Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
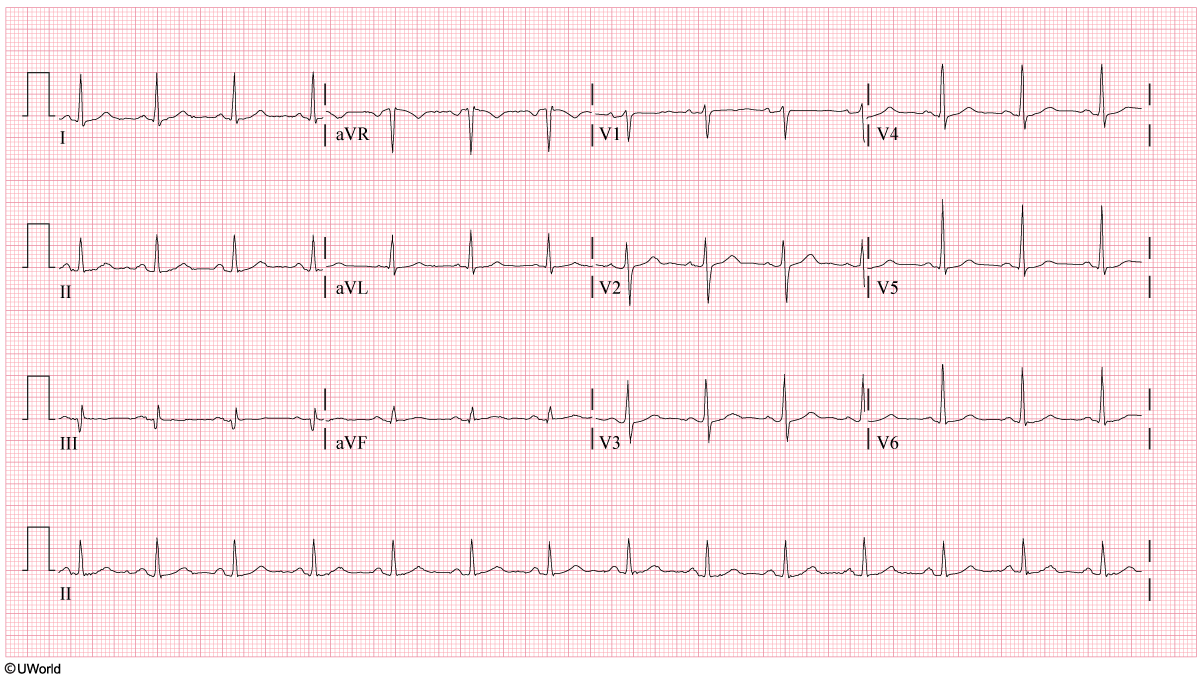
A 15-year-old boy is brought to the emergency department by ambulance after collapsing while playing basketball at school. Paramedics found the patient unresponsive and performed cardiopulmonary resuscitation for 5 minutes, after which pulse and respirations were restored. The patient has no history of trauma or chronic medical conditions and showed no prior indication of illness before his collapse. He has been hospitalized twice, once at age 4 for a febrile illness that resolved spontaneously and once at age 10 for acute appendicitis. On arrival at the emergency department, temperature is 36.7 C (98.1 F), blood pressure is 100/60 mm Hg, pulse is 72/min, and respirations are 12/min. The head is normocephalic and without trauma. The pupils are equal and reactive to light and accommodation with normal fundi. No rhinorrhea, pharyngeal erythema, or erythema of tympanic membranes is present. The neck is supple without lymphadenopathy. The lungs are clear to auscultation bilaterally. S1 and S2 are normal without murmurs, rubs, or gallops. The abdomen is soft and nontender with no organomegaly. ECG shows ST-segment elevations in leads II, III, and aVF. Further cardiac work-up demonstrates intimal thickening, calcification, and aneurysmal dilation of the proximal right coronary artery. The patient most likely has a history of what undiagnosed condition that resulted in his current findings?
CorrectIncorrect -
Question 2 of 40
2. Question
A 52-year-old man comes to the office due to progressive insomnia over the past 2 weeks. The patient has had difficulty concentrating during this period and is worried that he may be unable to complete some work projects on time. His wife also reports that he has been more irritable and agitated, particularly over the last few days. The patient has been taking his wife’s temazepam to help him sleep; nevertheless, the insomnia has not improved. Three years ago, the patient was diagnosed with cirrhosis due to nonalcoholic steatohepatitis. He has no history of hepatic encephalopathy or esophageal varices. Two months ago, ultrasonography of the abdomen revealed moderate ascites and no liver masses; the patient was prescribed furosemide and spironolactone. He also has a history of obesity, hyperlipidemia, and type 2 diabetes mellitus, which improved after gastric banding surgery 3 years ago. The patient does not use tobacco, alcohol, or recreational drugs, and he maintains a low-sodium diet. Temperature is 37.1 C (98.8 F), blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 16/min. BMI is 31 kg/m2. The patient is alert and oriented. There is no scleral icterus and the mucous membranes are moist. The lungs are clear to auscultation and heart sounds are normal with no murmurs. The abdomen is protuberant but nontender, and the liver edge is not palpable. A flapping motion occurs with hand dorsiflexion, but no focal neurologic deficits are present. Laboratory results are as follows:
Complete blood count
Hemoglobin
12.6 g/dL
Platelets
110,000/mm3
Leukocytes
7,200/mm3
Serum chemistry
Sodium
134 mEq/L
Potassium
4.2 mEq/L
Bicarbonate
24 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.9 mg/dL
Glucose
100 mg/dL
Liver function studies
Albumin
3.4 g/dL
Total bilirubin
1.0 mg/dL
Alkaline phosphatase
70 U/L
Aspartate aminotransferase (SGOT)
40 U/L
Alanine aminotransferase (SGPT)
34 U/L
Coagulation studies
INR
1.4
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
A 32-year-old woman comes to the office after requesting an urgent appointment due to “flu symptoms” for the past 2 days. She describes having headache, dizziness, chills, muscle aches, and occasional nausea. The patient says, “My husband surprised me with a trip to celebrate our wedding anniversary over the weekend. I was in such a rush to pack I left my medications and makeup bag at home. Luckily, the hotel had almost everything I needed, but I ruined the trip because I was sick for most of it.” She has been tearful and anxious since returning home earlier today, stating she is “on the verge of having a panic attack.” The patient has a history of depression and panic disorder, which have been well controlled on paroxetine for the past 3 years. Additional medical history includes hypothyroidism, treatment with a stable dose of levothyroxine, and dysmenorrhea, for which she takes ibuprofen. Height is 163 cm (5 ft 4 in) and weight is 80 kg (176.4 lb). BMI is 30 kg/m2. Temperature is 37 C (98.6 F), blood pressure is 125/75 mm Hg, and pulse is 84/min. Physical examination is normal. Mental status examination shows an anxious, irritable mood with a full range of affect. Speech is of normal rate and rhythm. She has no suicidal ideation and there is no evidence of delusions or hallucinations. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
A 67-year-old woman comes to the emergency department due to generalized weakness that has slowly worsened over the past 3 days. She has also been constipated, and her last bowel movement was 5 days ago. The patient has metastatic breast cancer and is currently undergoing combination chemotherapy. She takes oxycodone and docusate. Temperature is 37.2 C (99 F), blood pressure is 130/80 mm Hg, pulse is 94/min, and respirations are 18/min. Pulse oximetry shows 97% on room air. Mucous membranes are dry. Cardiopulmonary auscultation reveals clear lung fields and normal heart sounds. The abdomen is mildly distended, soft, and nontender. Lower extremities show no edema. Neurological examination is normal. Laboratory results are as follows:
