Time limit: 0
Quiz Summary
0 of 33 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 33 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 33
1. Question
A 19-year-old woman is admitted to the intensive care unit after an accidental heroin overdose. The patient has a history of injection drug use and was found on the floor by her friend, unresponsive with a hypodermic needle in her arm. She received naloxone and cardiopulmonary resuscitation by paramedics on the scene. Subsequent evaluation reveals extensive anoxic brain injury. On hospital day 8, she remains comatose and apneic with absent brainstem reflexes. Brain death has been confirmed by the consulting neurologist, and the organ procurement organization has been notified of the patient’s status. Her parents have arrived at the hospital for a family meeting with the physician. Which of the following is the best approach to organ donation discussion with this patient’s family?
CorrectIncorrect -
Question 2 of 33
2. Question
A 20-year-old woman comes to the office due to decreased exercise tolerance. She plays on her college soccer team, and her coach is concerned about a noticeable decline in performance over the last 3 months. The patient reports cough, dyspnea, and chest tightness starting 5-10 minutes after commencing exercise; these symptoms abate halfway through practice and games. She is asymptomatic at other times. The patient has no known medical conditions. Her brother has ostium secundum atrial septal defect, and her mother has allergic rhinitis. Vesicular breath sounds are heard on lung examination. Digital clubbing is absent. Cardiac auscultation shows normal splitting of S2 in the left upper sternal border during inspiration and no murmurs. Jugular venous pressure is normal. There is no lower extremity edema. Which of the following is the most appropriate next step for establishing the diagnosis in this patient?
CorrectIncorrect -
Question 3 of 33
3. Question
A 73-year-old man comes to the emergency department with fever and chest discomfort. He was hospitalized with right lower-lobe pneumonia 3 months ago and improved with antibiotics. He has since had an intermittent cough and a 4.5-kg (10-lb) weight loss. The patient is a life-long nonsmoker. He has a long history of Parkinson’s disease with gait instability along with hypertension and acid-reflux disease. His temperature is 38.3 C (101 F), blood pressure is 122/70 mm Hg, heart rate is 105/min, and respirations are 24/min. Examination shows upper-extremity rigidity, resting tremor, mild dysarthria, and frequent drooling. Lung examination shows crackles and dullness at the right base. Extremities are warm to the touch. The white blood cell count is 13,500/µL. Chest x-ray shows a right middle-lobe infiltrate. Intravenous antibiotics are started. Which of the following tests is most helpful in evaluating this patient?
CorrectIncorrect -
Question 4 of 33
4. Question
The following vignette applies to the next 3 items.
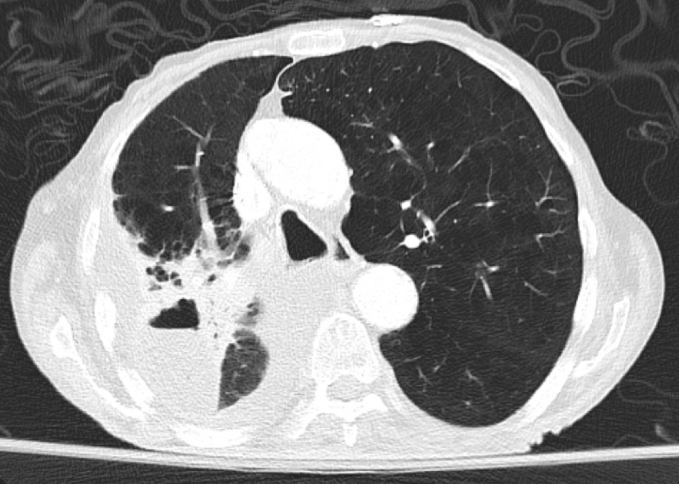
A 60-year-old man with a history of chronic obstructive pulmonary disease comes to the office due to hemoptysis. For the past several days, he has had increasing cough with greenish-yellow sputum. He also had 2 episodes of blood-streaked sputum, which prompted the clinic visit. The patient has mild dyspnea but no fever or chest pain. His other medical problems are peripheral vascular disease and osteoarthritis. His current medications include aspirin, inhaled fluticasone and salmeterol, and ipratropium. He continues to smoke 1/2 pack of cigarettes daily and drinks alcohol occasionally. The patient had a screening CT scan 2 years ago that was negative for lung mass. His father died of lung cancer. Blood pressure is 140/95 mm Hg and heart rate is 100/min. The patient’s pulse oximetry shows 95% on room air. Lung auscultation reveals bilateral expiratory wheezing.
Item 1 of 3
Which of the following is the best initial step in management of this patient?
CorrectIncorrect -
Question 5 of 33
5. Question
Item 2 of 3
The initial workup reveals no significant abnormality. The patient is started on glucocorticoid therapy and additional inhaled albuterol. Which of the following is the best next step in management?
