Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 64-year-old man with heart failure comes to the office for follow-up. The patient has shortness of breath on exertion, increasing fatigue, and can barely climb a flight of stairs without stopping to catch his breath. He has no chest pain, cough, or palpitations. Six years ago, the patient had a myocardial infarction, and 3 years ago, he had a cardiac catheterization with stent placement following an episode of chest pain. His other medical problems include hypertension, hyperlipidemia, and type 2 diabetes mellitus. The patient’s medications include carvedilol, sacubitril-valsartan, aspirin, furosemide, atorvastatin, dapagliflozin, and spironolactone. He does not use tobacco, alcohol, or illicit drugs. Blood pressure is 131/78 mm Hg, and pulse is 76/min and regular. Physical examination shows scattered bibasilar crackles on chest auscultation and trace peripheral edema. Laboratory results are as follows:
Sodium
135 mEq/L
Potassium
3.9 mEq/L
Blood urea nitrogen
25 mg/dL
Creatinine
1.3 mg/dL
A recent echocardiogram showed left ventricular dilation with inferior wall hypokinesis, mild left ventricular hypertrophy, and left ventricular ejection fraction of 25%. His ECG is shown here. Which of the following interventions is most likely to improve this patient’s survival?
CorrectIncorrect -
Question 2 of 40
2. Question
A 37-year-old man comes to the office with a several month history of decreased sexual performance. He feels well otherwise, except for mild weakness and occasional headaches. He has no significant past medical history. He does not smoke, but drinks two to three bottles of beer on the weekends. He does not use any illicit drugs. His father died of colon cancer at age 62. Blood pressure is 132/78 mm Hg and pulse is 67/min. On physical examination, both testes are small. There is visual loss in the right temporal visual field. Laboratory testing reveals a prolactin level of 3,200 ng/mL and normal TSH, morning serum cortisol, and insulin-like growth factor levels. Possible diagnoses are explained to the patient. Which of the following best addresses this patient’s concerns?
CorrectIncorrect -
Question 3 of 40
3. Question
A 37-year-old male comes to the emergency department with a two-day history of right leg swelling and discomfort. He denies any provoking event such as trauma, recent surgery, or recent travel. He denies fevers, chills, shortness of breath, cough, syncope, or palpitations. He has no significant past medical history and takes no medications except ibuprofen for occasional headaches. He exercises three times per week. He denies using any illegal drugs including steroids. He does not smoke, but drinks beer on the weekends. His mother suffers from diabetes mellitus and his paternal uncle died suddenly at age 41 of unknown causes. On physical examination today, the patient’s blood pressure is 131/78 mmHg and heart rate is 92/min. His heart sounds are normal, without murmurs or additional sounds. The lungs are clear to auscultation. There is pitting edema of the right lower extremity up to the knee without erythema or warmth. On ultrasound examination of the right lower extremity, the right femoral vein is non-compressible. Which of the following is most likely to be found on genetic work-up of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
A 64-year-old man is brought to the emergency department after his daughter found him confused and lethargic at home. She reports that there were several open medication bottles in his bathroom. The patient has a known history of depression but has never admitted to suicidal ideation. He was recently treated for postherpetic neuralgia. He has no history of heart disease. On physical examination, the patient is lethargic and responds only to strong vocal stimuli. Blood pressure is 78/60 mm Hg and heart rate is 76/min. His pupils are dilated but reactive to light. Mucous membranes are dry and the neck is supple. Deep tendon reflexes are symmetric and the plantar responses are flexor. ECG shows a normal sinus rhythm with QRS prolongation to 130 msec. Which of the following is most likely to narrow the QRS interval in this patient?
CorrectIncorrect -
Question 5 of 40
5. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 36-year-old woman comes to the office to discuss weight gain. During her pregnancy 6 years ago, she gained a significant amount of weight that she found difficult to lose; since then, she has slowly gained additional weight. She has no polyuria/polydipsia, visual disturbances, fatigue, or heat/cold intolerance. The patient has no significant medical history and takes no medications. She uses an intrauterine contraception device. The patient consumes fast foods 2 or 3 times a week. She does not use tobacco, alcohol, or recreational drugs. Family history is significant for myocardial infarction in her father. Blood pressure is 129/78 mm Hg and pulse is 76/min. Waist circumference is 88 cm (35 in), and neck circumference is 38 cm (15 in). BMI is 29 kg/m2. Examination shows scattered, pale stretch marks across the upper and lower abdomen. The remainder of the physical examination, including cardiopulmonary, thyroid, abdominal, and neurologic, is unremarkable.
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
Item 2 of 2
Initial test results are normal. Following patient-centered lifestyle counseling, the patient begins a calorie-restricted, low-carbohydrate diet and an appropriate exercise regimen. She returns to the office in 6 months for follow-up; although she has made some lifestyle changes, she has found it difficult to adhere strictly to the regimen and has lost no weight. The patient has experienced intermittent back pain but otherwise feels well. BMI is now 31 kg/m2. The patient requests more aggressive weight loss intervention. In addition to continuing lifestyle counseling, which of the following is most appropriate?