Serum chemistry
Sodium
136 mEq/L
Potassium
5.2 mEq/L
Chloride
100 mEq/L
Bicarbonate
24 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
1.2 mg/dL
Calcium
14.3 mg/dL
Glucose
100 mg/dL
Phosphorus
3.2 mg/dL
Magnesium
2.3 mg/dL
Liver function studies
Total bilirubin
0.3 mg/dL
Alkaline phosphatase
220 U/L
Aspartate aminotransferase
12 U/L
Alanine aminotransferase
24 U/L
Gamma-glutamyl transpeptidase
25 U/L
Endocrine
Parathyroid hormone, serum
8 pg/mL
Parathyroid hormone-related peptide
1 pmol/L
(<2.0 pmol/L)
Vitamin D
1,25-dihydroxycholecalciferol
25 pg/mL
25-hydroxycholecalciferol
20 ng/mL
12-lead ECG is performed. Intravenous fluids are initiated, and the patient is admitted to the hospital. Which of the following is the most appropriate next step in management of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 5 of 40
5. Question
A 24-year-old woman is brought to the emergency department by her roommates after they found her crouched under a table in the apartment to “avoid being shot.” The patient says, “The government is monitoring my movements and has sent special agents to kill me.” She is convinced that she hears voices of people outside the apartment who are plotting against her. The patient was recently fired from her job and blames this on the “conspiracy against me.” Her roommates have never witnessed this behavior before. They report that she has a history of depression for which she takes paroxetine. They also report that she drinks beer on weekends and has a history of marijuana and cocaine use. They do not know if she is using drugs currently. Temperature is 37.8 C (100 F), blood pressure is 160/100 mm Hg, and pulse is 112/min. On examination, the patient is diaphoretic, frightened, physically restless, and tremulous. Her pupils are dilated and reactive to light. Cardiopulmonary examination shows tachycardia but is otherwise normal. The patient’s abdomen is soft and nontender with normal bowel sounds. Neurological examination is unremarkable. Which of the following is the most likely explanation for this patient’s symptoms?
CorrectIncorrect -
Question 6 of 40
6. Question
A 26-year-old woman, gravida 2 para 0 aborta 2, comes to the office for a follow-up visit 2 weeks after suction curettage was performed for an incomplete abortion. Since the procedure, the patient has had persistent vaginal spotting but no fever, chills, abdominal pain, or purulent discharge. She has hypothyroidism and is taking levothyroxine. Four years ago, the patient underwent an elective termination of pregnancy at 6 weeks gestation; she has no other previous surgeries. The patient does not use tobacco, alcohol, or recreational drugs. She conceived while taking combination oral contraceptive pills. Temperature is 36.7 C (98.1 F), blood pressure is 120/80 mm Hg, and pulse is 76/min. BMI is 25 kg/m2. Pelvic examination shows a 6-week-sized, anteverted uterus; a closed cervix; and scant discharge with minimal bleeding. The histopathologic report from the products of conception shows uterine decidua and chorionic villi. A recent TSH level was 3.3 µU/mL. The patient asks why her miscarriage occurred. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 7 of 40
7. Question
A 57-year-old African American woman comes to the emergency department with dyspnea on exertion that has been gradually progressive over the last 4-5 weeks. She has also had a nonproductive cough over the same time period, as well as fatigue and malaise for the last few months. Medical history includes coronary artery disease with a stent placed 6 months ago, triple-negative breast cancer treated with breast-conserving therapy and adjuvant chemotherapy 3 years ago, hypertension, and hyperlipidemia. The patient’s medications include lisinopril, rosuvastatin, aspirin, clopidogrel, and metoprolol. She does not use tobacco, alcohol, or illicit drugs. Family history is notable for coronary artery disease in both parents, who are now deceased. Temperature is 37.2 C (99 F), pulse is 95/min, blood pressure is 125/75 mm Hg, respirations are 18/min, and oxygen saturation is 90% on room air. Examination shows moist mucous membranes, no jugular venous distension, and no cervical lymphadenopathy. Auscultation reveals absent breath sounds and dullness to percussion over the right lung base, as well as normal S1 and S2. There is no edema. Chest x-ray reveals a large, right-sided pleural effusion and is otherwise unremarkable. A thoracentesis is performed and 1,250 mL of serosanguineous fluid is removed. Laboratory studies of the pleural fluid show the following:
Lactate dehydrogenase
200 U/L (serum level: 280)
Protein
4.2 g/dL (serum level: 7.2)
Glucose
30 mg/dL (serum level: 90)
Nucleated cells
4,000/mm3
Lymphocytes
60%
Neutrophils
35%
Eosinophils
5%
Which of the following is the most likely cause of this patient’s pleural effusion?
CorrectIncorrect -
Question 8 of 40
8. Question
A 34-year-old man comes to the urgent care center due to a day of pruritic skin rash over the lower trunk and upper thighs. He and his girlfriend are on vacation in Puerto Rico. They arrived 4 days ago; and so far during their stay, they have hiked forest trails, eaten local cuisines, and swum at the resort pool. The patient was bitten several times by insects during his hike. He has had no fever, chills, headache, abdominal pain, diarrhea, dysuria, or joint pain. The patient has a history of seasonal allergies but no other medical problems. Temperature is 36.7 C (98.1 F), blood pressure is 120/60 mm Hg, and pulse is 70/min. BMI is 26 kg/m2. Skin examination findings are shown in the image below.