CorrectIncorrect -
Question 6 of 33
6. Question
Item 3 of 3
Soon after the patient leaves the office, his wife calls and requests information about her husband’s condition. She is also the treating physician’s patient. Which of the following is the most appropriate response to her request?
CorrectIncorrect -
Question 7 of 33
7. Question
A 24-year-old woman with a history of asthma comes to the emergency department at 32 weeks gestation with a 5-day history of increased dyspnea, wheezing, and cough. Her asthma was previously well-managed with a combination fluticasone-salmeterol inhaler twice daily, but the patient stopped using it when she discovered she was pregnant. She reports no nasal congestion, sore throat, or sinus pain. The patient has no other medical conditions, and her pregnancy has progressed normally. Her only other medication is a prenatal multivitamin. She does not use tobacco, alcohol, or illicit drugs. Her father has a history of asthma. On examination, the patient appears to be in mild respiratory distress. She is afebrile. Blood pressure is 110/68 mm Hg, pulse is 104/min, and respirations are 21/min. Pulse oximetry is 94% on room air. Lung examination reveals inspiratory and expiratory wheezes with a prolonged exhalation phase. Heart sounds are normal. Mild bilateral pitting pedal edema is present; there is no calf tenderness in either leg. Fetal heart rate monitoring is reassuring. Nebulized albuterol and inhaled ipratropium are administered and provide some relief. On repeat assessment shortly afterward, the patient continues to feel short of breath, and wheezing is still present on examination. Arterial blood gas analysis shows a pH of 7.45, PaCO2 of 26 mm Hg, and PaO2 of 100 mm Hg on 2 L of oxygen by nasal cannula. What is the best next step in management of this patient?
CorrectIncorrect -
Question 8 of 33
8. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 27-year-old man comes to the emergency department (ED) with worsening shortness of breath. The patient uses a combination inhaled beta-agonist and corticosteroid inhaler for asthma, but ran out of his medications 10 days ago. Temperature is 37.2 C (99 F), blood pressure is 164/84 mm Hg, pulse is 110/min, and respirations are 28/min. Oxygen saturation is 87% on room air and improves to 92% on 3 liters/min by nasal cannula. The patient is alert and speaking in partial sentences. Accessory muscle recruitment is noted. Lung examination is significant for reduced air movement and diffuse wheezing bilaterally. Peak expiratory flow rate is 50% of his personal best a few months ago when the asthma was under control.
Item 1 of 2
Which of the following is the most appropriate immediate step in management of this patient?
CorrectIncorrect -
Question 9 of 33
9. Question
Item 2 of 2
While in the emergency department, the patient is treated with alternating doses of nebulized albuterol and ipratropium along with intravenous methylprednisolone. One hour after treatment is started, his respirations are more labored. The patient is diaphoretic and exhibiting deep suprasternal retractions. He appears agitated and has difficulty following instructions. Temperature is 37.2 C (99 F), blood pressure is 110/74 mm Hg, pulse is 126/min, and respirations are 28/min. Oxygen saturation is 95% on nonrebreather mask. Lung examination is significant for markedly reduced air entry throughout with minimal wheezing bilaterally. Which of the following is the most important next step in management?
CorrectIncorrect -
Question 10 of 33
10. Question
A 53-year-old woman is admitted to the hospital due to a 3-day history of worsening dyspnea. On examination, the patient is tachypneic; diffuse, wet, inspiratory crackles are present on pulmonary auscultation. Chest x-ray reveals bilateral patchy opacities. Arterial blood gas analysis shows that the patient’s alveolar-arterial gradient (PAO2 − PaO2) is markedly increased. Although the patient receives 100% oxygen via a face mask, she has persistent hypoxemia and respiratory distress. Consequently, she is intubated and placed on mechanical ventilation with 100% oxygen and positive end-expiratory pressure (PEEP). Results of arterial oxygen measurements are as follows:
Arterial partial pressure
of oxygen (mm Hg)O2 saturation
Room air
40
75%
100% oxygen via face mask
43
78%
100% oxygen & PEEP
80
96%
The patient’s improved oxygenation following PEEP application is most likely due to a decrease in which of the following?
