Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 53-year-old woman comes to the office due to persistent fatigue. The patient says, “I feel so tired for no reason. I could take a nap at my desk every day, and I worry because I’m getting more and more behind at work.” She adds, “I am also very thirsty and can’t go for more than a few hours without needing to urinate.” The patient works as a human resources analyst and is afraid her boss will notice her tired appearance and frequent trips to the bathroom. Medical history is significant for asthma, anxiety, and treatment-resistant depression. Over the last year, she has been hospitalized twice, once for asthma exacerbation and once for depression. The patient smokes a pack of cigarettes a day and drinks alcohol occasionally. She has a history of cocaine abuse but does not use illicit drugs at present. Family history is significant for bipolar disorder in her mother; the patient’s father died of prostate cancer. The patient is not allergic to any medications. Blood pressure is 143/78 mm Hg and pulse is 79/min. BMI is 29 kg/m2. Physical examination is unremarkable. Laboratory evaluation shows a serum creatinine of 1.0 mg/dL and fasting blood glucose of 211 mg/dL. HbA1c is 7.5%. Which of the following medications most likely contributed to this patient’s current condition?
CorrectIncorrect -
Question 2 of 40
2. Question
A 1-day-old boy is in the newborn nursery for routine care. He was born to a 35-year-old mother at 38 weeks gestation via normal spontaneous vaginal delivery. There were no known complications with the pregnancy or delivery. The patient has breastfed several times and has voided and had a bowel movement. At 24 hours of life, standard pulse oximetry screening shows oxygen saturation of 89% in the right upper extremity and 88% in the left lower extremity. Physical examination reveals a slightly dusky-appearing infant who is crying and moving all extremities equally. Auscultation reveals a regular rate and rhythm with no murmurs. Over the next few hours, the patient develops increasing respiratory distress and hypotension. Repeat pulse oximetry demonstrates oxygen saturations <80% in all extremities. Blood pressure in all extremities is symmetric but low. The extremities are cold with diminished peripheral pulses. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 3 of 40
3. Question
A father brings his 10-year-old son to your office for a sports physical before beginning the basketball season. The father states that the boy has no medical issues and that this visit is more of a formality. The father reports that all of his son’s immunizations are up-to-date. The boy takes no medications and has no medication allergies. On physical examination today, his vital signs are within normal limits. The lungs are clear to auscultation, and the heart sounds are normal. There are no hernias palpated, the boy’s gait is normal, and there are no neurologic deficits. Urinalysis shows 3+ glucose. What is the most appropriate next step in this patient’s evaluation?
CorrectIncorrect -
Question 4 of 40
4. Question
A 37-year-old woman comes to the emergency department with 2 days of productive cough, fever, chills, and shortness of breath. Over the past 12 hours, the shortness of breath has progressed to the point that she can walk only a few feet before becoming prohibitively dyspneic. She has no hemoptysis, chest pain, abdominal pain, nausea, vomiting, or diarrhea. The patient’s appetite is good, and she reports no weight loss. Her medical history is significant for rheumatoid arthritis that was treated initially with methotrexate before switching to etanercept. She also takes losartan for hypertension. Tuberculin skin testing 6 months ago, prior to initiating etanercept, was negative. The patient smokes a pack of cigarettes daily and drinks alcohol occasionally. She does not use illicit drugs. Temperature is 38.3 C (101 F), blood pressure is 132/87 mm Hg, respirations are 23/min, and pulse is 114/min. Oxygen saturation is 92% on room air by pulse oximetry. The patient is in mild respiratory distress. Mucous membranes are moist, and no jugular venous distension is present. Breath sounds are decreased at the right lung base. There is swelling and redness of the small joints of the hands bilaterally. No rash is present. Chest x-ray reveals a dense opacity in the right lower lobe with a small area of cavitation. Which of the following is the most likely cause of this patient’s pulmonary findings?