The remainder of the examination is normal. Which of the following is the most appropriate next step in management of this patient’s current skin condition?
CorrectIncorrect -
Question 9 of 40
9. Question
A 62-year-old man comes to the clinic due to shortness of breath over the last 6 months. The patient has gradually felt more fatigued after his usual amount of activity and frequently needs to stop and rest. He has noticed that the symptoms are more severe in the morning. For several years the patient has had an intermittent cough productive of clear sputum. He has no orthopnea, lower extremity swelling, fever, chills, or weight loss. Medical issues include coronary artery disease with a prior bypass surgery, hypertension, major depression, squamous cell skin cancer, and hypothyroidism. He had a local excision of the skin cancer from his left forearm. The patient smoked a pack of cigarettes daily for 40 years but quit 5 years ago. He has consumed 2 or 3 beers daily for the past 40 years but has used no illicit drugs. The patient worked in an automotive factory but is currently retired. Temperature is 36.4 C (97.5 F), blood pressure is 136/82 mm Hg, pulse is 65/min, and respirations are 16/min. Pulse oximetry shows 95% on ambient air. Physical examination shows moist mucous membranes and no jugular venous distension. Heart sounds are regular in rate and rhythm with clear S1 and S2 and no murmurs. Scattered wheezes are heard over both lung fields. Respiratory effort is normal. The abdomen is soft, nontender, and nondistended. There is no peripheral edema. Laboratory testing, including complete blood count and metabolic panel, is normal. Chest x-ray reveals no infiltrates. Results of a flow-volume loop are as follows:
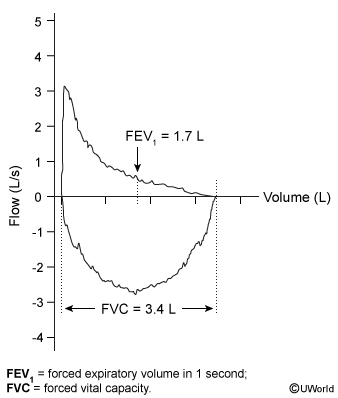
FEV1 is 60% of predicted and FVC is 75% of predicted. Diffusing capacity of the lung for carbon monoxide is within normal limits. No significant change in measured volumes is observed 15 minutes after administration of a bronchodilator. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 10 of 40
10. Question
An 80-year-old woman is brought to the emergency department after an episode of near-syncope. The patient feels excessively tired and breathless on moderate exertion and has had occasional palpitations over the past 6 months. She has had several brief episodes of lightheadedness during the last 2 weeks, and while walking in a mall today, she felt extremely weak and dizzy. The patient was helped by her family and did not fall or lose consciousness. She has had no chest pain, cough, or pedal edema. The patient has hypertension and was diagnosed with paroxysmal atrial fibrillation a year ago. She takes apixaban and valsartan. Blood pressure is 156/80 mm Hg and pulse is 52/min without significant orthostatic changes. No jugular venous distension is present. Cardiac auscultation reveals regular S1 and S2 with S4 but no murmurs. Carotid pulses are full and symmetric. Breath sounds are normal with no crackles. There is no extremity edema. ECG shows sinus bradycardia and right bundle branch block. Laboratory results show normal blood count, serum electrolytes, and renal function. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 11 of 40
11. Question
A 66-year-old man with end-stage renal disease comes to the emergency department due to left elbow pain. He first noted the pain while undergoing hemodialysis the previous day. The patient has no other joint symptoms, history of similar pain, or recent trauma to the elbow. In addition to chronic kidney disease, medical history is notable for type 2 diabetes mellitus, hypertension, and peripheral arterial disease. He quit smoking 3 years ago and does not use alcohol or recreational drugs. Temperature is 36.8 C (98.2 F), blood pressure is 144/92 mm Hg, and pulse is 96/min. Examination shows erythema and swelling at the posterior left elbow. Range of motion is limited due to pain. Laboratory results are as follows:
Serum chemistry
Sodium
132 mEq/L
Potassium
5.0 mEq/L
Creatinine
4.8 mg/dL
Calcium
10.3 mg/dL
Complete blood count
Hemoglobin
10.9 g/dL
Leukocytes
8,000/mm3
Platelets
136,000/mm3
X-ray of the elbow is shown in the exhibit. Which of the following is the most appropriate next step in evaluation of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 12 of 40
12. Question
A 55-year-old woman is brought to the emergency department after collapsing during a prolonged coughing episode at home. Her husband reports that she has had a dry cough and shortness of breath for the last 5 days. Shortly after arriving at the emergency department, the patient is intubated due to worsening tachypnea and increased work of breathing. The patient has a history of type 2 diabetes mellitus, hypothyroidism, and a recent diagnosis of polymyositis. She currently takes prednisone, azathioprine, metformin, and levothyroxine; her prednisone dose was recently reduced from 60 mg to 40 mg daily. She has no known drug allergies, and does not use tobacco, alcohol, or receational drugs. Temperature is 37.8 C (100 F), blood pressure is 110/60 mm Hg, pulse is 100/min, and respirations are 18/min. Pulse oximetry reading prior to intubation was 76% on room air, improving to 98% with 60% FiO2 after intubation. The endotracheal tube is in place, and the patient has moist mucous membranes. Cardiopulmonary auscultation reveals diffuse crackles and rhonchi. Laboratory results are as follows:
Complete blood count
Hemoglobin
10.4 g/dL
Mean corpuscular volume
90 µm3
Platelets
210,000/mm3
Leukocytes
12,000/mm3
Neutrophils
92%
Lymphocytes
3%
Monocytes
5%
Eosinophils
0%
Arterial blood gases (on room air)
pH
7.45
PaO2
45 mm Hg
PaCO2
29 mm Hg
Chest x-ray prior to intubation is shown below:

Pharmacological prophylaxis with which of the following medications would have most likely prevented the patient’s current condition?