CorrectIncorrect -
Question 11 of 33
11. Question
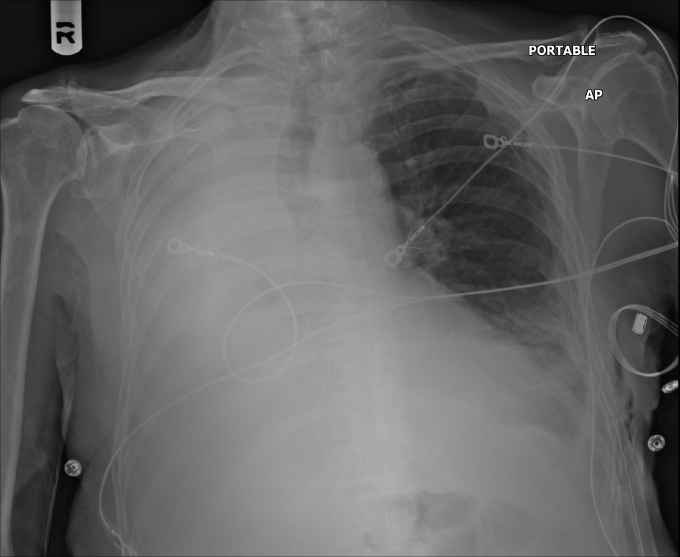
A 65-year-old man comes to the emergency department due to worsening dyspnea. The patient has a history of cigarette smoking and chronic productive cough. He experienced increasing shortness of breath today without fever, chills, or chest pain. Temperature is 36.7 C (98 F), blood pressure is 135/85 mm Hg, pulse is 94/min, and respirations are 24/min. Pulse oximetry shows 86% on room air. He has decreased breath sounds over the right chest. Chest x-ray is shown in the exhibit. Which of the following is the most likely cause of this patient’s radiographic findings?
 CorrectIncorrect
CorrectIncorrect -
Question 12 of 33
12. Question
A 32-year-old woman comes to the emergency department due to 4 weeks of worsening cough, shortness of breath, and low-grade fevers. She also has had an unintentional weight loss of 4.5 kg (10 lb) over the past 3 months. Temperature is 37.1 C (98.8 F), blood pressure is 120/70 mm Hg, pulse is 102/min, and respirations are 22/min. Pulse oximetry shows 86% on ambient air. Lung auscultation reveals bilateral crackles. There are no heart murmurs, and jugular venous pressure is normal. Chest x-ray reveals diffuse interstitial infiltrates. The patient undergoes bronchoscopy; methenamine silver staining of the bronchoalveolar lavage specimen is shown in the image.
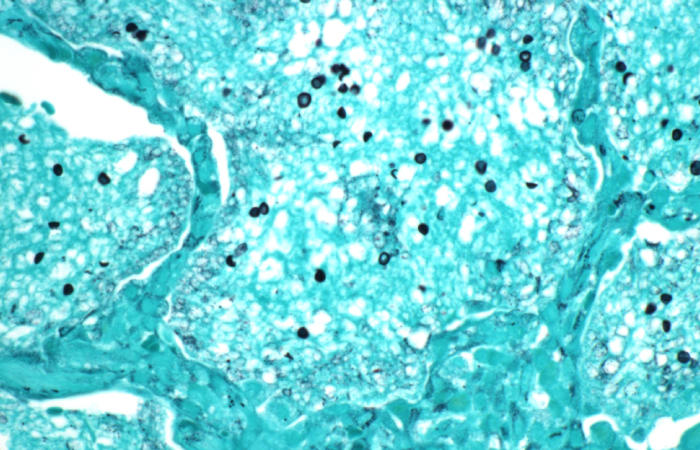
Which of the following is the most appropriate pharmacotherapy for this patient’s current condition?
CorrectIncorrect -
Question 13 of 33
13. Question
A 56-year-old, previously healthy man is admitted to the intensive care unit for acute respiratory distress syndrome due to viral pneumonia. The patient requires prolonged mechanical ventilation with deep sedation, prone positioning, and paralytic agents. He develops hypoactive delirium, which slowly improves with sedation washout. After 7 days, the patient is successfully extubated and discharged to a skilled rehabilitation center. A week later, he is participating in daily physical therapy. The patient requires 2-person assistance to stand due to diffuse weakness. He has been irritable and confused in the evenings and is prescribed zolpidem to assist with sleep. Montreal Cognitive Assessment score is 25/30, with deficits in attention and memory. Neurologic examination reveals flattened affect and mild psychomotor retardation. He is on extended sick leave from his job as an air traffic controller. Which of the following statements best represents this patient’s long-term prognosis?