CorrectIncorrect -
Question 5 of 40
5. Question
A 27-year-old woman, gravida 2 para 1, at 28 weeks gestation comes to the office for a routine prenatal visit. She has no contractions, leakage of fluid, or vaginal bleeding; fetal movements are normal. The patient had occasional nausea and vomiting during the first trimester but they resolved at 14 weeks gestation. This pregnancy has otherwise been uncomplicated. Fetal anatomy scan was normal at 20 weeks gestation. She has a history of heavy vaginal bleeding that required a blood transfusion as a teenager but has had normal menses for the past 8 years. The patient has no prior surgeries. Her last pregnancy was uneventful. She does not use tobacco, alcohol, or illicit drugs. The patient has been taking prenatal vitamins and folic acid supplements over the last year. Blood pressure is 128/72 mm Hg and heart rate is 93/min. Uterine size is appropriate for gestational age. Fetal heart rate is 150/min by Doppler ultrasound. The patient is Rh(D) negative. Her anti-Rh(D) antibody titer was 1:2 at her first prenatal visit and is now 1:16. Her current boyfriend is Rh(D) negative, but she states that this baby is from her previous boyfriend, who fathered her first child. Which of the following is the best management for this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
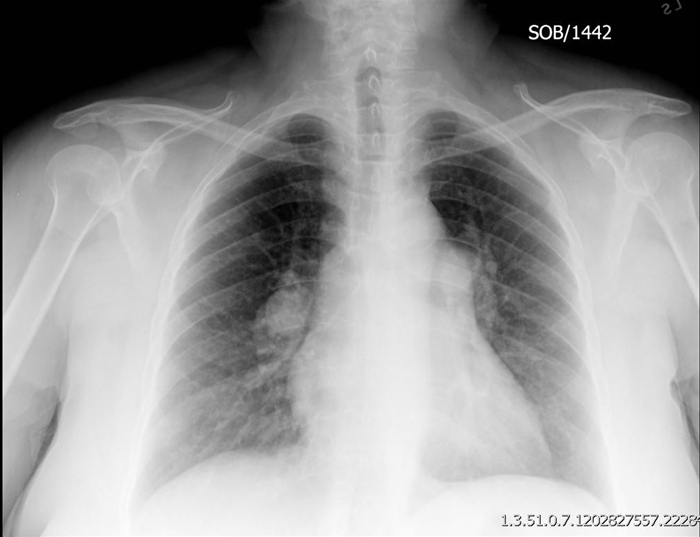
A 45-year-old woman comes to the office due to progressive exertional dyspnea and fatigue. Symptoms started approximately a year ago. Currently, the patient can walk only 2 blocks on flat ground prior to “giving out” and stopping to catch her breath. She becomes immediately fatigued and short of breath when climbing stairs. The patient also reports early satiety and a sensation of abdominal tightness. She has no skin changes, cough, orthopnea, or dysphagia. Medical history is unremarkable. The patient takes no medications and does not use tobacco or alcohol. Her husband says that she occasionally snores at night. Family history includes systemic lupus erythematosus in her mother. Blood pressure is 121/72 mm Hg and pulse is 92/min. Oxygen saturation is 92% on room air. BMI is 32 kg/m2. Muscle bulk, tone, and strength are normal. There is a grade 2/6 systolic murmur best heard at the left lower sternal border. Jugular venous pressure is elevated. The lungs are clear to auscultation. Liver span is increased. There is 1+ pitting edema in the lower extremities. Complete blood count and basic metabolic panel are unremarkable. Chest x-ray, shown in the exhibit, demonstrates normal lung parenchyma and prominent hilar vasculature. Which of the following is the most appropriate diagnostic study at this time?
 CorrectIncorrect
CorrectIncorrect -
Question 7 of 40
7. Question
A 29-year-old woman, gravida 2 para 0 aborta 1, comes to the office for an initial prenatal visit. The first day of her last menstrual period was 8 weeks ago. The patient has fatigue and mild nausea but no vomiting. She has had no pelvic pain or vaginal bleeding. Her prior pregnancy ended in a first-trimester spontaneous abortion. She has no chronic medical conditions and has had no surgeries. The patient takes a daily prenatal vitamin and folate supplementation. She does not use tobacco, alcohol, or illicit drugs. The patient is up to date on immunizations. Blood pressure is 130/84 mm Hg and pulse is 65/min. BMI is 24 kg/m2. Examination of the heart and lungs is normal; there is no peripheral edema. Pelvic examination reveals an enlarged, nontender uterus and no adnexal masses or tenderness. A scant, thin, white vaginal discharge is present on speculum examination. Transvaginal ultrasound confirms the presence of an 8-week intrauterine gestation with a normal heartbeat. A urine dipstick has trace protein and negative glucose. Which of the following tests is indicated for this patient at this visit?
CorrectIncorrect -
Question 8 of 40
8. Question
A 53-year-old man comes to the clinic due to fatigue. It is difficult for him to concentrate and he often feels sleepy during the day. The patient often falls asleep while someone is talking to him, as well as while he is stopped at traffic lights. He also reports headaches that begin in the morning when he wakes up and that do not subside until afternoon. He goes to sleep at about 11:00 PM and wakes up at 7:00 AM. His partner has witnessed episodes of the patient choking and gasping during the night. Medical history is significant for hypertension treated with lisinopril and hydrochlorothiazide and type 2 diabetes mellitus treated with metformin. The patient also takes a low-dose aspirin daily. He has smoked a pack of cigarettes a day for the last 30 years and drinks 2-3 alcoholic beverages on weekends. His mother died of a stroke at age 67, and his father suffers from diabetes mellitus and hypertension. Temperature is 36.5 C (97.7 F), blood pressure is 156/100 mm Hg, pulse is 76/min, and respirations are 14/min. BMI is 34 kg/m2 and neck circumference is 45 cm (17.7 in). Oropharyngeal examination shows moist mucous membranes and tongue scalloping. The base of the uvula and soft palate is visible. Chest auscultation reveals scattered wheezes and normal first and second heart sounds. No edema is present. Laboratory testing shows a hemoglobin level of 15.6 g/dL and an HbA1c of 7.2%. Which of the following clinical findings most strongly correlates with the disease likely causing this patient’s symptoms?