CorrectIncorrect -
Question 7 of 40
7. Question
A 35-year-old man returns to the office for his third visit in 6 months because he is convinced that he is infected with parasites. He has gained 1.4 kg (3 lb) since his last visit 2 months ago and believes that his abdomen is distended due to growing parasites. He reports occasional nausea and an episode of diarrhea. The patient believes he became infected with a tapeworm while eating undercooked meat on a business trip to Asia 6 years ago. Since then, he has seen multiple physicians for this same concern, with no evidence of parasitic infection. He has had several negative stool examinations that he claims are false. The patient checks his stool after each bowel movement and spends hours on the Internet researching parasitic diseases. He has no significant medical history. Current medications include a multivitamin and acetaminophen as needed. He drinks alcohol socially and does not use tobacco or illicit drugs. Temperature is 36.5 C (97.7 F), blood pressure is 121/78 mm Hg, and pulse is 62/min. The abdomen is soft, nontender, and nondistended with normal bowel sounds. The remainder of the physical examination is unremarkable. The patient’s mood is anxious and his affect is tense. He has no auditory hallucinations but describes a sensation of parasites crawling under his skin. He insists on being tested again for parasites. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 8 of 40
8. Question
A 5-year-old boy is brought to the emergency department for bloody diarrhea. Yesterday morning, he had loose, watery bowel movements and non-bilious emesis, but his stool became grossly bloody as the day progressed. He has had 2 loose, bloody bowel movements this morning as well as abdominal pain but has been afebrile. The patient has been urinating normally and has had no blood in his urine. He went on a class trip to a local petting zoo one week ago. The patient and his family went on a vacation cruise 2 weeks ago. There is no significant past medical history and immunizations are up to date. The boy’s parents and 4-year-old brother are currently well. Temperature is 36.6 C (97.8 F), blood pressure is 110/60 mm Hg, and heart rate is 100/min. Examination shows a tired-appearing boy with chapped lips and dry oral mucosa. The abdomen is not distended but bowel sounds are hyperactive. There is generalized abdominal tenderness without guarding or rebound. Rectal examination reveals normal tone, no fissures, and no lesions; blood mixed with stool is present in the rectal vault. No petechial rashes are seen. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 9 of 40
9. Question
A 32-year-old man comes to the physician with groin discomfort on his right side. Two weeks ago, he discovered a lump in his right groin that “comes and goes” and soon after was diagnosed with an inguinal hernia at an urgent care clinic. The patient’s past medical history is significant for psoriasis treated with topical agents. He does not take oral medications or illicit drugs. The patient drinks 2–3 beers daily and smokes a pack of cigarettes each day. As a construction worker, he regularly lifts objects up to 30 lb (13.6 kg). The patient’s mother died of ovarian cancer, and his father was recently diagnosed with prostate cancer. Blood pressure is 128/81 mm Hg and pulse is 87/min. Body mass index is 22.5 kg/m2. Physical examination is significant for scaly patches on his back and both knees. A reducible hernia is palpated in the right groin. Laboratory results are as follows:
White blood cells
4,800/µL
Hemoglobin
11.5 g/dL
Mean corpuscular volume
69 fL
Platelets
175,000/µL
Creatinine
1.1 mg/dL
Serum iron
90 µg/dL
Iron transferrin saturation
35%
Red blood cell distribution width is normal. Which of the following is the best next step in evaluation of this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
A 24-year-old woman, gravida 1 para 0, comes to the office for an initial prenatal visit. She has no cramping or vaginal bleeding. This was an unplanned pregnancy. The patient started combination oral contraceptive pills 2 years ago, when she began methotrexate and hydroxychloroquine therapy for rheumatoid arthritis. Since then, she has had irregular menses that occur every 1-2 months and consist of 2-3 days of spotting. Several months ago, while visiting family abroad, the patient ran out of and skipped several days of her contraceptive pills. She resumed taking her oral contraceptives after her return. However, she became concerned when she did not have a menstrual period for several months and took a home pregnancy test. The patient has no other chronic medical conditions and has had no prior surgeries. She started taking a folate supplement and prenatal vitamin when she found out she was pregnant. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 100/70 mm Hg. BMI is 24 kg/m2. Pelvic examination reveals a 15-week-sized uterus with no adnexal masses or tenderness. Initial laboratory results include the following:
Complete blood count
Hemoglobin
11.2 g/dL
Platelets
240,000/mm3
Immunologic and rheumatologic studies
Hepatitis panel
Hepatitis B surface antigen
negative
HIV screening
HIV-1 antibody
negative
Rapid plasma reagin
nonreactive
Maternal serum quadruple screen
Estradiol
normal
Quantitative β-hCG
normal
Inhibin A
normal
Alpha-fetoprotein, serum
elevated
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 46-year-old male undergoes a cadaveric kidney transplant for rapidly progressive glomerulonephritis. His past medical history is significant for hepatitis C, hypertension, and type 2 diabetes mellitus. The surgery is uncomplicated, and when he is discharged, his BUN is 12 mg/dL and creatinine is 1.2 mg/dL. His immunosuppression regimen includes cyclosporine, mycophenolate, and low-dose prednisone. Five weeks after the procedure, he complains of malaise. His BUN is 28 mg/dL and creatinine is 2.1 mg/dL. A renal allograft biopsy shows evidence of renal tubular damage with prominent basophilic intranuclear inclusions. Which of the following is the most likely cause of his decreased renal function?