CorrectIncorrect -
Question 14 of 33
14. Question
A 36-year-old man comes to the emergency department due to sudden-onset left-sided chest pain for the past 2 hours. The patient says, “It feels like someone stabbed my chest and I have difficulty breathing.” The pain does not radiate and worsens with deep inspiration and movements. He has had no nausea, diaphoresis, or lightheadedness. The patient has a history of type 1 diabetes mellitus, and a month ago he developed right foot ulceration after stepping on a sharp piece of metal. His foot wound did not heal with nonsurgical treatments, and a week ago he underwent transmetatarsal amputation of the right first toe after evaluation revealed acute osteomyelitis of the metatarsal bone. The patient also experienced severe anaphylactic reaction after intravenous contrast was administered during CT angiography of the right lower extremity prior to the surgery. He has no other medical problems and does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 110/62 mm Hg, pulse is 106/min, and respirations are 24/min. The patient’s pulse oximetry shows 92% while breathing ambient air. Lung auscultation reveals pleural friction rub over the left lower chest. Heart sounds are regular with an accentuated pulmonary component of S2. There are no murmurs or gallops. The abdomen is soft and nontender. Right foot examination shows healing surgical wound with no erythema or drainage. There is no extremity edema or calf tenderness. ECG shows sinus tachycardia with no significant ST segment or T wave changes. Chest x-ray shows slight blunting of the left costophrenic angle. There are no parenchymal infiltrates or consolidation. Ventilation/perfusion scan is performed, which is reported as low probability for pulmonary embolism. Which of the following is the most likely diagnosis for this patient?
CorrectIncorrect -
Question 15 of 33
15. Question
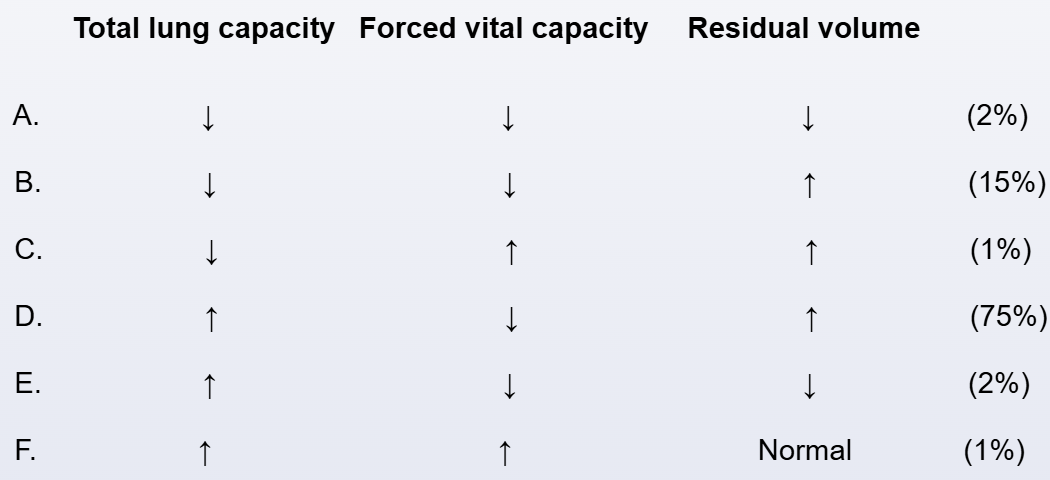
A 65-year-old man comes to the office due to worsening exertional dyspnea over the last 3 months. This past year he had 4 respiratory tract infections. The patient does not use alcohol or recreational drugs. He has smoked 1½ packs of cigarettes daily for 30 years. Temperature is 36.7 C (98.1 F), pulse is 76/min, blood pressure is 132/77 mm Hg, and respirations are 18/min. On physical examination, breath sounds are diffusely decreased. Chest radiograph reveals increased lucency of the lungs. This patient’s pulmonary function testing will most likely show which of the following patterns of findings?
 CorrectIncorrect
CorrectIncorrect -
Question 16 of 33
16. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 54-year-old man comes to the emergency department after an episode of syncope. While he was watching television 30 minutes ago, he experienced sudden-onset chest pressure followed by a syncopal episode. He regained consciousness within a minute but continues to have chest “heaviness” and shortness of breath. Two days ago, the patient returned home from an extended car trip. He has a history of hypertension, osteoarthritis, and prostate cancer treated with brachytherapy. He is a former smoker with a 15-pack-year history and does not use alcohol or illicit drugs. Temperature is 38.3 C (100.9 F), blood pressure is 81/50 mm Hg, pulse is 110/min and regular, respirations are 26/min, and pulse oximetry is 92% on room air. The lungs are clear to auscultation. Cardiac examination shows a nondisplaced point of maximal impulse, with no murmurs but an accentuated pulmonic component of S2. Laboratory results are as follows:
Complete blood count
Leukocytes
14,000/mm3
Hematocrit
40%
Platelets
320,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
4.6 mEq/L
Bicarbonate
22 mEq/L
Blood urea nitrogen
20 mg/dL
Creatinine
0.9 mg/dL
Glucose
105 mg/dL
Arterial blood gases on room air
pH
7.50
PaO2
74 mm Hg
PaCO2
26 mm Hg
Troponin T, serum
0.96 ng/mL (normal: <0.01)
ECG shows sinus tachycardia with nonspecific ST-segment and T-wave changes. CT angiography reveals filling defects in the bilateral main pulmonary arteries. Blood pressure after multiple fluid boluses is 85/60 mm Hg and pulse is 108/min.