CorrectIncorrect -
Question 9 of 40
9. Question
A group of investigators are conducting a large cohort study to evaluate the effect of aortic sclerosis on cardiovascular outcomes. In this study, patients aged 50 to 85 years old seen at the primary care center are assessed for an ejection-type systolic murmur to diagnose aortic sclerosis. Those who have the murmur undergo transthoracic echocardiography to exclude aortic stenosis or other significant valvular abnormalities. The composite outcome pre-defined by investigators includes non-fatal myocardial infarction, stroke, or death from cardiovascular causes. At five years, the patients with aortic sclerosis have a relative risk of 1.53 (95% CI 1.32-1.76) to develop the composite outcome compared to those patients without aortic sclerosis. In a multivariate logistic regression model that includes the patient’s age, history of hypertension and diabetes mellitus, and smoking history, the relative risk is 1.13 (95% CI 0.86-1.31) for patients with aortic sclerosis compared to patients without aortic sclerosis. Which of the following best explains the discrepancy between the relative risk measures obtained in this study?
CorrectIncorrect -
Question 10 of 40
10. Question
A 2-week-old girl is brought to the physician for a routine visit. She was born at 37 weeks gestation to a primigravid woman by uncomplicated vaginal delivery. Her nursery course was uneventful, and her newborn screening results were normal. The patient is breastfeeding every 2 hours, and her urine and stool output are normal. Yesterday, her umbilical cord stump fell off on its own. Her abdomen is now protruding outward in a particular area, especially when she is crying, and the parents are concerned. Examination shows an alert infant with an abdomen that is soft and nontender and has bowel sounds in all four quadrants. A mass is visualized and palpated. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 12-year-old boy is brought to the emergency department with right leg pain that began immediately after he tripped during a soccer game about an hour ago. Ice was applied on the field with no relief, and the patient has been unable to walk. Since early childhood, he has experienced “growing pains” in his legs that have frequently awakened him at night. The current discomfort, however, is significantly more severe and localized. The patient has been healthy and takes no medications. He is active and enjoys playing multiple sports. On examination, he is awake and alert but in moderate pain. Cardiopulmonary examination is normal. The abdomen is soft and nontender, and the spleen is palpable 5 cm below the left costal margin. Laboratory studies show a hemoglobin level of 10.5 g/dL and platelet count of 95,000/mm3. Point tenderness is present over the right tibia proximally, and the patient is unable to bear weight on the affected leg. X-ray reveals a transverse proximal right tibial diaphyseal fracture. A metabolic disturbance of which of the following could account for this patient’s findings?
CorrectIncorrect -
Question 12 of 40
12. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 23-year-old woman, gravida 0 para 0, comes to the office for a routine visit. She has had irregular menstrual periods for the past 2 years. Many times, the bleeding lasts over 10 days and is heavy. The patient’s last menstrual period was 4 months ago. Menarche was at age 14. She is sexually active with her boyfriend and uses condoms for contraception. The patient has no chronic medical conditions or previous surgeries. She smokes a pack of cigarettes a day and drinks alcohol occasionally. Her last Pap test and sexually transmitted infection testing 6 months ago were normal. The patient’s mother has type 2 diabetes mellitus and hypertension. Her older sister has Down syndrome. Blood pressure is 144/88 mm Hg and pulse is 76/min. BMI is 37 kg/m2. Physical examination shows normal hair growth and no acne. The thyroid is not enlarged and has no nodules. There are no abdominal striae. The external genitalia are normal, and the uterus is small and nontender with no palpable adnexal masses. Urine pregnancy test is negative.