CorrectIncorrect -
Question 13 of 40
13. Question
A 62-year-old woman comes to the office for follow-up on hypertension and knee osteoarthritis. She has noticed marked improvement of her knee pain since she started taking naproxen, chondroitin, and glucosamine a month ago. During previous office visits, her blood pressure ranged between 110/66 mm Hg and 130/84 mm Hg. The patient’s other medications include simvastatin, amlodipine, and lisinopril, which she has taken for the past 6 years. She has never used tobacco and drinks a glass of wine most evenings. Today, blood pressure is 153/96 mm Hg in the right arm and 154/98 mm Hg in the left. Pulse is 78/min and regular and respirations are 14/min. BMI is 26 kg/m2. There is no carotid bruit or jugular venous distension. The lungs are clear to auscultation, and heart sounds are normal with no murmur, gallops, or rubs. The abdomen is nondistended, soft, and nontender with normoactive bowel sounds. There is no hepatosplenomegaly. There is mild joint line tenderness and crepitus on knee examination. Mild ankle edema is noted bilaterally. ECG shows no abnormalities. Complete blood count and serum chemistry studies are within normal limits. Which of the following is the best recommendation for this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 25-year-old woman, gravida 1 para 0, at 16 weeks gestation comes to the office for routine prenatal care. The patient has had no vaginal bleeding or cramping, but she reports a painful lesion on her right labium majus for the past 3 days. The lesion was initially pustular but after 2 days eroded into an ulcer that has been draining clear fluid. The patient has no other chronic medical conditions and has never had a similar lesion previously. She takes a prenatal vitamin daily and does not use tobacco, alcohol, or recreational drugs. Temperature is 37.2 C (99 F) and blood pressure is 100/60 mm Hg. The fetal heart rate is 150/min by Doppler ultrasound. Pelvic examination shows a tender 2-cm shallow erosion on the right labium majus with an erythematous base. Speculum examination shows no cervical or vaginal lesions, and there is no inguinal lymphadenopathy. The patient is prescribed antiviral therapy for 7 days and returns for follow-up. Her symptoms have resolved and physical examination confirms that the lesion is no longer present. Which of the following is the most appropriate strategy to decrease the risk of perinatal transmission?
CorrectIncorrect -
Question 15 of 40
15. Question
A 1-day-old boy is being evaluated routinely in the nursery. He was born to a 37-year-old primigravida at 38 weeks gestation via vaginal delivery. The mother received routine prenatal care and her serologies for HIV, hepatitis B, and syphilis were negative. She received intrapartum antibiotic prophylaxis for a positive group B Streptococcus genital culture in the third trimester. The mother and father are otherwise healthy with no medical problems. On examination of the boy’s external genitalia, a ventrally positioned urethral meatus is noted on the shaft of the penis and the penis is curved downward. Both testicles are easily palpated within the scrotum. The remainder of the newborn examination is normal. What is the most appropriate management of this patient’s condition?
CorrectIncorrect -
Question 16 of 40
16. Question
A 6-month-old boy is brought to the office due to fever, which he has had for the past 2 days. He had difficulty sleeping the previous night. The patient had an episode of nonbloody, nonbilious emesis yesterday and several loose stools today; his appetite has decreased slightly during this period. Urine output has been normal. There have been no medical problems since birth. The patient was born at 40 weeks gestation after an uncomplicated pregnancy. Height, weight, and head circumference have remained at the 50th percentile since birth. His immunizations are up to date. He lives with both parents and a 4-year-old sibling. His diet consists of milk-based infant formula every 3 hours. The patient takes no medications and has no known allergies. Temperature is 38.3 C (101 F), pulse is 132/min, and respirations are 26/min. He is awake and alert but cranky. Nares are clear with no rhinorrhea and mucous membranes are moist. Heart sounds are normal without murmurs. Lungs are clear to auscultation bilaterally. The abdomen is soft and nontender with normal bowel sounds. There are no rashes or skin lesions. Which of the following is the best next step in the management of this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
The following vignette applies to the next 2 items.
A 28-year-old woman comes to the clinic due to generalized fatigue. The patient has also had several months of intermittent heavy menstrual bleeding, “spots” on her skin, and small streaks of blood when she blows her nose. She has had no dyspnea, fever, night sweats, or weight loss. The patient has a history of hypothyroidism and asthma treated with levothyroxine and inhaled albuterol. Her mother, father, and 2 siblings have no chronic medical problems. She does not use tobacco, alcohol, or illicit drugs. Temperature is 36.7 C (98.1 F), blood pressure is 120/70 mm Hg, pulse is 88/min, and respirations are 12/min. BMI is 22 kg/m2. Mucous membranes are moist, and no thyromegaly is present. Cardiopulmonary auscultation indicates clear lung fields and normal first and second heart sounds. The abdomen is soft and nontender, with no hepatomegaly or splenomegaly. Skin examination shows several flat, erythematous/violaceous 1- to 3-mm (.04- to .12-in) lesions on the lower extremities. The color of the lesions does not change with pressure. Laboratory results are as follows:
Complete blood count
Hemoglobin
9.8 g/dL
Mean corpuscular volume
72 µm3
Platelets
16,000/mm3
Leukocytes
7,500/mm3
Liver function studies
Total protein
7.5 g/dL
Albumin
4 g/dL
Total bilirubin
0.3 mg/dL
Alkaline phosphatase
120 U/L
Aspartate aminotransferase
37 U/L
Alanine aminotransferase
49 U/L
Coagulation studies
Prothrombin time
12 sec
International normalized ratio
1.0
Activated partial thromboplastin time
38 sec
HIV antibody/p24 antigen
negative
Thyroid stimulating hormone
2.4 µU/mL
A peripheral smear shows a reduced number of morphologically normal platelets; hypochromic, microcytic red blood cells that vary in shape and size; and normal-appearing leukocytes.
Item 1 of 2
Which of the following is the most likely diagnosis for this patient?