Item 1 of 2
Which of the following findings in this patient is most predictive of increased 30-day mortality?
CorrectIncorrect -
Question 17 of 33
17. Question
Item 2 of 2
The patient develops progressive hypoxemia requiring 100% supplemental oxygen via a nonrebreather mask, but even with treatment his respiratory distress worsens and he becomes progressively confused and lethargic. Endotracheal intubation is performed and mechanical ventilation is initiated. Intravenous norepinephrine infusion is started due to persistent hypotension. Bedside echocardiography reveals right ventricular dilation and hypokinesis, but left ventricular contractility is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 18 of 33
18. Question
A 43-year-old man comes to the office due to a cough. The patient started with symptoms of nasal congestion, sore throat, and cough about 10 days ago, and most of the symptoms have since improved. However, the cough is persistent throughout the day and is productive of yellow sputum. He has no fever, chills, weight loss, or night sweats. The patient has had no prior respiratory problems, shortness of breath, sick contacts, or recent travel. He has taken lisinopril for hypertension and metformin for type 2 diabetes mellitus for the past 5 years. His last hemoglobin A1c was 6.6%. The patient has smoked half a pack of cigarettes daily for 5 years and is currently trying to quit. He drinks 1 or 2 cans of beer daily but does not use illicit drugs. Family history includes diabetes in multiple family members. Temperature is 36.1 C (97 F), blood pressure is 130/80 mm Hg, pulse is 65/min, and respirations are 14/min. The patient’s pulse oximetry shows 99% on room air. On examination, the patient is in no apparent distress and appears his stated age. Mucous membranes are moist, and no lymphadenopathy or jugular venous distension is present. Heart rate is regular with normal S1 and S2. Bilateral scattered rhonchi are auscultated, which clear after expectoration. No crackles, wheezing, or rubs are heard. Percussion is resonant throughout, and normal tactile fremitus is observed. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 19 of 33
19. Question
A 47-year-old woman comes to the office due to progressive exertional dyspnea and fatigue. She also reports painful episodes of bluish discoloration of the fingers and toes that are triggered by cold exposure and improve with rewarming. Medical history is significant for severe gastroesophageal reflux disease. Physical examination shows skin tightening over the fingers. The oral aperture is small, and scattered telangiectasias are present over the lips. Cardiac examination demonstrates an increased intensity of S2 over the upper left sternal border. Lungs are clear to auscultation with normal air movement and no crackles. The abdomen is soft with mild hepatomegaly. There is bilateral lower extremity pitting edema. Chest x-ray reveals no abnormalities. Results of office spirometry are as follows:
Forced vital capacity (FVC)
Normal
Forced expiratory volume in 1 second (FEV1)
Normal
FEV1/FVC ratio (%)
Normal
Which of the following is the most likely cause of this patient’s dyspnea?
CorrectIncorrect -
Question 20 of 33
20. Question
A 72-year-old woman is being treated in the intensive care unit for lobar pneumonia, septic shock, and respiratory failure with intravenous fluids, antibiotics, vasopressors, and mechanical ventilation. Her condition is improving and she is extubated on day 5. Within a few minutes of extubation, the patient develops stridor and is given intravenous dexamethasone and nebulized epinephrine. Her current examination shows blood pressure of 148/86 mm Hg, pulse of 102/min, and respirations of 30/min. Pulse oximetry shows 94% on nonrebreather mask. She has audible stridor and labored breathing with use of accessory muscles of respiration. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 21 of 33
21. Question
A 48-year-old man comes to the office for an initial visit. He says that he feels well and has no known medical conditions. The patient has a 20-pack-year smoking history and does not use alcohol or recreational drugs. He is counseled on smoking cessation. During the discussion of how smoking affects lung function, the patient is shown a graph of the expected change in forced expiratory volume in 1 second (FEV1) over time if he continues to smoke at the same rate (Curve D shown below). Which of the following curves most likely demonstrates the expected FEV1 over time if this patient were to stop smoking now?