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
Item 2 of 2
The patient’s pelvic ultrasound shows a normal uterus and bilateral, polycystic-appearing ovaries. Laboratory results are as follows:
17-hydroxyprogesterone, serum
124 ng/dL (normal: <200)
Prolactin, serum
12 ng/mL (normal: <20)
Testosterone, serum
85 ng/dL (normal: 20-70)
TSH, serum
3.8 µU/mL (normal: 0.5-5)
Which of the following is the best next step in evaluation of this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 46-year-old woman comes to the emergency department after experiencing several episodes of a ”funny sensation” in her chest. These episodes started yesterday after a friend’s birthday party where the patient drank about 2 glasses of wine. She has no significant medical history. The patient works as a librarian, rides a bicycle 3 times a week, and jogs occasionally. There is no family history of coronary artery disease or stroke. On examination, she is in no acute distress. Blood pressure is 132/88 mm Hg, pulse is 122/min and irregular, and oxygen saturation is 98% on room air. Heart sounds reveal a soft S1 and a 3/6 holosystolic murmur best heard at the apex with radiation to the axilla. The lungs are clear to auscultation. There is no peripheral edema. ECG is consistent with atrial fibrillation with rapid ventricular response. The next morning, the patient’s pulse is 78/min and regular. Repeat ECG confirms normal sinus rhythm. She feels well. Echocardiography demonstrates mitral valve prolapse with severe mitral regurgitation, mild pulmonary regurgitation, and a left ventricular ejection fraction of 50%. Which of the following is the most appropriate statement to this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 62-year-old female complains of irritated, dry, ”gritty” eyes for the last several months. At times, her eyes are very sensitive to bright lights. She denies any fatigue, joint pain, weight loss, dry mouth, or difficulty swallowing. Her past medical history is significant for hypertension and hypothyroidism. She does not smoke or consume alcohol. Laboratory studies show a TSH level of 4.3 µU/mL, hemoglobin of 13.2 g/dL, platelet count of 150,000/mm3, serum creatinine level of 1.1 mg/dL, and ESR of 12 mm/hr. The antinuclear antibody (ANA) test is negative. Which of the following is the best treatment for this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
A 61-year-old female comes to your office complaining of right knee pain that limits her daily activities. She denies fever, chills, rash, or nocturnal pain. She has a past medical history of rheumatoid arthritis that has been treated for years with methotrexate and non-steroidal anti-inflammatory agents (NSAIDs). She has also received corticosteroids intermittently for disease flare-ups. She was started on infliximab recently, which has improved her morning stiffness and general well-being. Her other medical problems include hypertension and type 2 diabetes mellitus. She does not smoke cigarettes or consume alcohol. On examination, there are some deformities involving the small joints of both hands along with atrophy of the interosseous muscles. The right knee is swollen. There is pain on passive flexion of the right knee, but no joint laxity is present. Joint aspiration reveals clear fluid containing 1,000 leukocytes/mL with 30% neutrophils. Which of the following is the most likely cause of this patient’s current presentation?
CorrectIncorrect -
Question 17 of 40
17. Question
A 67-year-old man comes to the office due to 2 days of left-sided burning chest pain. The patient has never had similar symptoms. He has had no nausea, vomiting, palpitations, or shortness of breath. The patient has a history of hypertension, type 2 diabetes mellitus, and a right total knee replacement 2 years ago due to osteoarthritis. He was treated with external beam radiation therapy for localized prostate cancer 3 years ago. The patient smokes a pack of cigarettes daily and drinks beer occasionally. Temperature is 36.7 C (98.1 F), blood pressure is 143/92 mm Hg, and heart rate is 78/min. BMI is 24.5 kg/m2. Physical examination reveals scattered vesicles over the seventh left intercostal space. While discussing treatment options, which of the following should be emphasized?
CorrectIncorrect -
Question 18 of 40
18. Question
A 42-year-old Caucasian male comes to clinic with a two week history of right groin discomfort. He describes the sensation as a nagging pain that lasts for a couple of hours. Sometimes, he feels a tender fullness in his right groin. His past medical history is significant for asthma and hypertension. He uses an inhaled corticosteroid daily and albuterol as needed for wheezing and shortness of breath. For his hypertension, he takes valsartan and hydrochlorothiazide. He is a construction worker, and his job responsibilities include lifting heavy objects. Which of the following statements is most accurate regarding femoral hernias?
CorrectIncorrect -
Question 19 of 40
19. Question
A 29-year-old woman comes to the office due to inability to conceive despite appropriately timed, unprotected intercourse for the past 4 months. Menarche was at age 13; menses occur every month and last for 4-7 days. The patient takes nonsteroidal anti-inflammatory medication several times a day during her menstrual periods due to cramping. She has had no abnormal Pap tests and has a remote history of Chlamydia trachomatis cervicitis but has had negative sexually transmitted infection testing since then. The patient and her husband have no chronic medical conditions or previous surgeries. Blood pressure is 110/70 mm Hg and pulse is 70/min. BMI is 25 kg/m2. Physical examination shows a soft, nontender abdomen with no masses. Pelvic examination reveals a cervix with no discharge; a small, mobile, anteverted uterus; no cervical motion tenderness; and no palpable adnexal masses. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 25-year-old woman comes to the office due to joint pain. The patient was feeling well until 4 days ago, when she acutely developed a fever and generalized malaise. At that time, she noticed pain in her right wrist, right ankle, and the small joints of the right hand. The fever has now resolved, but the joint pain has worsened. The patient has had no chest pain, cough, abdominal pain, dysuria, hematuria, or rash. Her last menstrual period was a week ago, and she uses a copper intrauterine device for contraception. Medical history is otherwise unremarkable. Her mother has rheumatoid arthritis, and her paternal uncle has Crohn disease. The patient does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 112/71 mm Hg, and pulse is 94/min. Examination shows prominent tenderness to palpation at the right wrist and along the right extensor hallucis longus tendon with passive extension. A 5-mm, hemorrhagic pustule is noted on the sole of the right foot. Which of the following is the best diagnostic test for this patient’s condition?