CorrectIncorrect -
Question 18 of 40
18. Question
Item 2 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
A 14-year-old girl with a history of seizure disorder is brought to the office by her mother for follow-up. The patient has tried several anticonvulsant medications with no improvement. Her mother wonders if other epileptic medications might improve her daughter’s condition. The patient and her mother describe daily seizures characterized by falling to the floor followed by generalized convulsive and thrashing movements. The seizures last 1-2 minutes and are usually, but not always, followed by a period of confusion. The patient says, “The seizures are still pretty bad. It’s hard to take the medication when it’s obviously not working.” The mother is considering home schooling her daughter as the seizures frequently occur at school and have been embarrassing for the patient. Video electroencephalogram, performed at a hospital last week, shows that the patient had several episodes of shaking that were not associated with any abnormalities. Vital signs and physical examination are normal. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 38-year-old man comes to the emergency department due to several weeks of subjective fever, night sweats, malaise, and shortness of breath. He has also had anorexia, vague abdominal discomfort, and unspecified weight loss. The patient was diagnosed with HIV 2 years ago but is not compliant with HIV-related medications. His most recent visit to the HIV clinic was a year ago, and he does not know his last CD4 count or viral load. The patient smokes marijuana and has used injection drugs in the past. He was recently released from prison and is living with his mother in Massachusetts. Temperature is 37.2 C (99 F), blood pressure is 118/78 mm Hg, pulse is 90/min, and respirations are 18/min. The patient’s pulse oximetry shows 88% while breathing ambient air. BMI is 19 kg/m2. Physical examination reveals bitemporal wasting, moist mucous membranes, and flat neck veins. Diffuse, bilateral crackles are present on lung auscultation. Heart sounds are normal with no murmur. The abdomen is soft with mild right upper quadrant tenderness. Bowel sounds are normal. No extremity edema is present. Neurologic examination is within normal limits. Laboratory results are as follows:
Complete blood count
Hemoglobin
9.6 g/dL
Hematocrit
28%
Mean corpuscular volume
88 µm3
Platelets
90,000/mm3
Leukocytes
3,500/mm3
Serum chemistry
Sodium
131 mEq/L
Potassium
4.2 mEq/L
Bicarbonate
26 mEq/L
Blood urea nitrogen
10 mg/dL
Creatinine
0.6 mg/dL
Calcium
10.2 mg/dL
Glucose
100 mg/dL
Liver function studies
Total protein
7.8 g/dL
Albumin
3.4 g/dL
Total bilirubin
1.3 mg/dL
Alkaline phosphatase
170 U/L
Aspartate aminotransferase
162 U/L
Alanine aminotransferase
174 U/L
Chest imaging findings are shown below.

This patient’s current symptoms are most likely due to active infection with which of the following?
CorrectIncorrect -
Question 21 of 40
21. Question
A 13-month-old girl is brought to the office in February due to diarrhea. She had 2 episodes of nonbilious emesis the previous day, followed by copious watery diarrhea that “runs out of her diaper.” Since yesterday, she has had 12 large, watery bowel movements. Her mother states, “She doesn’t want to eat anything. Normally she drinks 18 ounces of milk a day, but now she’s only drinking about half of that.” The family moved to New York when the child was born, and last week they traveled to Florida for the winter holiday. During the trip, the patient ate hamburger for the first time at a family barbecue and played in her uncle’s pool. Since returning home, the girl has attended day care over the past few days except for today due to the diarrhea. Medical history is significant only for an episode of otitis media requiring antibiotics at age 9 months. She currently takes no medications and has never been vaccinated due to parental preference. Temperature is 38 C (100.4 F) and pulse is 118/min. On physical examination, the patient’s lips and skin are slightly dry. Cardiopulmonary examination is unremarkable. The abdomen is nondistended and soft with hyperactive bowel sounds. There is no tenderness to palpation. Which of the following practices would have been most effective in preventing this patient’s symptoms?
CorrectIncorrect -
Question 22 of 40
22. Question
An 18-month-old girl is brought to the office for a routine well-child visit. Her parents are concerned about her dietary habits and say that she is a picky eater. She will eat only fruit, bread, eggs, and cheese. They have offered meat (eg, beef, chicken, shellfish), nut products, and vegetables several times, but she tends to spit the food out or refuses to open her mouth. The mother says, “She mostly feeds herself with her fingers or a spoon but is very sloppy. Most of the food seems to end up on her high chair and not in her mouth.” The parents switched the girl from a bottle to a cup with a spout last month, and her whole milk intake dropped from 20 oz to 8 oz a day. Her bowel habits have also recently changed from stooling once every other day to twice a day. The child can say 10-15 words and walks well. The father has a severe peanut and shellfish allergy for which he carries an epinephrine pen. The patient’s medications include a daily multivitamin and occasional topical emollients for eczema. Medical records show weight consistently at the 10th percentile and length at the 20th percentile. Physical examination shows an alert and playful girl. She has dry, erythematous patches of skin on her cheeks and wrists. The remainder of her examination is unremarkable. The mother says, “She’s the smallest child in her day care class. I’m concerned about her growth.” Which of the following is the most appropriate step in management of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 47-year-old man comes to the office due to a 4-month history of cough. The patient reports frequent episodes of paroxysmal coughing spells productive of small amounts of white sputum. On several occasions, wheezing and chest tightness have occurred. The patient has no fever, dyspnea on exertion, or heartburn. He has no other medical conditions and takes no medications. The patient has never smoked, does not use recreational drugs, but drinks 1 or 2 cans of beer daily. He started working as an industrial welder after losing his job as an electrician 18 months ago. The patient has no pets. He traveled to Connecticut 2 months ago for vacation, during which time his breathing was “a lot better than normal.” The patient has lived with his wife in the same house for the past 20 years, and she has no respiratory symptoms, but his sister has asthma. Temperature is 37 C (98.6 F), blood pressure is 128/74 mm Hg, pulse is 68/min, and respirations are 16/min. Oxygen saturation is 98% on ambient air. Nasopharyngeal mucosae are normal with no sinus tenderness. The remainder of the physical examination is normal. Blood cell counts and serum chemistry are within normal limits. Chest x-ray reveals no abnormalities, and office spirometry is normal. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
A 64-year-old woman comes to the office for a new patient visit. She recently relocated to the area to live with her son. The patient reports occasional knee pain from osteoarthritis, which responds to acetaminophen, and she also takes amlodipine for hypertension. She has no other symptoms or chronic health issues. She is a former smoker with a 10-pack-year smoking history and does not use alcohol or receational drugs. Blood pressure is 140/85 mm Hg and pulse is 78/min. There is no carotid bruit and jugular venous pressure is normal. Lungs are clear to auscultation and heart sounds are normal with no murmur. The abdomen is soft and nontender with no organomegaly. There is mild crepitus with range of motion at the knees, but no joint erythema, effusion, or tenderness. Funduscopic examination reveals enlargement of the optic cups with an increased cup:disc ratio bilaterally. Perimetry testing shows mild peripheral visual field loss. Tonometry reveals normal bilateral intraocular pressures. Which of the following is the most likely cause of this patient’s current eye findings?