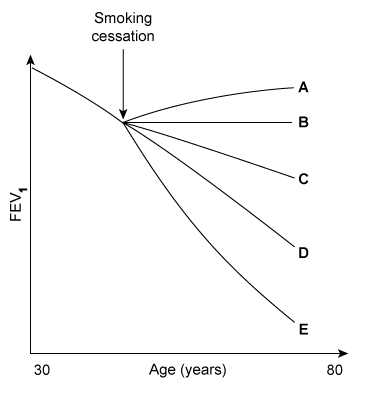 CorrectIncorrect
CorrectIncorrect -
Question 22 of 33
22. Question
An 82-year-old man is brought to the emergency department due to 3 weeks of worsening cough and low-grade fever. The cough was dry initially but has been associated with yellow, sour-tasting phlegm over the past several days. The patient’s medical history is significant for hypertension, chronic kidney disease, and vascular dementia. He has never smoked and drinks a glass of wine on social occasions only. The patient is independent for most activities of daily living, but his daughter helps with shopping and finances. Temperature is 38 C (100.4 F), blood pressure is 122/78 mm Hg, pulse is 98/min, and respirations are 20/min. The patient is alert and oriented but appears frail. There are right-sided crackles and rhonchi. Heart sounds are normal. The abdomen is soft and nontender. There is mild generalized weakness but no focal neurologic deficits. Leukocyte count is 14,200/mm3; chest imaging findings are shown in the exhibit. Sputum and blood samples are obtained for culture, and empiric antibiotics are initiated. Which of the following additional interventions is most appropriate in this patient’s management?
 CorrectIncorrect
CorrectIncorrect -
Question 23 of 33
23. Question
A 55-year-old man with a history of hypertension and obesity is evaluated in the recovery room for hypoxemia after undergoing a sleeve gastrectomy several hours ago. Although the endotracheal intubation was difficult, the procedure was completed without intraoperative complications. The patient was then extubated and transferred to the postanesthesia recovery unit. He was initially stable on ambient air but soon became hypoxemic. Despite the use of oxygen by nasal cannula, his condition has not improved. Other issues include gastroesophageal reflux and generalized anxiety disorder. The patient’s medications include omeprazole, paroxetine, chlorthalidone, and lisinopril. He drinks 3 or 4 beers on most days but does not use tobacco or illicit drugs. His last alcoholic drink was the night prior to surgery. The patient’s preoperative testing was significant only for a mildly elevated serum bicarbonate at 30 mEq/L. Temperature is 37.2 C (99 F), blood pressure is 140/80 mm Hg, pulse is 108/min, and respirations are 12/min. The patient’s pulse oximetry shows 84% on room air. BMI is 39 kg/m2. Examination shows an obtunded patient who is minimally responsive to stimuli. Physical findings include 3-mm reactive pupils, moist mucous membranes, normal jugular venous pressure, coarse breath sounds over the lung fields without stridor or wheezing, and normal S1 and S2. The abdomen is soft and nontender. Examination shows no edema. Laboratory results are as follows:
Arterial blood gas
pH
7.20
PaO2
52 mm Hg
PaCO2
70 mm Hg
ECG shows sinus tachycardia, and chest x-ray reveals bibasilar atelectasis. Which of the following is the most likely cause of this patient’s clinical deterioration?
CorrectIncorrect -
Question 24 of 33
24. Question
A 55-year-old man is brought to the emergency department after a motor vehicle collision. Due to severe, blunt trauma to the chest and abdomen the patient develops acute respiratory distress syndrome and requires intubation with mechanical ventilation. He receives enteral tube feeding for several days, but has high gastric residuals due to ileus. On hospital day 8, total parenteral nutrition is initiated. Temperature is 36.5 C (97.7 F), blood pressure is 110/60 mm Hg, pulse is 85/min, and respirations are 16/min. Physical examination shows moist mucous membranes and normal jugular venous pressure. Breath sounds are coarse bilaterally and heart sounds are normal. Multiple scattered ecchymoses are present on the chest and abdomen. There is mild pedal edema in the bilateral lower extremities. Laboratory results are as follows:
Complete blood count
Hemoglobin
11.2 g/dL
Platelets
200,000/mm3
Leukocytes
4,100/mm3
Serum chemistry
Sodium
134 mEq/L
Potassium
3.6 mEq/L
Creatinine
1.2 mg/dL
Calcium
9.6 mg/dL
Glucose
97 mg/dL
Liver function studies
Albumin
3.7 g/dL
To prevent further complications, which of the following laboratory tests should be monitored closely both before and after initiation of total parenteral nutrition?