CorrectIncorrect -
Question 21 of 40
21. Question
An 88-year-old female nursing home resident is admitted to the hospital because of fever, chills, and cough. She was recently discharged after an episode of aspiration pneumonia. She has lost ten pounds over the last four months. She has advanced dementia and requires constant assistance with her activities of daily living. She speaks in short sentences and does not recognize her caregivers. She is also incontinent of urine. Her other medical problems include hypertension, coronary artery disease, chronic atrial fibrillation, type 2 diabetes mellitus, and mild intermittent asthma. She has had multiple ischemic strokes in the past with some residual left-sided hemiparesis. She had coronary artery bypass surgery fifteen years ago. Her temperature is 37.8°C (100°F), blood pressure is 152/87 mmHg, heart rate is 82/min, and oxygen saturation is 92% on 2 liters of oxygen via nasal cannula. Her BMI is 18.5 kg/m2. On examination, the mucous membranes are dry and coarse rhonchi are heard over the right lower lung field. A stage 3 coccygeal pressure ulcer and a stage 2 right heel ulcer are noted. Blood cultures are sent and she is started on broad-spectrum antibiotics. Further testing in the hospital reveals severe dysphagia. Her daughter is asking about nutritional support for her mother because she is losing weight. Which of the following best addresses her concerns?
CorrectIncorrect -
Question 22 of 40
22. Question
A 62-year-old man comes to the emergency department due to shortness of breath and weakness. Over the past 4 days, he has had progressive difficulty walking due to bilateral leg weakness and has stumbled and fallen several times. The patient has also had tingling and numbness of his hands and feet as well as palpitations and light-headedness when he stands suddenly. For the past day, his hands have been weak, and he has had difficulty swallowing. The patient has had no fever, chest or abdominal pain, or bowel/bladder dysfunction. He has no prior medical history besides occasional episodes of nasal congestion. The patient has never been hospitalized and takes no medications. He smokes a pack of cigarettes and drinks 2 or 3 cans of beer a day. Which of the following is most expected on physical examination of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 56-year-old male is scheduled for a right adrenalectomy after an MRI of the abdomen showed a 5 cm mass. He initially presented with weight gain, headaches, and fatigue. He was also recently diagnosed with type 2 diabetes mellitus and started on oral hypoglycemic agents. His other medical problems include non-ulcer dyspepsia and systolic/diastolic hypertension. His pre-operative 24-hour urine cortisol excretion was 3 times the normal value and his serum ACTH level was 4 pg/mL (normal 9-52 pg/mL). Plasma fractionated metanephrines were 1.5 times the normal value. Twelve hours after surgery, the patient complains of abdominal discomfort and has one episode of non-bilious vomiting. His blood pressure is 72/40 mmHg and heart rate is 95/min, regular. Which of the following is the most likely cause of this patient’s current condition?
CorrectIncorrect -
Question 24 of 40
24. Question
A 64-year-old woman with advanced knee osteoarthritis comes to the office for preoperative assessment prior to right knee arthroplasty. The patient also has rheumatoid arthritis, which was diagnosed 15 years ago and is managed with methotrexate and adalimumab. She has taken short courses of oral glucocorticoids for acute flares; her last steroid course was approximately a year ago. The patient has difficulty climbing stairs due to joint pain but can walk 1 or 2 blocks on level ground without chest pain or shortness of breath. Blood pressure is 122/78 mm Hg, pulse is 80/min, and respirations are 16/min. Oxygen saturation is 99% on ambient air. BMI is 24 kg/m2. Oropharyngeal, cardiopulmonary, abdominal, and neurologic examinations are unremarkable. There are chronic deformities of the hand joints and wrists but no active synovitis. The right knee shows significant periarticular bony hypertrophy. Which of the following is most appropriate in the preoperative assessment of this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 72-year-old male has experienced three episodes of severe dizziness over the last two weeks. He describes ”almost passing out” each time, but denies any associated chest pain, shortness of breath, headaches, weakness or numbness. His past medical history is significant for hypertension, type 2 diabetes mellitus, and hyperlipidemia. Current medications include lisinopril, hydrochlorothiazide, metformin, and simvastatin. At his primary care provider’s office, he is found to have a blood pressure of 124/78 mmHg and heart rate of 123/min, irregularly irregular. The decision is made to transfer him to the emergency department for further evaluation. During the transfer, he experiences another episode of severe dizziness. Vital signs on arrival are blood pressure 122/72 mmHg and heart rate 53/min, regular. Physical examination reveals a faint systolic murmur over the left sternal border. The lungs are clear to auscultation. There is trace peripheral edema. Neurological examination shows good muscle strength bilaterally. An EKG reveals sinus rhythm at 55 beats per minute and no acute ST segment or T wave changes. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 26 of 40
26. Question
A 72-year-old man is brought to the office by his wife due to a hand tremor for the past 3-4 months. The tremor is most noticeable when he watches television and reads the newspaper. He has a long-standing history of type 2 diabetes mellitus, hypertension, and stage 2 chronic kidney disease. The patient is concerned that he may have Parkinson disease because he heard about it on television and read about it online. The presence of which of the following additional findings is most consistent with a diagnosis of idiopathic Parkinson disease in this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