CorrectIncorrect -
Question 25 of 40
25. Question
A 61-year-old postmenopausal woman comes to the office for abdominal distension, bloating, and lower abdominal pain over the past 4 months. The patient also reports an 8-kg (17.6-lb) unintentional weight loss during this time and says that it is due to decreased appetite; she is routinely unable to finish her meals. The patient has a history of type 2 diabetes mellitus and hypertension controlled by oral medications. She has had a laparoscopic cholecystectomy and appendectomy. There is no history of gynecologic issues other than unexplained infertility. Menopause was at age 54, and she used hormone replacement therapy for 5 years afterward. The patient has had no postmenopausal bleeding. Family history is significant for colorectal cancer in her father at age 70; otherwise, it is noncontributory. Temperature is 36.7 C (98 F), blood pressure is 130/80 mm Hg, pulse is 72/min, and respirations are 18/min. BMI is 32 kg/m2. On abdominal examination, there is mild tenderness to deep palpation in the right lower quadrant. Bimanual examination reveals right-sided adnexal fullness. Laboratory results are as follows:
Complete blood count
Hemoglobin
10.6 g/dL
Mean corpuscular volume
82 µm3
Platelets
140,000/mm3
Leukocytes
4,100/mm3
Serum chemistry
Creatinine
0.8 mg/dL
Liver function studies
Albumin
3.7 g/dL
Aspartate aminotransferase (SGOT)
37 U/L
Alanine aminotransferase (SGPT)
49 U/L
Pelvic ultrasound reveals a small uterus with a thin endometrial lining and a 6-cm lobulated right adnexal mass with thick internal septations and mild ascites. CT scan of the chest, abdomen, and pelvis confirms the adnexal mass and ascites with no distant lesions. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 26 of 40
26. Question
A 27-year-old woman, gravida 1 para 0, at 16 weeks gestation comes to the office after a recent exposure to sick children. She is a preschool teacher, and 4 children in her classroom have been sent home with fever, red cheeks, and a lacy rash on the trunk over the past 2 weeks. The patient is afebrile but has had a sore throat and cough for the past 24 hours. She reports no vaginal bleeding or cramping. Prior to this, her pregnancy was uncomplicated and all initial prenatal laboratory findings were normal. She has allergic rhinitis for which she takes a daily antihistamine. Surgical history includes a laparoscopic appendectomy. The patient also takes a daily prenatal vitamin and occasional acetaminophen. She does not use tobacco, alcohol, or illicit drugs. The patient was adopted and is unaware of any family history. Temperature is 37.1 C (98.8 F), blood pressure is 98/66 mm Hg, and pulse is 84/min. The uterus is palpable 4 fingerbreadths below the umbilicus, and fetal heart rate is auscultated at 162/min via handheld Doppler. She has no signs of a rash and can move her upper and lower extremities freely without pain. Which of the following is the best advice for this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
A 52-year-old man is admitted to the intensive care unit due to intracranial hemorrhage. The patient came to the emergency department with severe headache several hours ago and became increasingly somnolent. Endotracheal intubation was performed for airway protection and a noncontrast CT scan of the head revealed a right basal ganglia hemorrhage. The patient has a history of hypertension but has been nonadherent to treatment. Temperature is 37.1 C (98.8 F), blood pressure is 178/106 mm Hg, and pulse is 96/min. On examination, the patient is lightly sedated and withdraws to noxious stimuli. The intravenous access, arterial line, and endotracheal and nasogastric tubes are in adequate position. The lungs are clear on auscultation and heart sounds are normal. The patient is receiving intravenous infusions of antihypertensives and sedatives. Deep venous thrombosis prophylaxis with intermittent pneumatic compression devices and enteral feeding via a nasogastric tube are initiated. Intracranial pressure monitoring is planned. Which of the following is the most appropriate intervention to prevent ventilator-associated pneumonia in this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 35-year-old man comes to the office due to difficulty sleeping. He often lies awake at night, unable to relax and worries about how he will function at work the following day. The patient describes taking 1-2 hours to fall asleep and frequently waking in the middle of the night due to recurrent nightmares. During the day, he feels anxious and tense. He has difficulty focusing on his job and describes lapses in concentration in which he experiences disturbing visual images related to a car accident a year ago. The patient denies feeling depressed but notes that his wife says that he is more irritable than usual. He uncharacteristically yells at his kids for making too much noise and argues with his wife over minor issues. The patient has a history of neck stiffness and chronic knee pain due to injuries sustained in the accident. He limits caffeine to 2 cups of coffee in the morning. He does not use alcohol or illicit drugs. Vital signs are stable. Physical examination is remarkable for a well-healed scar and decreased range of motion of the right knee joint. In addition to recommending psychotherapy, which of the following is the most appropriate pharmacotherapy?
CorrectIncorrect -
Question 29 of 40
29. Question
A 52-year-old woman comes to the office 2 weeks after undergoing elective laparoscopic cholecystectomy for intermittent biliary colic. The cholecystectomy revealed multiple small gallstones. There were no complications, but the patient has had intermittent upper abdominal pain and nausea since the procedure. She has been able to tolerate a regular diet but requires acetaminophen-hydrocodone for the pain. The patient has a history of hyperlipidemia. She does not use tobacco or recreational drugs and occasionally drinks alcohol. Her father has cirrhosis. Temperature is 37.1 C (98.8 F), blood pressure is 130/90 mm Hg, and pulse is 70/min. BMI is 34.2 kg/m2. Sclerae are mildly icteric, and mucous membranes are moist. The lungs are clear to auscultation, and heart sounds are normal. The abdomen is soft with mild tenderness in the right upper quadrant; no rebound tenderness or guarding is present. The surgical incisions are healing well without erythema or discharge. Bowel sounds are normal. Laboratory results are as follows:
Complete blood count
Hemoglobin
13 g/dL
Platelets
320,000/mm3
Leukocytes
12,000/mm3
Serum chemistry
Sodium
140 mEq/L
Potassium
4.2 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Glucose
100 mg/dL
Liver function studies
Albumin
4 g/dL
Total bilirubin
3.8 mg/dL
Indirect bilirubin
1.0 mg/dL
Alkaline phosphatase
320 U/L
Aspartate aminotransferase (SGOT)
82 U/L
Alanine aminotransferase (SGPT)
94 U/L
Lipase
36 U/L
Coagulation studies
INR
0.8
Which of the following is the most likely cause of this patient’s current condition?