CorrectIncorrect -
Question 25 of 33
25. Question
A 34-year-old man comes to the emergency department due to 3 weeks of nonproductive cough, increasing shortness of breath, subjective fevers, night sweats, and intermittent right-sided, sharp chest pain. Two weeks ago, the patient was diagnosed with community-acquired pneumonia at an urgent care clinic and received a week of oral antibiotics without symptomatic improvement. He has no other medical problems and takes no medications. The patient has a history of injection drug use and was recently incarcerated. Temperature is 37.7 C (99.8 F), blood pressure is 120/70 mm Hg, and pulse is 88/min. Chest examination reveals decreased breath sounds and dullness to percussion in the right lower chest. Heart sounds are normal and without murmurs. The abdomen is soft and non-tender with no hepatosplenomegaly. He has no skin rash or enlarged lymph nodes. Chest imaging reveals a right lower lobe pulmonary infiltrate and moderate-sized pleural effusion. A thoracentesis is performed; the pleural fluid is lymphocyte predominant and exudative with an elevated adenosine deaminase level. No organisms are seen on smear. Rapid HIV testing is positive. Which of the following is the best next step in management of this patient’s pleural effusion?
CorrectIncorrect -
Question 26 of 33
26. Question
A 78-year-old woman is brought to the emergency department for evaluation of sudden-onset shortness of breath. Medical history includes hypertension, hypothyroidism, and chronic obstructive pulmonary disease. Initial work-up reveals large, bilateral, segmental pulmonary emboli. Lower-extremity venous compression ultrasonography reveals a large thrombus in the left deep femoral vein. Rivaroxaban is started, and the patient is admitted to the hospital. On the third hospital day, the patient experiences 4 bouts of large-volume, maroon hematochezia. Temperature is 36.7 C (98 F), blood pressure is 98/54 mm Hg, pulse is 110/min, and respirations are 26/min. Pulse oximetry shows 93% on 2 L/min of supplemental oxygen. Hemoglobin level is 8.9 g/dL compared with 12.6 g/dL on admission. Platelet count is 320,000/mm3. The patient’s hemodynamic status is stabilized with intravenous fluids without the need for red blood cell transfusions. Anticoagulation is temporarily held, and the patient has no further episodes of bleeding. Upper gastrointestinal endoscopy and colonoscopy reveal no abnormalities. Video capsule endoscopy demonstrates multiple angiodysplasias in the jejunum and ileum, which are unamenable to endoscopic treatment. Which of the following is the most appropriate next step in management of the patient’s venous thromboembolic disease?
CorrectIncorrect -
Question 27 of 33
27. Question
A 67-year-old woman is evaluated in the intensive care unit for neck swelling. An hour ago, the patient was admitted to the ICU for treatment of pyelonephritis complicated by septic shock and disseminated intravascular coagulation. A central line catheter was placed in the right internal jugular vein. The insertion was difficult, requiring multiple attempts. X-ray after placement revealed the catheter to be in a good position. Over the past 30 minutes, she has developed swelling at the site of the catheter and a feeling of tightness in her neck. She also feels her voice is changing. On examination, there is ballotable swelling under the site of the catheter with surrounding ecchymosis, and the trachea is deviating to the left. The voice sounds hoarse. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 28 of 33
28. Question
A 32-year-old woman comes to the office for a preemployment examination. The patient has had mild shortness of breath on exertion over the past year, which she attributes to deconditioning. Three months ago, an ophthalmologist treated her for anterior uveitis. The patient has no other medical conditions and takes no medications. She does not use tobacco, alcohol, or recreational drugs. Blood pressure is 110/70, pulse is 72/min, and respirations are 14/min. On physical examination, visual acuity is within normal limits. There is swelling of the parotid glands and the lungs are clear to auscultation. Chest x-ray reveals enlarged hilar lymph nodes and nodular pulmonary infiltrates. Which of the following histopathological findings are most likely to be seen on lymph node biopsy in this patient?
CorrectIncorrect -
Question 29 of 33
29. Question
An 83-year-old woman is brought to the emergency department due to several hours of confusion and lethargy. The patient resides in an assisted living facility, and her oral intake has been poor over the preceding 2 days. She has a history of hypertension, type 2 diabetes mellitus, chronic kidney disease, and coronary atherosclerosis. Two months ago, the patient had a non–ST-segment elevation myocardial infarction and underwent percutaneous coronary intervention. She has been taking her medications without issue, but her long-acting insulin was held last night. Temperature is 34.5 C (94.1 F), blood pressure is 85/41 mm Hg, pulse is 108/min, and respirations are 28/min. Pulse oximetry is 93% on room air. The patient is unable to answer questions or follow commands. Cardiovascular examination is normal, and the lungs are clear on auscultation. The extremities are without edema. The skin is cool. Fingertip capillary refill is sluggish. Cardiac telemetry demonstrates normal sinus rhythm with minor T-wave abnormalities. Laboratory results are as follows:
Complete blood count
Hemoglobin
10.4 g/dL
Platelets
120,000/mm3
Leukocytes
17,900/mm3
Serum chemistry
Sodium
129 mEq/L
Blood urea nitrogen
50 mg/dL
Creatinine
2.2 mg/dL
Glucose
58 mg/dL
Urinalysis
Leukocyte esterase
negative
Nitrites
negative
Bacteria
none
White blood cells
1/hpf
Intravenous administration of which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 30 of 33
30. Question
A 58-year-old man is evaluated for an 18-month history of cough. The patient reports daily cough productive of approximately 100 mL of tenacious, brownish sputum. Six months ago, he experienced worsening of the cough with increased sputum volume, malodor, and purulence. The patient was treated with a protracted course of oral antibiotics due to delayed improvement. He had a recurrent episode 3 months ago that similarly required extended antibiotic treatment. The patient reports no new symptoms. Medical history is significant for hypertension and hypothyroidism. He smoked a half-pack of cigarettes daily for 30 years and quit 5 years ago. The patient lives with his healthy adult children and has no pets. Vital signs are within normal limits. Oxygen saturation is 95% on room air. Lung auscultation reveals coarse rhonchi in the left upper thorax. Chest imaging shows left upper lobe bronchial wall thickening and airway dilation without infiltrate or consolidation. The remaining areas of the lungs appear normal. Which of the following is most likely to reveal the underlying cause of this patient’s current condition?