A 68-year-old male with a past medical history of hypertension, hyperlipidemia, type 2 diabetes mellitus, and transient ischemic attacks is admitted to the hospital for chest pain. He complains of episodic substernal chest pain that radiates down his left arm for approximately 25-30 minutes. The pain is not related to exertion. He denies having palpitations, shortness of breath, nausea, vomiting, or sweating. He had a carotid endarterectomy five years ago. He has smoked one-half pack of cigarettes per day for the last 30 years and drinks alcohol occasionally. He has a strong family history of hypertension, stroke, and myocardial infarction. After his initial evaluation, an ECG is obtained that shows non-specific ST segment abnormalities in the inferior and lateral leads. The cardiac troponin T level is negative. A cardiac catheterization is performed, showing 50% atherosclerotic stenosis of the proximal left anterior descending artery and 70% atherosclerotic stenosis of the distal right coronary artery. No intervention is undertaken. On the third day of hospitalization, the patient continues to complain of occasional chest pain. His BUN level is 42 mg/dL and his serum creatinine level is 1.9 mg/dL (in comparison to a BUN of 19 mg/dL and a creatinine of 0.9 mg/dL on the day of admission). Physical examination now shows a purple discoloration of his right third toe. Which of the following additional laboratory findings would you most expect in this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 78-year-old man is brought to the emergency department from a nursing home due to 3 days of increased sleepiness. Medical history is significant for ischemic stroke, dementia, and hypertension. He is incontinent of urine and is completely dependent on caregivers for his activities of daily living. Temperature is 38.1 C (100.6 F), blood pressure is 110/58 mm Hg, and pulse is 102/min. On examination, the patient appears somewhat somnolent but is easily arousable to verbal stimuli and provides single-word answers. Pupils are equal and reactive to light. Mucous membranes are dry. The lungs are clear to auscultation and the abdomen is soft and nontender. Laboratory findings are as follows:
Leukocytes
16,500/mm3
Hemoglobin
15.2 g/dL
Platelets
344,000/mm3
Sodium
124 mEq/L
Potassium
4.4 mEq/L
Chloride
94 mEq/L
Bicarbonate
20 mEq/L
Blood urea nitrogen
46 mg/dL
Creatinine
1.2 mg/dL
Glucose
124 mg/dL
Urinalysis shows large leukocyte esterase, trace protein, and 50-100 WBCs/hpf. Which of the following is the most appropriate treatment for this patient’s electrolyte abnormalities?
CorrectIncorrect -
Question 29 of 40
29. Question
A 48-year-old woman comes to the office due to several months of vague abdominal discomfort and bloating. Her abdomen has also grown in size despite no changes to diet or activity level. The patient has a history of recurrent urinary tract infections. She is otherwise healthy but has recently had irregular menstruation, which she attributes to menopause. Family history is notable for colon cancer in her father. Temperature is 37.1 C (98.8 F), blood pressure is 142/88 mm Hg, and pulse is 78/min. BMI is 20 kg/m2. Mucosal pallor is present. Cardiopulmonary examination is normal. Abdominal palpation reveals a nontender mass in the right flank that moves with respiration. Which of the following is the most likely cause of this patient’s current abdominal finding?
CorrectIncorrect -
Question 30 of 40
30. Question
A 38-year-old woman comes to the emergency department with severe upper abdominal pain. She describes the pain as crampy and radiating between her shoulder blades. The pain started 5 hours ago and has gradually increased in intensity. The patient feels nauseated and has vomited twice since the onset of symptoms. Medical history is significant for peptic ulcer disease, nephrolithiasis, and pelvic inflammatory disease. Medications include omeprazole. The patient drinks a fifth of liquor most days of the week and reports drinking approximately twice this amount the evening prior to her symptom onset. She smokes tobacco occasionally and uses no illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 134/78 mm Hg, pulse is 112/min, and respirations are 14/min. The heart rate is regular in rhythm, and lungs are clear to auscultation bilaterally. The abdomen is nondistended and tender in the epigastric area without guarding or rebound. The extremities are warm and without edema. The remainder of the physical examination is normal. Laboratory results are as follows:
Serum chemistry
Sodium
136 mEq/L
Potassium
4.2 mEq/L
Chloride
98 mEq/L
Bicarbonate
26 mEq/L
Blood urea nitrogen
8 mg/dL
Creatinine
0.6 mg/dL
Calcium
9.4 mg/dL
Glucose
97 mg/dL
Liver function studies
Total protein
7.7 g/dL
Albumin
4.3 g/dL
Total bilirubin
0.3 mg/dL
Direct bilirubin
0.1 mg/dL
Alkaline phosphatase
70 U/L
Aspartate aminotransferase
37 U/L
Alanine aminotransferase
49 U/L
Lipase
872 U/L (normal 0-160 U/L)
The patient is admitted to the hospital and treated with intravenous fluids and hydromorphone as needed. The nausea and vomiting is treated with antiemetics. Vital signs improve several hours after admission. The following day the patient reports that her pain has resolved and that she has not vomited or felt nauseated since she came to the hospital. She asks when she will be allowed to start eating again. Which of the following is the most appropriate next step regarding management of this patient’s nutrition?