CorrectIncorrect -
Question 30 of 40
30. Question
A 55-year-old woman, gravida 2 para 2, comes to the office for postcoital vaginal bleeding. The patient’s last menstrual period was a year ago, but she has had intermittent, postcoital vaginal bleeding for the past 6 weeks. Over the last week, her bleeding has increased so that she now has to use a pad each day. She has also noticed pain with intercourse, requiring the use of a water-based lubricant. The patient has no weight loss, abdominal pain, distension, or abnormal vaginal discharge. She has no chronic medical conditions. Surgical history is significant for 2 cesarean deliveries and a bilateral tubal ligation. Her last Pap test, 2 years ago, was normal. Her maternal aunt had epithelial ovarian cancer at age 49. The patient takes a daily multivitamin and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 130/80 mm Hg, pulse is 72/min, and respirations are 14/min. BMI is 30 kg/m2. The abdomen is soft, nontender, and nondistended with no palpable masses. Pelvic examination reveals pale, thin vaginal mucosa without excoriations or lesions. There is minimal dark red blood in the vaginal vault, but no cervical lesions. The uterus is small, mobile, and nontender; the ovaries are not palpable. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 34-year-old man comes to the office for follow-up 1 week after being discharged from the hospital. The patient had gone to the emergency department due to sudden-onset left-sided flank pain. He says, “The pain was like the pain I had when I passed a kidney stone 4 years ago.” CT scan of the abdomen revealed a left-sided 3-mm ureteric calculus with no hydronephrosis. The patient was treated with intravenous fluids and analgesics and passed the stone spontaneously. He did not catch the stone for analysis, but his previous stone contained calcium. The patient has no other medical conditions and takes no medications. Temperature is 36.4 C (97.5 F), blood pressure is 120/80 mm Hg, and pulse is 74/min. Physical examination shows no abnormalities. Laboratory results are as follows:
Complete blood count
Hemoglobin
13.8 g/dL
Platelets
320,000/mm3
Leukocytes
8,100/mm3
Serum chemistry
Sodium
140 mEq/L
Potassium
4.4 mEq/L
Bicarbonate
26 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Glucose
90 mg/dL
Calcium
9.2 mg/dL
Urinalysis shows no proteinuria, hematuria, or pyuria. The patient says, “I’ve been drinking plenty of fluids since the last time I had this, but I still developed another stone. Isn’t there something else I can do to prevent this?” Which of the following is the best response to this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
An 18-month-old boy is brought to the emergency department by his parents due to cough. He has had clear rhinorrhea and tactile fever for the past 2 days and woke up abruptly last night with harsh, forceful coughing. There has been no emesis or diarrhea. The patient attends day care, where several children have had congestion and cough. Medical history is significant for birth at 34 weeks gestation. He has no chronic health issues, takes no medications, and is unvaccinated. Temperature is 38 C (100.4 F), pulse is 124/min, and respirations are 32/min. Physical examination shows an alert, crying child with mild inspiratory stridor; when he attempts to run from the examiner, he has an episode of dry, hoarse cough, and his stridor worsens. The pharynx is not erythematous, and the tympanic membranes are gray with normal light reflex and landmarks. Lung fields are clear without wheezes or rales, but subcostal and intercostal retractions are present. S1 and S2 are normal without murmurs. Which of the following interventions could have reduced the risk of this patient’s condition?
CorrectIncorrect -
Question 33 of 40
33. Question
An 82-year-old woman is brought to the emergency department after an episode of syncope. Her daughter reports that they were standing in the lobby of their church when her mother collapsed. The daughter did not witness any convulsions and says her mother regained consciousness after a few seconds. The patient does not recall feeling lightheaded prior to this episode. In the last 2 months she has had episodes of lightheadedness about 3 times a week while both sitting and standing. She has a history of hypertension, osteoporosis, vitamin D deficiency, and gastroesophageal reflux disease. She denies any history of vertigo. The patient had a biopsy of a benign thyroid nodule a few years ago but has had no other surgery. She takes amlodipine, enalapril, omeprazole, and a vitamin D supplement. She has no allergies. The patient does not use tobacco or alcohol. Her mother died of a stroke at age 90. Temperature is 36.1 C (97 F), blood pressure is 140/80 mm Hg, pulse is 61/min, and respirations are 14/min. Pulse oximetry shows 97% on room air. Height is 160 cm (5 ft 3 in) and weight is 65 kg (143.3 lb). Physical examination reveals moist mucous membranes, normal jugular venous pressure, clear lung fields, and normal first and second heart sounds. The abdomen is soft and nontender. Lower extremity examination shows trace pretibial edema bilaterally. Spine examination shows mild kyphosis, but there is no tenderness to palpation of the lower back or pain with range of motion of the neck. Muscle strength is diffusely mildly reduced in the upper and lower extremities, but there are no focal deficits, and upper and lower limb deep tendon reflexes are 2+. Laboratory results are below:
Complete blood count
Leukocytes
8,000/mm3
Hemoglobin
12.6 g/dL
Hematocrit
38%
Platelets
200,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
4.2 mEq/L
Chloride
108 mEq/L
Bicarbonate
24 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Calcium
8.8 mg/dL
Glucose
80 mg/dL
Cardiology
Troponin T, serum
<0.01 ng/mL
Chest x-ray reveals a previous vertebral compression fracture and a hiatal hernia, but there is no acute cardiopulmonary finding. ECG reveals normal sinus rhythm with a right bundle branch block and a left anterior fascicular block. Transthoracic echocardiogram shows normal left and right ventricular function and no significant valvular disease. Which of the following is the most likely cause of this patient’s syncope?
CorrectIncorrect -
Question 34 of 40
34. Question
A 3-year-old boy with sickle cell disease is brought to the emergency department with sudden onset of difficulty walking. The patient was behaving normally before his nap but was unable to get out of bed or walk across the room when he woke up. His mother says that his right hand also seems “clumsy.” Over the past year, the patient has had 2 hospitalizations for severe upper extremity and back pain, but over the past 4 months, he has been healthy with no pain, shortness of breath, or fatigue. Temperature is 36.7 C (98 F), blood pressure is 90/50 mm Hg, pulse is 120/min, and respirations are 22/min. Cardiovascular examination shows a regular rate and rhythm with normal S1 and S2 and no murmurs, rubs, or gallops. Significant weakness and hypotonia of the right arm and leg are present. Which of the following screening tests could have identified an increased risk for this patient’s acute diagnosis?