CorrectIncorrect -
Question 12 of 40
12. Question
A multiyear, federal, cross-sectional analysis is conducted evaluating trends in per capita spending on health care services among various segments of the US population. The results indicate that per capita spending has increased each year and is significantly higher compared to that in other countries. Further analysis indicates that one segment of the population consistently incurs disproportionately higher spending, as seen in the shaded area on the graph below.
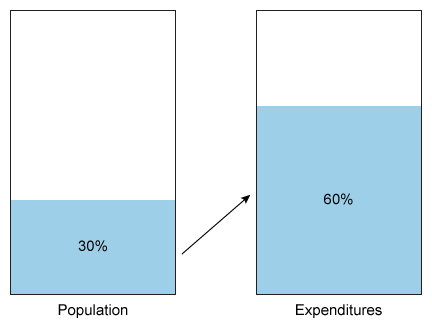
Which of the following is likely to be most commonly found in the shaded population?
CorrectIncorrect -
Question 13 of 40
13. Question
A 36-year-old woman, gravida 2 para 1, at 39 weeks gestation comes to the office for a routine prenatal visit. The patient has had no vaginal bleeding, leakage of fluid, or contractions. Fetal movement is normal. She has type 2 diabetes mellitus that has been controlled with an insulin regimen during this pregnancy. Her prior pregnancy resulted in an uncomplicated spontaneous vaginal delivery of a 4.1-kg (9-lb) infant. In addition to insulin, the patient takes a prenatal vitamin daily. She does not use tobacco, alcohol, or illicit drugs. Blood pressure is 124/76 mm Hg and pulse is 88/min. BMI is 28 kg/m2. Fundal height is 42 cm. Cervical examination shows the cervix to be 3 cm dilated and 50% effaced and the fetal head at −3 station. An ultrasound performed today reveals a vertex presentation, an estimated fetal weight of 5.1 kg (11.2 lb), and a normal biophysical profile. The patient’s last hemoglobin A1c was 7.2%. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 62-year-old woman comes to the office due to a 2-month history of muscle weakness. She has a feeling of heaviness in her legs and has had moderate to severe muscle pain after walking. She also reports, “My hands feel clumsy, and sometimes I need help turning door knobs and opening jars.” On most days the patient goes to sleep at 9 PM and wakes up at 8 AM, but her sleep is disrupted several times a night due to a “pins and needles” sensation in both hands. She has been ”feeling down” recently and has a history of depression treated with fluoxetine. The patient has had no cough, chest pain, abdominal pain, diarrhea, diplopia, or urinary symptoms. Medical history is also notable for hypertension, for which she takes hydrochlorothiazide. She was also recently diagnosed with hyperlipidemia but is not on lipid-lowering therapy as she wants to “control it with my diet.” The patient smoked a pack of cigarettes a day for 30 years but quit 4 years ago. She drinks a glass of wine occasionally on weekends. Blood pressure is 150/83 mm Hg and pulse is 62/min. BMI is 31 kg/m2. There is no muscle tenderness, joint deformities, or skin lesions. Laboratory results are as follows:
Complete blood count
Hemoglobin
10.2 g/dL
Mean corpuscular volume
86 μm3
Leukocytes
6,000/mm3
Platelets
180,000/mm3
Serum chemistry
Sodium
132 mEq/L
Potassium
4.5 mEq/L
Creatinine
1.4 mg/dL
Calcium
8.8 mg/dL
Glucose
70 mg/dL
Aspartate aminotransferase (SGOT)
62 U/L
Alanine aminotransferase (SGPT)
24 U/L
Creatine kinase
1,200 U/L
Additional testing is most likely to find which of the following in this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 23-year-old woman comes to the office due to frequent headaches. She has had sporadic episodes since age 16 and now has similar headaches 5 or 6 times a month. The headaches are often preceded by a “funny feeling” in her stomach. The pain is severe, one-sided, and throbbing and associated with nausea and vomiting. Acetaminophen and resting in a dark, quiet room help relieve the pain. The headaches typically resolve within 12 hours, but the patient has gone to the emergency department for treatment twice in the past 3 months. She is otherwise healthy and does not use tobacco, alcohol, or recreational drugs. Her mother also has frequent headaches. Blood pressure is 130/78 mm Hg and pulse is 82/min. There is no muscle weakness or sensory loss, the visual fields are fully intact, and no cerebellar signs are present. Which of the following preventive medications is most likely to be effective in reducing the frequency of this patient’s headaches?