CorrectIncorrect -
Question 31 of 40
31. Question
A 62-year-old man comes to the office for follow-up after a recent hospitalization. Three weeks ago, he experienced coughing and difficulty breathing and was diagnosed with community-acquired pneumonia. The patient was admitted for antibiotic therapy, and his hospital course was complicated by an episode of severe right knee pain and swelling. Synovial fluid aspirated from the affected joint revealed uric acid crystals. The joint pain improved with treatment in the hospital, and the patient currently has no joint symptoms. In the past, he has had similar episodes of joint pain involving the right foot and left knee and is worried that it may recur. His other medical conditions include hypertension and hyperlipidemia. The patient has completed the prescribed antibiotics, and his only current medications are ramipril and atorvastatin. He drinks 1 or 2 beers on the weekend and does not smoke. Blood pressure is 129/78 mm Hg and pulse is 82/min. Lungs are clear on auscultation. Right knee examination shows full, pain-free range of motion with no erythema, warmth, or swelling. The remainder of the examination is normal. Laboratory results show a serum creatinine level of 1 mg/dL and serum uric acid level of 10.5 mg/dL. After a detailed discussion, the patient elects to begin preventive therapy in addition to lifestyle modifications, and allopurinol is prescribed. Which of the following additional interventions is most appropriate for this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 21-year-old student comes to the university health clinic due to left knee pain. For the last 3 weeks, she has had aching, poorly localized anterior knee pain that is worse when standing up from a low chair or when sitting in class for extended periods. The patient plays on a club softball team but is unable to play through a complete game due to the pain. Her medical history is unremarkable, and her only medication is an oral contraceptive. She does not use tobacco, alcohol, or illicit drugs. Temperature is 36.9 C (98.4 F), blood pressure is 118/70 mm Hg, and pulse is 68/min. BMI is 17 kg/m2. Inspection of the knee and leg is normal with no erythema, swelling, or obvious deformity. Active and passive range of motion is normal. Quadriceps strength is normal and symmetric, but squatting reproduces the pain. No focal tenderness is noted on palpation of the knee. Which of the following should be recommended to the patient at this time?
CorrectIncorrect -
Question 33 of 40
33. Question
A 54-year-old man comes to the office for a follow-up examination 2 weeks after he had an ischemic stroke. At the time of the stroke, he was also found to be in atrial fibrillation with rapid ventricular response, which was controlled with metoprolol. He currently has no symptoms. Medical history is significant for coronary artery disease, heart failure, type 2 diabetes mellitus, hypertension, hyperlipidemia, and peptic ulcer disease. He had a cardiac catheterization with stent placement in the left anterior descending artery 3 years ago. His left ventricular ejection fraction measured 2 weeks ago by echocardiography was 35%. He had an episode of upper gastrointestinal bleeding requiring hospitalization 3 years ago without any recurrence. He has a 40 pack-year smoking history but quit several years ago. Family history is significant for a stroke in his father at age 61 and diabetes mellitus in his mother. Blood pressure is 151/87 mmHg and pulse is 74/min and irregularly irregular. BMI is 30 kg/m2. On examination, no carotid bruits are heard on neck auscultation, the lungs are clear to auscultation, and there is no peripheral edema. Neurologic examination shows mild left-sided hemiparesis that does not interfere with walking. His last HbA1c was 8.1%. Which of the following places this patient at the highest risk of stroke in the future?
CorrectIncorrect -
Question 34 of 40
34. Question
A 58-year-old woman is brought to the emergency department with fevers and weakness. A week ago, she developed intermittent fevers with soaking night sweats. She also has experienced chills, malaise, and weight loss. The patient has used intravenous drugs over the past year and reports sharing needles. Medical history includes congestive heart failure, hypertension, and asthma. A recent echocardiogram showed a left ventricular ejection fraction of 30%. The patient’s medications include lisinopril, metoprolol, and inhaled albuterol. Temperature is 38.6 C (101.5 F), blood pressure is 130/75 mm Hg, pulse is 85/min, and respirations are 16/min. Physical examination is notable for a right-sided holosystolic murmur. The patient is admitted for further treatment, and blood cultures quickly grow methicillin-resistant Staphylococcus aureus. Echocardiography confirms the diagnosis of infective endocarditis. Treatment with intravenous antibiotics is initiated, and the patient’s blood cultures clear within 3 days. However, peripheral venous access is lost on hospital day 4 and is unable to be regained. The patient undergoes placement of a central line for further treatment with antibiotics. An hour later, she is found hypotensive and tachycardic, with a blood pressure of 90/50 mm Hg and a heart rate of 126/min. A chest x-ray obtained shortly after the line placement is shown below.