CorrectIncorrect -
Question 35 of 40
35. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to the Next Item, you will not be able to add or change an answer.
A 29-year-old woman comes to the office for follow-up. She was seen a month earlier for stomach upset, headaches, muscle aches and pains, insomnia, and fatigue. Examination and routine laboratory tests were normal and she was treated symptomatically. At today’s visit, the patient says, “I was worried I had some kind of flu, but it’s been going on too long. I occasionally feel queasy during the day. At night, I can’t sleep because my back and shoulders hurt and I lie awake with negative thoughts.” Further questioning reveals that the patient has had intermittent headaches, anxiety, insomnia, and fatigue for several years. She says, “I often feel overwhelmed and exhausted. I put a lot of stress on my body worrying about every little thing. I’m ‘keyed up’ all the time and snap at my husband and coworkers. When I am under pressure at work my chest feels tight and I can get dizzy. I’m always running to the bathroom. On top of everything else, I’m depressed that my mother was recently diagnosed with breast cancer.” Medical history is significant for eczema, insomnia, and migraine headache. The patient drinks a glass of wine several times a week and does not use illicit drugs. She drinks 2 cups of coffee in the morning but avoids caffeine at night. Temperature is 36.7 C (98 F), blood pressure is 110/70 mm Hg, pulse is 84/min, and respirations are 16/min. Physical examination is normal.
Item 1 of 2
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 36 of 40
36. Question
Item 2 of 2
The patient is given a referral for psychotherapy. However, she returns 6 months later and reports that her insurance covered only 3 sessions, and she continues to experience chronic worry, anxiety, and tension. The patient says, “I have difficulty falling asleep because I am thinking about stuff that occurred during the day and worrying how I will accomplish everything I have to do tomorrow on such little sleep. I worry about every little thing and can’t slow my mind down.” The patient continues to experience intermittent headaches, and shoulder and back pain. She says, “I can’t even relax on weekends. My husband is upset because I never want to do anything; I’m too tired.” The patient asks if there is a medication she can take. Which of the following would be the most appropriate pharmacotherapy?
CorrectIncorrect -
Question 37 of 40
37. Question
A 6-month-old girl is brought to the emergency department due to a fever and a rash. For the past 4 days, the patient has had a fever, dry cough, and rhinorrhea. Two days ago, she developed a rash on her cheeks and forehead, which has slowly spread to the rest of her body. During a trip to Mexico 3 weeks ago, she developed 2 days of vomiting and diarrhea after drinking a smoothie. The patient was born full-term without complications and has no chronic medical problems. She lives with her parents and 3-year-old brother. She attends day care 5 days a week and has no known sick contacts. Temperature is 39.1 C (102.4 F), blood pressure is 90/60 mm Hg, pulse is 135/min, and respirations are 20/min. Physical examination shows a tired-appearing infant resting in her mother’s lap. Bilateral conjunctivae are mildly erythematous with no discharge. Mucous membranes are moist with no lesions. A maculopapular, blanching, dark-red rash covers her entire body aside from her palms and soles. No petechiae, ecchymoses, or purpura is noted. Auscultation of the chest reveals no murmurs or adventitious lung sounds. What is the most likely route of transmission of this patient’s disease?
CorrectIncorrect -
Question 38 of 40
38. Question
A 32-year-old woman, gravida 2 para 1, at 9 weeks gestation comes to the office to establish prenatal care. The patient has had nausea and vomiting relieved by vitamin B6 supplementation. She has no abdominal pain or vaginal bleeding. Her previous pregnancy required an induction of labor for oligohydramnios at 40 weeks gestation, which resulted in an uncomplicated vaginal delivery. The patient has no chronic medical conditions and has had no previous surgeries. She has no history of sexually transmitted infections. The patient is up to date on all vaccinations and takes a daily prenatal vitamin. Blood pressure is 100/70 mm Hg and pulse is 72/min. BMI is 26 kg/m2. Pelvic examination reveals a 12-week-sized, nontender uterus and no adnexal masses or tenderness. Bedside ultrasound reveals a monochorionic diamniotic twin gestation with a single fundal placenta. This patient is at highest risk for which of the following complications?
CorrectIncorrect -
Question 39 of 40
39. Question
A 47-year-old man comes to the office for follow-up of hypertension. He reports increased fatigue, which he attributes to stress and describes as difficulty concentrating at work and lethargy during the day. The patient also has occasional palpitations. He has no chest pain, shortness of breath, syncope, or lower extremity edema. He takes chlorthalidone, amlodipine, and lisinopril, and the dose of lisinopril was increased during the last visit 4 weeks ago. The patient reports good medication adherence. He is a lifetime nonsmoker. He is single and lives alone. Blood pressure is 152/90 mm Hg and pulse is 68/min. BMI is 32 kg/m2. The lungs are clear on auscultation and heart sounds are normal. Laboratory results are as follows:
Hemoglobin
14.2 g/dL
Serum potassium
4.1 mEq/L
Serum creatinine
0.8 mg/dL
Urine protein
none
Echocardiogram shows left atrial enlargement and mild left ventricular hypertrophy. A short run of atrial fibrillation is revealed on 24-hour ECG monitoring. Further evaluation of this patient should initially focus on which of the following pathologies?
CorrectIncorrect -
Question 40 of 40
40. Question
A 75-year-old man comes to an urgent care clinic with his son after a ground-level fall. The patient reports, “I was playing with my grandchild when I tripped on the edge of the living room carpet and fell. I hit the right side of my head against the table.” He did not lose consciousness and has no headache, vomiting, blurry or double vision, weakness, or numbness. The patient has had no recent chest pain, palpitations, lightheadedness, or shortness of breath. Medical history is notable for hypertension, hyperlipidemia, coronary artery disease, and osteoarthritis. Current medications include aspirin, atorvastatin, carvedilol, clopidogrel, lisinopril, and acetaminophen as needed. He is a former smoker and does not use alcohol or illicit drugs. Blood pressure is 126/82 mm Hg, and pulse is 84/min and regular. The patient is alert, cooperative, and well oriented. There is a 2-cm laceration at the right parietal area with mild oozing. Neurological examination shows equal and reactive pupils and symmetric motor strength and sensation in the upper and lower extremities. There is no spine tenderness. Gait is steady. The scalp laceration is sutured and the bleeding stops. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect
