bacterial pneumonia and acute respiratory distress syndrome. The patient completes a course of intravenous antibiotic therapy, and his clinical status steadily improves. He is extubated after 8 days of mechanical ventilation. The patient’s cough strength is reduced, but he continues to raise a moderate amount of thick secretions that require intermittent oral suctioning. He is diffusely weak and requires assistance to reposition in the bed. At night, he becomes disoriented and pulls at his lines, requiring cloth mittens and soft restraints. During the day, the patient alternates between periods of agitation, drowsiness, and clarity. Temperature is 36.1 C (97 F), blood pressure is 108/66 mm Hg, pulse is 93/min, and respirations are 20/min. Pulse oximetry shows 96% on 3 L/min of supplemental oxygen by nasal cannula. Results of serum chemistry testing are within normal limits, and complete blood count reveals normocytic anemia with a hemoglobin level of 8.5 g/dL. Which of the following interventions is most strongly indicated at this time to promote this patient’s recovery?
CorrectIncorrect -
Question 38 of 40
38. Question
A 64-year-old man comes to the physician for evaluation prior to right total hip arthroplasty. He has a chronic cough with a modest amount of sputum production, which he attributes to smoking. He otherwise feels well. His chronic medical conditions include hypertension, coronary artery disease, and severe degenerative joint disease. He has an 80-pack-year smoking history and currently smokes one and a half packs of cigarettes daily. A chest x-ray taken about a week ago reveals a 2-cm pulmonary nodule in the left upper lobe. Which of the following clinical or radiographic features suggests a benign cause of the pulmonary nodule?
CorrectIncorrect -
Question 39 of 40
39. Question
A 79-year-old man with metastatic prostate cancer is brought to the emergency department by his caretaker due to concern about his breathing. The patient takes a short-acting opioid every 4 hours and applies a transdermal fentanyl patch for malignant bone pain; the dose of the patch was increased 3 days ago due to inadequate pain control. The caretaker reports that the patient’s breathing “has been strange” since this morning, but he has had no fever or cough. Temperature is 37.4 C (98.6 F), blood pressure is 112/78 mm Hg, pulse is 115/min, and respirations are 24/min. Oxygen saturation is 90% on room air. On physical examination, the patient is chronically ill-appearing and drowsy but arouses easily to voice. Bilateral pupils are small but reactive. The lungs are clear to auscultation with normal tidal air movement bilaterally. The patient continues to have significant pain with any repositioning. Chest x-ray reveals stable appearance of previously known blastic lesions in the thoracic spine and ribs but no acute abnormalities. ECG shows sinus tachycardia. Blood cell counts and urinalysis are normal. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 46-year-old previously healthy man comes to the hospital due to a day of pleuritic chest pain and dyspnea. The patient has had right leg swelling for the past week. He has smoked a pack of cigarettes daily for 12 years and works as a truck driver. Cardiopulmonary examination is within normal limits with the exception of tachycardia. The right lower extremity is swollen and tender up to the mid thigh. CT pulmonary angiography shows a right-sided pulmonary embolism, and duplex venous ultrasound reveals a thrombus in the right femoral vein. The patient is admitted to the hospital and started on low-molecular-weight heparin therapy. During morning rounds, he suddenly becomes unresponsive and has no palpable pulses despite electrical activity consistent with sinus bradycardia at 50/min on the cardiac monitor. Advanced cardiac life support measures, including external chest compressions and endotracheal intubation, are implemented. After 4 minutes of chest compressions, he is still pulseless and the monitor shows sinus bradycardia. Which of the following is the best next step in management of this patient?
CorrectIncorrect