CorrectIncorrect -
Question 16 of 40
16. Question
A 42-year-old man is evaluated for acute shortness of breath during hospitalization. The patient was admitted yesterday due to severe abdominal pain, nausea, and vomiting after alcohol binge drinking. Evaluation revealed epigastric tenderness, leukocytosis, and elevated serum amylase and lipase levels. The patient was treated with intravenous fluids, analgesics, and antiemetics. Today, he began to experience progressive shortness of breath. Temperature is 37.2 C (99 F), blood pressure is 120/78 mm Hg, pulse is 118/min, and respirations are 24/min. The patient’s pulse oximetry shows 84% while breathing ambient air and 89% with 4 L/min oxygen via nasal cannula. He is using accessory muscles of respiration. Neck veins are flat. Lung auscultation reveals bilateral diffuse crackles. Chest radiography reveals bilateral interstitial infiltrates that were not present at time of admission. Endotracheal intubation is performed for mechanical ventilation. Which of the following ventilator settings is most likely to improve mortality in this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
A 63-year-old man is evaluated for occasional right upper quadrant pain that develops after he eats fatty meals. The pain is accompanied by nausea and bloating. Medical history is significant for coronary artery disease, hypertension, hyperlipidemia, and type 2 diabetes mellitus. The patient underwent coronary artery bypass surgery 6 years ago and a right-sided carotid endarterectomy for asymptomatic, high-grade carotid artery stenosis 10 years ago. He smokes a pack of cigarettes daily and drinks alcohol occasionally. He was offered insulin therapy several months ago due to suboptimal blood glucose control but refused. Abdominal ultrasonography reveals a few small gallstones as well as a 3.5-cm infrarenal abdominal aortic aneurysm. Which of the following statements by the physician best addresses the latter sonographic finding?
CorrectIncorrect -
Question 18 of 40
18. Question
A 36-year-old man comes to the office due to an itchy rash on his arms. He has never had a rash like this before. He denies any skin cream use or recent changes in soap or laundry detergent. He has not had any recent travel. His past medical history is significant for hypertension and kidney stones. Current medications include amlodipine, which he has been taking for 6 months. The examination findings are shown in the picture below.

Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 19 of 40
19. Question
A 75-year-old woman is brought to the hospital from a nursing facility due to progressive shortness of breath, productive cough, and lethargy. Medical history is significant for hypertension, hyperlipidemia, ischemic stroke with residual left-sided hemiparesis, and moderate dementia. Temperature is 38.3 C (101 F), blood pressure is 120/70 mm Hg, pulse is 110/min, and respirations are 32/min. Pulse oximetry shows 84% on ambient air. Predicted body weight is 60 kg (132 lb). The patient appears to be in respiratory distress and is using accessory muscles of respiration. Mucous membranes are dry. Lung auscultation reveals coarse crackles and rhonchi over the right lower lobe. The patient is not alert enough for noninvasive ventilation, and rapid sequence induction followed by endotracheal intubation is performed. Breath sounds are auscultated bilaterally, and capnography shows a normal-appearing waveform. She is placed on a mechanical ventilator on assist-control mode with the following settings: Respiratory rate of 12/min, tidal volume of 480 mL, fraction of inspired oxygen of 100%, and positive end-expiratory pressure of 5 cm H2O. Immediately after the mechanical ventilation is initiated, the patient’s blood pressure drops to 70/50 mm Hg, with a pulse of 120/min and an oxygen saturation of 95%. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 63-year-old man comes to the office due to leg swelling that started 2 weeks ago. He had a respiratory infection 2 months ago that was treated with antibiotics. The patient has had no rash, joint pain, fever, cough, abdominal pain, or diarrhea. Medical history is significant for hypertension, for which he takes lisinopril and chlorthalidone. He has not been taking any nonsteroidal anti-inflammatory medications. The patient does not use tobacco, alcohol, or recreational drugs. Blood pressure is 135/70 mm Hg and pulse is 95/min. There is 2+ symmetric pitting edema of both lower extremities. Physical examination is otherwise unremarkable. Laboratory findings are as follows:
Hemoglobin
12.5 mg/dL
Leukocytes
7,200/mm3
Platelets
210,000/mm3
Sodium
139 mEq/L
Potassium
4.1 mEq/L
Chloride
104 mEq/L
Bicarbonate
25 mg/dL
Blood urea nitrogen
24 mg/dL
Creatinine
1.1 mg/dL
Glucose
95 mg/dL
Total bilirubin
0.8 mg/dL
AST
23 U/L
ALT
28 U/L
Alkaline phosphatase
98 U/L
Albumin
2.0 g/dL
Urinalysis is significant for 4+ protein. A 24-hour urine collection shows protein excretion of 11.5 g/day. The risk for which of the following is most likely to be significantly increased in this patient?