CorrectIncorrect -
Question 31 of 33
31. Question
A 26-year-old man with a 5-year history of asthma comes to the office for follow-up after a recent hospital discharge. The patient was admitted due to fever, shortness of breath, trace hemoptysis, and productive cough with brownish mucus; he was treated with oral glucocorticoids, antibiotics, and nebulized bronchodilators. There were 2 similar episodes in the past year which were treated in the emergency department with tapering oral glucocorticoids on each occasion. He has a history of “walking pneumonia.” Current medications include fluticasone/salmeterol, montelukast, and as-needed albuterol. He does not smoke cigarettes. His father was a heavy drinker and died from liver cirrhosis. The patient is not in acute distress. Physical examination shows diffuse wheezing with adequate air entry. A high resolution CT scan shows central bronchiectasis and a right lower lobe infiltrate. Review of prior chest x-rays shows a lingular infiltrate and a left lower lobe infiltrate. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 32 of 33
32. Question
A 32-year-old man is brought to the emergency department after a motor vehicle accident that resulted in severe head injuries. The patient was unresponsive and hypotensive when paramedics arrived at the scene. He was intubated on-site and given aggressive intravenous fluids. Neurologic imaging reveals multiple cortical contusions, brain hemorrhage, and diffuse axonal injury. The patient is admitted to the intensive care unit. Three days later, he continues to require mechanical ventilation. Temperature is 36.7 C (98 F), blood pressure is 100/45 mm Hg, and pulse is 62/min. Sedation is held, and the patient is examined. There is no response to stimuli of any type. Brainstem reflexes are absent. The ventilator is temporally disconnected to assess for spontaneous respiration. No spontaneous breathing movements are visualized, and arterial blood gas results after 10 minutes are consistent with a positive apnea test, confirming brainstem failure. The patient is declared brain-dead. His wife informs the medical team that the patient always wanted to donate his organs in the event of unexpected death. Which of the following is an important component of care to maximize the viability of this patient’s organs for donation?
CorrectIncorrect -
Question 33 of 33
33. Question
A 25-year-old man with cystic fibrosis comes to the clinic for a routine follow-up appointment. The patient has had multiple hospital admissions over the last few years for pulmonary exacerbations. Pulmonary function testing today will most likely reveal which of the following results?
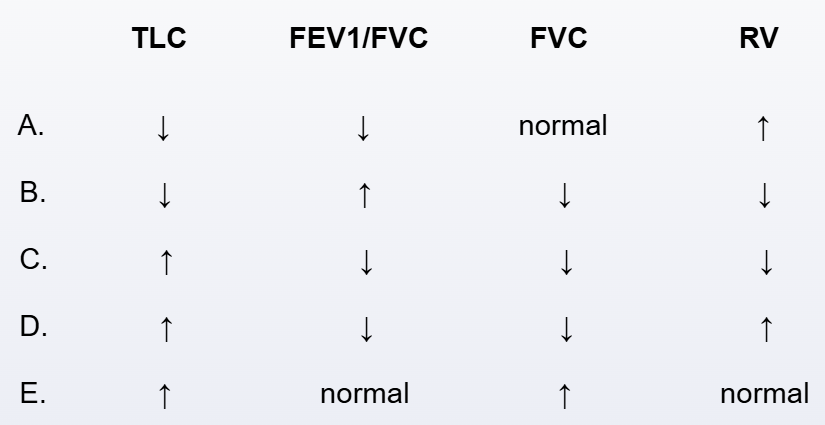 CorrectIncorrect
CorrectIncorrect