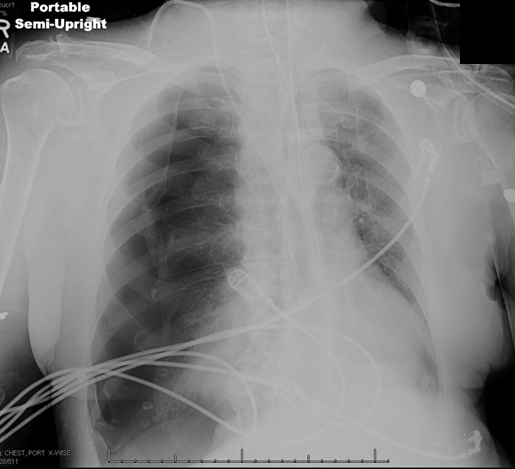
Which of the following mechanisms is likely most responsible for this patient’s hypotension?
CorrectIncorrect -
Question 35 of 40
35. Question
A 38-year-old male is brought to the emergency department after being involved in a bar fight. He has a small laceration on his right arm, a large bruise around his left eye, and several bruises in the epigastric region. There is also a laceration on his right hand that resulted from punching someone in the teeth. On physical examination, his blood pressure is 127/78 mmHg and heart rate is 82/min. There is mild upper abdominal tenderness without guarding or rebound. Chest x-ray is clear. Abdominal ultrasound does not show any intraabdominal fluid. Which of the following antibiotics is most appropriate for this patient?
CorrectIncorrect -
Question 36 of 40
36. Question
Based on a meta-analysis of several cohort studies, investigators estimate the annual risk of gastrointestinal bleeding in patients with a recent peptic ulcer-related gastrointestinal bleed to be 5 per 1,000 patients. The annual risk increases to 25 per 1,000 patients for patients started on low-dose aspirin therapy for cardiovascular prevention. What is the number needed to harm in this group of patients if they are started on aspirin?
CorrectIncorrect -
Question 37 of 40
37. Question
A 62-year-old male complains of two days of right arm pain. He denies fever, chills, joint pain, or rash. He also denies recent trauma. He has no significant past medical history. His family history is significant for hypertension, type 2 diabetes mellitus, and stroke. He has smoked one pack of cigarettes per day for the last 30 years. On physical examination, his blood pressure is 152/91 mmHg, heart rate is 86/min, and oxygen saturation is 94% on room air. His BMI is 31 kg/m2. There is pitting edema of the right arm and tortuous, engorged superficial veins over the right shoulder. The tip of the spleen is palpable below the left costal margin. His leukocyte count is 12,500/mm3, hemoglobin is 19.5 g/dL, and platelet count is 650,000/mm3. Which of the following is the most accurate test to diagnose this patient’s condition?
CorrectIncorrect -
Question 38 of 40
38. Question
A 36-year-old woman, gravida 1 para 1, comes to the office for evaluation of vaginal pruritus. She also has experienced worsening discomfort during sexual intercourse that is no longer relieved with over-the-counter lubricants. Six months ago, the patient had a vacuum-assisted vaginal delivery complicated by a third-degree perineal laceration that required extensive repair. She was placed on stool softeners for 6 weeks after the delivery. She has had 2 urinary tract infections since the delivery but has no chronic medical conditions or previous surgeries. The patient has no history of abnormal Pap tests but did have a Trichomonas vaginalis infection several years ago, which was treated with metronidazole. She has been exclusively breastfeeding her infant since delivery; the infant is healthy and meets all developmental milestones. The patient takes a prenatal vitamin daily and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 120/70 mm Hg and pulse is 84/min. BMI is 24 kg/m2. On pelvic examination, the perineal laceration repair is nontender and appropriately healed. The vaginal mucosa appears pale and thin; vaginal discharge is minimal and has a pH of 5.6. A rectovaginal examination reveals normal rectal sphincter tone. Wet mount microscopy shows no protozoa or clue cells. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to the Next Item, you will not be able to add or change an answer.
A 31-year-old woman, gravida 2 para 2, comes to the office due to fatigue, anxiety, and palpitations. She feels warm all the time, but when she takes her temperature it is consistently normal. The patient had an uncomplicated vaginal delivery 2 months ago and has not resumed normal menses. She states, “I hardly make any breast milk, and I have had to add in some formula.” The patient has had a 10-kg (22-lb) weight loss since delivery, which she thinks is “expected.” She had similar symptoms for 2 months after delivery of her first child, but her symptoms are more severe this time. Medical history is otherwise unremarkable. The patient smoked cigarettes briefly as a teenager but quit 15 years ago and does not use alcohol or illicit drugs. Her mother had a ”thyroid operation” when she was young, and her father had a stroke and has hypertension. Blood pressure is 136/67 mm Hg and pulse is 120/min. The thyroid gland is diffusely enlarged. The heart has a regular tachycardia with normal heart sounds. The hands show a fine tremor with warm, moist palms. Laboratory results are as follows:
TSH
0.01 µU/mL
Antithyroid peroxidase antibody
positive
Erythrocyte sedimentation rate
27 mm/hr
Item 1 of 2
Which of the following is the best treatment for this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
Item 2 of 2
Appropriate treatment is planned. The patient asks about the long-term consequences of her condition. Which of the following statements best addresses her concerns?
CorrectIncorrect