CorrectIncorrect -
Question 21 of 40
21. Question
A 27-year-old woman, gravida 2 para 1, at 26 weeks gestation comes to the office for evaluation of a fever. She has had a fever and joint pain for several days and is now starting to notice a faint, diffuse rash. The patient has felt minimal fetal movement during this time. Her 5-year-old son was recently ill with a similar fever and body rash, and he also had facial redness. He is now feeling well. The patient has no chronic medical conditions or previous surgeries. She takes a daily prenatal vitamin and is allergic to penicillin. She does not use tobacco, alcohol, or illicit drugs. Temperature is 37.8 C (100 F), blood pressure is 110/70 mm Hg, and pulse is 96/min. The fetal heart rate is 160/min by bedside Doppler. A diffuse erythematous rash is visible on the patient’s skin. The lungs are clear to auscultation and heart sounds are normal. The abdomen is soft and nontender, and fundal height is 26 cm. A review of the patient’s blood work from her first prenatal visit shows that she is immune to rubella. HIV and syphilis screening were negative. She asks how this infection will affect her pregnancy. Which of the following is the best counseling for this patient?
CorrectIncorrect -
Question 22 of 40
22. Question
A 45-year-old man comes to the office due to persistent weakness and fatigue for the past year. He also reports poor concentration and decreased sex drive. The patient has no history of serious illness and takes no medications. He does not use tobacco or illicit drugs and drinks alcohol occasionally. The patient works as a hospital phlebotomist and lives alone after a recent divorce. His father died from complications of cirrhosis. Temperature is 37 C (98.6 F), blood pressure is 126/70 mm Hg, and pulse is 80/min. BMI is 34 kg/m2. Cardiopulmonary examination is normal. The abdomen is nondistended, soft, and nontender with no hepatosplenomegaly. Laboratory results are as follows:
Complete blood count
Hemoglobin
14.6 g/dL
Platelets
360,000/mm3
Leukocytes
8,800/mm3
Serum chemistry
Blood urea nitrogen
14 mg/dL
Creatinine
0.9 mg/dL
Glucose
140 mg/dL
Liver function studies
Total bilirubin
1.0 mg/dL
Alkaline phosphatase
68 U/L
Aspartate aminotransferase
62 U/L
Alanine aminotransferase
74 U/L
25-hydroxyvitamin D
40 ng/mL (15-80 ng/mL)
Vitamin B12, serum
380 pg/mL
Ferritin, serum
650 ng/mL (15-200 ng/mL)
Transferrin saturation
70%
Erythrocyte sedimentation rate
10 mm/h (0-15 mm/h)
TSH
3.8 µU/mL (0.5-5.0 µU/mL)
Hepatitis B surface antibody
positive
Hepatitis B surface antigen
negative
Hepatitis C virus antibody
negative
HIV antibody
negative
Testosterone, total, serum
250 ng/dL (240-950 ng/dL)
Which of the following is the best next step in evaluation of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 19-year-old man comes to the office due to severe heartburn. The patient states that 3 days ago he awoke at night with a burning sensation in his chest and stomach. Since then, the pain has been constant, and eating or drinking makes it worse. He has never had similar symptoms before. The patient has had no fever, nausea, vomiting, hematemesis, hematochezia, or melena. He has taken over-the-counter antacids but with no significant symptom relief. He has a history of eczema during childhood and a 2-year history of severe acne. The patient reports significant improvement in his acne since oral doxycycline was initiated 3 months ago and takes his medications regularly at bedtime. He does not use tobacco, alcohol, or illicit drugs. Family history is notable for scleroderma in his mother. Temperature is 36.6 C (97.9 F), blood pressure is 116/70 mm Hg, and pulse is 78/min. BMI is 28 kg/m2. Oropharyngeal mucosa appears normal with no erythema or lesions. Cardiopulmonary examination is normal. The abdomen is nondistended, soft, and nontender. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
A 67-year-old man comes to the emergency department due to 2 days of progressive shortness of breath and cough productive of white sputum. The patient reports no fever, chills, hemoptysis, palpitations, or syncope. His medical history is significant for chronic obstructive pulmonary disease with a recent FEV1 that was 68% of the predicted value. The patient uses 2 L of supplemental oxygen at home via nasal cannula. His current medications include a combination fluticasone and salmeterol inhaler, a tiotropium inhaler, and an albuterol inhaler as needed. The patient no longer smokes but has a 50-pack-year history. Temperature is 37.2 C (99 F), blood pressure is 165/95 mm Hg, and pulse is 116/min and regular. His respiratory rate is 28/min, and oxygen saturation is 89% on 2 L oxygen via nasal cannula. On examination, the patient is in moderate respiratory distress and using accessory muscle of respiration. He is alert and cooperative. Breath sounds are decreased bilaterally with diffuse wheezing and prolonged expirations. Heart sounds are distant. The abdomen is soft and nontender. There is no peripheral edema. A chest x-ray reveals hyperinflated lung fields without infiltrates. The initial arterial blood gas on 2 L nasal cannula oxygen shows the following:
pH
7.27
pCO2
65 mm Hg
pO2
62 mm Hg
In addition to systemic corticosteroids, antibiotics, and nebulized bronchodilators, which of the following is the best initial treatment for this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 63-year-old man with a history of coronary artery disease comes to the emergency department due to 2 episodes of chest pain. The first episode occurred 12 hours ago while the patient was doing laundry and consisted of retrosternal discomfort. The second episode occurred 2 hours ago while he was watching television and consisted of retrosternal pressure and mild shortness of breath lasting 20 minutes. Medical history is significant for coronary artery bypass surgery 6 years ago and type 2 diabetes mellitus. The patient last saw his cardiologist a year ago, at which time nuclear stress testing showed no evidence of ischemia. Current medications include metoprolol, atorvastatin, and low-dose aspirin. Blood pressure is 132/85 mm Hg and pulse is 63/min. The lungs are clear to auscultation, and there is no peripheral edema. ECG shows 1-mm ST-segment depressions in leads V5 and V6. Initial laboratory test results reveal an elevated troponin level. Clopidogrel and enoxaparin are administered, and the patient is admitted to the hospital. Following initial stabilization, this patient would benefit most from which of the following additional medications?
CorrectIncorrect -
Question 26 of 40
26. Question
A 60-year-old man comes to the office with right-sided headache, visual changes in his right eye, and mild fatigue. He has no other symptoms. Medical history is significant for hypertension and bipolar disorder that has been stable for years. He takes atenolol and lamotrigine at home. The patient has no drug allergies. He is a nonsmoker but drinks alcohol infrequently on weekends. Temperature is 37.8 C (100 F), blood pressure is 129/81 mm Hg, pulse is 86/min, and respirations are 14/min. Physical examination shows right-sided temporal tenderness. The physician strongly suspects giant cell (temporal) arteritis, refers him for a temporal artery biopsy, and prescribes prednisone 60 mg/day while awaiting biopsy results. The biopsy subsequently confirms the suspected diagnosis. The patient returns for follow-up after 2 weeks and appears tearful, frustrated, and irritable. He has become increasingly distressed and sad about the diagnosis of temporal arteritis and has isolated himself from friends and family. He is anhedonic. He has not been able to sleep at night due to racing thoughts. Vital signs are normal. On examination, the patient shows mild psychomotor slowness. His thought process is linear and organized. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 27 of 40
27. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 17-year-old girl is brought to the office due to recurrent sore throat. The patient says, “I’m the lead in my school’s musical, and rehearsals are every day after school, so I’ve been singing a lot. I’ve already tried lozenges and tea with honey, but nothing has helped with the pain.” She drinks 2 or 3 beers on the weekends and does not use other recreational substances. The patient is sexually active with her boyfriend and uses condoms. Menstrual cycles are regular. Family history is significant for lung cancer in her father. The patient receives above-average grades in school. Temperature is 37.2 C (99 F), blood pressure is 110/68 mm Hg, and pulse is 88/min. On physical examination, redness of the pharynx without exudates and mild parotid gland swelling are present. The remainder of the physical examination is unremarkable.
Item 1 of 2
This patient’s symptoms require additional history regarding which of the following?
CorrectIncorrect -
Question 28 of 40
28. Question
Item 2 of 2
The patient eats more than she intends to several times a week, consuming large amounts of ice cream, cookies, and chips. She is concerned about gaining weight and shares that she makes herself vomit after eating too much to maintain a stable weight. Complete blood count, basic metabolic panel, and serum electrolyte levels are normal. BMI is 20 kg/m2, at the 15th percentile for age. In addition to cognitive-behavioral therapy, which of the following pharmacologic options is indicated for this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
A 27-year-old woman, gravida 1 para 0, at 11 weeks gestation comes to the emergency department due to 2 days of a yellow, nonmalodorous vaginal discharge. The discharge stains through the patient’s underwear, requiring her to change multiple times a day. She has had no vaginal bleeding or contractions but has had increasing vulvar pruritus. The patient recently had a sinus infection that was treated with a course of antibiotics. She has no chronic medical conditions and has had no surgeries. The patient takes a daily prenatal vitamin and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 128/78 mm Hg and pulse is 86/min. Pelvic examination reveals no cervical motion or adnexal tenderness. On speculum examination, a thick, light yellow discharge is seen coating the vaginal vault. The cervix is closed, and no discharge from the cervical os is present. The pH of the fluid is 4. A bedside ultrasound reveals an 11-week intrauterine gestation with a normal fetal heart rate. The patient asks if there is anything that can treat her symptoms. Which of the following is the most appropriate response to this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 23-year-old woman is brought to the emergency department due to muscle cramps and generalized weakness. She is a nursing assistant, has no medical history, and does not use recreational substances or alcohol. The patient is hesitant when answering questions. Temperature is 36.6 C (97.9 F), blood pressure is 110/70 mm Hg, and pulse is 108/min. The patient is alert but appears anxious. Cardiopulmonary and neurologic examinations are normal. Serum electrolyte results are as follows:
Sodium
130 mEq/L
Potassium
2.7 mEq/L
Chloride
90 mEq/L
Bicarbonate
36 mEq/L
Arterial pH is 7.48. Measurement of which of the following would be most helpful for establishing the cause of this patient’s multiple electrolyte abnormalities?
CorrectIncorrect -
Question 31 of 40
31. Question
An 84-year-old woman is brought to the office by her daughter for a routine health maintenance evaluation. The patient was diagnosed with vascular dementia 2 years ago and had a stroke 6 months ago that left her with minimal residual left-sided weakness. She lives with her daughter, who drives her as needed and handles her finances, shopping, and cooking. The patient requires supervision when she leaves the house because she has gotten lost several times. Until a month ago, the patient could dress and feed herself and use the bathroom without assistance, although she has required help with bathing for the last year. At today’s visit, the daughter shares that her mother has recently required prompting to complete daily activities and meals and has been tearful and anxious much of the time. The patient is frequently restless and gets up several times a night to pace. She is now reluctant to leave the house, stating, “I am so worried something bad will happen.” Several times a day she asks for her husband, who died 10 years ago. The daughter says, “She gets overwhelmed so easily now that I avoid talking about the past and try to change the topic if she asks me something.” Additional medical history includes coronary artery disease and hypertension. Current medications include metoprolol, aspirin, lisinopril, atorvastatin, and donepezil. Vital signs are normal. The patient is alert and oriented to self and place only, which is her baseline. Physical examination shows no abnormalities with the exception of mild left-sided weakness that is unchanged from her last visit. The patient has no suicidal thoughts or hallucinations. Routine laboratory testing, including complete blood count, comprehensive metabolic panel, and urinalysis, are normal. MRI of the brain shows no acute changes. Which of the following is the most appropriate pharmacotherapy?
CorrectIncorrect -
Question 32 of 40
32. Question
A 43-year-old male presents to your office with a painful lesion on his right calf. Initially, he thought it was a spider bite because of a small amount of pain and redness. However, a couple of days later, the lesion got progressively larger. He also notes feeling weak and feverish. He lives in Connecticut and travels to Long Island frequently. He denies any trauma. He has no other medical problems. He does not drink alcohol, smoke tobacco or use any illicit drugs. Today his temperature is 38.1°C (100.5°F), blood pressure is 128/78 mmHg, and heart rate is 92/min. The lesion is shown on the slide below.

Which of the following is the best initial antibiotic choice for this patient?
CorrectIncorrect -
Question 33 of 40
33. Question
A 24-year-old body builder comes to the clinic due to persistent pain in his right elbow. The pain began suddenly 2 days ago, when he was lifting weights at the gym and felt a pop at the elbow. This was followed by bruising and swelling around the elbow and difficulty lifting objects. The patient is otherwise healthy and takes a daily multivitamin and protein supplement. On examination, swelling and ecchymosis are present in the right antecubital fossa. There is no sensory deficit and the radial pulse is strong. Strength with flexion of the right elbow and supination of the right forearm is decreased. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 34 of 40
34. Question
A 4-year-old boy is brought to the emergency department by ambulance after “acting strangely.” The mother states, “He seemed more tired than usual and was resting on the couch. He made some moaning sounds, and then his left arm started writhing and stiffening. He seemed awake the whole time and was looking at me, but he could not reply to anything I was saying.” The episode lasted approximately 10 minutes and ended before emergency personnel arrived. No medications were given. The patient has had several headaches in the last few weeks, often awakening him from sleep. Otherwise, he has no chronic medical conditions and has had no surgeries. Vaccinations are up to date. The patient’s mother takes opioids for chronic back pain. His 2-year-old brother has a history of febrile seizures. Temperature is 37.2 C (99 F). Height and weight are at the 50th and 75th percentiles, respectively. On physical examination, the patient appears tired but is cooperative. Neurologic examination, including funduscopy, is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 35 of 40
35. Question
A group of investigators studied the role of impaired metabolic activation of clopidogrel (CYP2C19 loss-of-function alleles) on clinical outcomes after a percutaneous coronary intervention (PCI). More than 2,000 patients were consented for the genetic study to determine the effect of different allelic variants of the CYP2C19 gene after a PCI for acute coronary syndrome. All of the patients received long-term, low-dose aspirin and clopidogrel following the procedure along with other therapies. One year after the PCI, 225 deaths as well as 94 strokes and non-fatal myocardial infarctions (MI) were observed. Patients with CYP2C19 loss-of-function alleles were 3.6 times more likely to experience the composite end points of death, non-fatal MI, or stroke as compared to patients with the wild-type allele (p <0.05). Which of the following best describes this study design?
CorrectIncorrect -
Question 36 of 40
36. Question
A 64-year-old woman comes to the emergency department due to back pain. For the past week, she has had slowly worsening, nonradiating back pain. She has no history of trauma to that area but has had intermittent fever and chills. The patient has a history of hypertension, type 2 diabetes mellitus, and end-stage renal disease due to diabetic nephropathy. She receives intermittent hemodialysis via a tunneled subclavian catheter, which was placed 2 months ago due to a failed arteriovenous fistula. The patient also underwent mitral valve repair for mitral regurgitation 4 years ago. She does not use tobacco, alcohol, or illicit drugs. Temperature is 38.3 C (101 F), blood pressure is 130/80 mm Hg, pulse is 96/min, and respirations are 18/min. Physical examination shows a normal central venous catheter site, clear lung fields, and no significant heart murmurs. The abdomen is soft and nontender. Spine examination is notable for focal tenderness over the lower thoracic vertebrae. Neurologic examination shows normal motor strength of both lower extremities. Sensation to light touch is decreased over both feet but deep tendon reflexes are normal. Laboratory results are as follows:
Complete blood count
Hemoglobin
10.1 g/dL
Platelets
180,000/mm3
Leukocytes
21,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
4.9 mEq/L
Calcium
8.6 mg/dL
Glucose
140 mg/dL
Erythrocyte sedimentation rate
100 mm/h
C-reactive protein
12.8 mg/L (normal: <8 mg/L)
Spine imaging reveals T12-L1 vertebral body destruction with disk-space narrowing; no epidural or paravertebral fluid collection is present. The patient is hospitalized and intravenous antibiotics are started. Two sets of blood cultures grow gram-positive cocci in clusters <24 hours after being drawn. The central venous catheter is removed by interventional radiology. Which of the following is the most appropriate next test for this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
A 42-year-old man comes to the office because of recurrent nasal discharge. For the past 3 days, he has had profuse bloody nasal discharge associated with sinus pressure, diffuse myalgia, and a dry cough. Medical history includes granulomatosis with polyangiitis, which has caused several episodes of upper respiratory tract symptoms; the patient has been treated with cyclophosphamide for the past 3 years. Temperature is 37.3 C (99.1 F), blood pressure is 136/85 mm Hg, pulse is 76/min, and respirations are 18/min. Examination shows bloody nasal discharge with crusting and multiple painless oral ulcers. The lungs are clear to auscultation and heart sounds are normal. Chest x-ray reveals a few nodules in both lungs but is otherwise clear. This patient’s condition is associated with the greatest risk for which of the following life-threatening complications?
CorrectIncorrect -
Question 38 of 40
38. Question
A 46-year-old man comes to the office due to fatigue for the past 3 months. Symptoms have progressed, and the patient now requires frequent daytime napping. Medical history is significant for ulcerative colitis diagnosed 12 years ago and treated with mesalamine. Surveillance colonoscopy a year ago was normal. The patient has had no fevers, chills, abdominal pain, or dysuria; he has 1 or 2 loose bowel movements per day. Blood pressure is 125/78 mm Hg, and pulse is 81/min. Physical examination is unremarkable. Laboratory results are as follows:
Hemoglobin
11.7 g/dL
Leukocytes
10,700/mm3
Platelets
510,000/mm3
Mean corpuscular volume
75 μm3
Sodium
140 mEq/L
Potassium
3.4 mEq/L
Chloride
104 mEq/L
Bicarbonate
22 mEq/L
Blood urea nitrogen
12 mg/dL
Creatinine
0.6 mg/dL
Glucose
95 mg/dL
Total bilirubin
2.8 mg/dL
Aspartate aminotransferase (SGOT)
49 U/L
Alanine aminotransferase (SGPT)
88 U/L
Alkaline phosphatase
535 U/L
Albumin
4.0 g/dL
INR
1.0
Hepatitis B surface antigen
negative
Anti–hepatitis C antibody
negative
Which of the following tests is most likely to confirm the diagnosis in this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 37-year-old woman, gravida 2 para 1, at 38 weeks gestation comes to the emergency department due to regular, painful uterine contractions and dark vaginal bleeding. The patient reports decreased fetal movement over the last 3 days, but no leakage of fluid. Her pregnancy was complicated by a first-trimester screen that showed an increased risk of trisomy 21. However, a cell-free fetal DNA test and anatomy ultrasound were both normal. The patient’s previous pregnancy was uncomplicated and ended in a term vaginal delivery. She has no medical problems or previous surgeries. She takes a prenatal vitamin daily and does not use tobacco, alcohol, or illicit drugs. Temperature is 36.7 C (98 F), blood pressure is 160/96 mm Hg, and pulse is 84/min. Pelvic examination shows minimal dark bloody discharge, cervical dilation of 3 cm, and the fetal head at 0 station. Tocometer shows contractions every 3 minutes, but the fetal heartbeat is not detected by Doppler sonography. Bedside ultrasound shows no fetal cardiac activity and a blood clot between the placenta and the uterus. Urine dipstick shows 3+ protein. Which of the following is the most appropriate counseling for this patient at this time?
CorrectIncorrect -
Question 40 of 40
40. Question
A 10-year-old boy is brought to the office due to 2 days of itching and redness of both eyes. His parents say, “He can’t stop rubbing his eyes, even though it seems to make the itching worse. Two kids in his class had pink eye 2 weeks ago, and we think he might need to be treated.” The boy has had no visual changes, photophobia, or fever. He has a history of mild intermittent asthma, for which he takes inhaled albuterol as needed. The patient lives at home with his parents, younger sister, and a dog that the family adopted from a shelter last month. Vital signs are within normal limits. Physical examination shows diffuse, bilateral conjunctival injection with thin, clear discharge. Darkening beneath both eyes and mild swelling of the eyelids are present. There are also mild, clear rhinorrhea and pale nasal mucosa. The lungs are clear to auscultation. The remainder of the physical examination is unremarkable. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect
