Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 3 items.
A 57-year-old man comes to the emergency department due to fever, chills, generalized weakness, dysuria, and increased urinary frequency for the past several days. He says he has “no energy” today and could not get out of bed. The patient has a history of schizophrenia and HIV. He does not remember his most recent CD4 cell count or the names of his current medications. The patient is a retired fishing boat captain, drinks 1 or 2 beers daily, and has smoked 2 packs of cigarettes daily for 38 years. Temperature is 38.3 C (101 F), blood pressure is 91/53 mm Hg, pulse is 122/min, and respirations are 20/min. Pulse oximetry shows 94% on room air. He is obese with weight of 80 kg, predicted body weight of 60 kg, and BMI of 32 kg/m2. The lungs are clear and there are no heart murmurs. The abdomen is soft and nontender. There is no peripheral edema. Laboratory results are as follows:
Complete blood count
Leukocytes
23,000/mm3
Hemoglobin
13.8 g/dL
Platelets
60,000/mm3
Serum chemistry
Sodium
131 mEq/L
Potassium
3.4 mEq/L
Chloride
96 mEq/L
Bicarbonate
14 mEq/L
Blood urea nitrogen
46 mg/dL
Creatinine
2.2 mg/dL
Urinalysis
Blood
moderate
Leukocyte esterase
positive
Nitrites
positive
Bacteria
many
White blood cells
50+/hpf
The patient is admitted and intravenous fluids and empiric antibiotics are administered. Three hours later, the patient becomes increasingly agitated, diaphoretic, and dyspneic. Repeat vital signs include a temperature of 37.6 C (99.7 F), blood pressure of 104/70 mm Hg, pulse of 116/min, and respirations of 42/min. Pulse oximetry shows 70% on 100% oxygen via nonrebreather mask. Lung examination reveals bilateral crackles. The remainder of the physical examination is unchanged. ECG shows sinus tachycardia. Chest x-ray reveals diffuse bilateral infiltrates.
Item 1 of 3
Which of the following is the most likely mechanism responsible for this patient’s current decompensation?
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 3
Endotracheal intubation is performed and the patient is mechanically ventilated. Several hours later, blood pressure is 123/80 mm Hg and pulse is 100/min. Ventilator settings are as follows: Fraction of inspired oxygen is 60%, tidal volume is 360 mL, positive end-expiratory pressure is 7 cm H2O, and respiratory rate is 16/min. The patient’s plateau pressure is 26 cm H2O. Arterial blood gases show pH is 7.37, PaO2 is 48 mm Hg, and PaCO2 is 38 mm Hg. Which of the following is the most appropriate next course of action?
CorrectIncorrect -
Question 3 of 40
3. Question
Item 3 of 3
The patient is maintained on mechanical ventilation, and his condition gradually improves over the next several days. Today, arterial blood gases show pH is 7.35, PaO2 is 94 mm Hg, and PaCO2 is 45 mm Hg, with fraction of inspired oxygen of 60%, positive end-expiratory pressure of 5 cm H2O, and tidal volume of 360 mL. Which of the following is the most appropriate course of action at present?
CorrectIncorrect -
Question 4 of 40
4. Question
A 22-year-old woman comes to the office for evaluation due to 9 months of amenorrhea. Since menarche at age 15, the patient has had a history of irregular menstrual cycles, previously occurring every 2-3 months. Menstrual periods were typically 2-3 days with light bleeding and no pain. She has no chronic medical issues and takes no medications. The patient, a professional ballerina, is sexually active and was treated for a chlamydial infection 3 years ago. She does not use tobacco, alcohol, or illicit drugs. Blood pressure is 110/80 mm Hg and pulse is 58/min. Height is 155 cm (5 ft 1 in) and BMI is 18 kg/m2. Cardiopulmonary examination is normal. Breasts are Tanner stage 4 and have no palpable masses or nipple discharge. On pelvic examination, the vaginal epithelium appears thin with few rugae, and the cervix has a closed, nulliparous os; no lesions; and no cervical discharge. Bimanual examination shows a mobile uterus and small, nontender ovaries. Urine pregnancy test is negative. Laboratory results are as follows:
FSH
2 mIU/mL
LH
2 mIU/mL
Prolactin, serum
20 ng/mL
Testosterone, serum
20 ng/dL
TSH
1.3 µU/mL
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 5 of 40
5. Question
An 11-day-old boy is brought to the office by his parents for concern of poor weight gain. The infant is breastfed exclusively and feeds every 1.5 hours during the day and every 2-3 hours overnight. The parents are unsure of how often he is voiding because he has 8-10 soft or runny bowel movements a day. His only medication is a daily vitamin D supplement. The infant was delivered vaginally following uncomplicated labor at 39 weeks gestation. Maternal prenatal laboratory results were unremarkable. Birth weight was 3.2 kg (7 lb 1 oz). Weight on day 6 of life was 3 kg (6 lb 10 oz). Weight today is 3.2 kg (7 lb 1oz). Physical examination shows a crying but easily consoled infant with jaundice of the face. The anterior fontanelle is open and flat, and the mouth appears moist. He has a strong suck and cry. The abdomen is soft, nondistended, and nontender. The mother tearfully says, “I don’t feel like he is getting enough milk because he seems to want to eat constantly. Sometimes I’ll nurse him for 20 minutes and then he cries and wants to nurse again. The most he sleeps is for 2-3 hours between feeds.” Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
An 85-year-old man is evaluated for fatigue. Three weeks ago, his wife passed away from a massive intracranial hemorrhage. Since then, the patient has been feeling sad and lonely and is unable to fall asleep at night. He feels fatigued during the day and sometimes does not want to “do anything.” The patient has no suicidal ideation. He states, “Everyone has to go someday; I have to put my life back together and work on improving my overall health.” His closest family member is his son, who lives 300 miles away. Since his wife passed away, the patient has lived alone but is considering moving into an assisted living facility. Medical history is notable for hypertension, hyperlipidemia, vitamin B12 deficiency, chronic low back pain, and mild chronic kidney disease. Current medications include valsartan, hydrochlorothiazide, pravastatin, aspirin, and a vitamin B12 supplement. The patient also takes acetaminophen intermittently for chronic back pain. He does not use tobacco, alcohol, or illicit drugs. Blood pressure is 146/70 mm Hg and pulse is 72/min. Examination of the neck shows no enlargement of the thyroid. The hands show periarticular bony enlargement at the proximal and distal interphalangeal joints. Laboratory tests show a normal complete blood count. Serum creatinine is 1.37 mg/dL. Serum TSH is 6.2 µU/mL. Repeat TSH is 6.3 µU/mL and free T4 is 1.23 ng/dL (normal: 0.9-1.7). Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 28-year-old woman comes to the office for medical evaluation prior to starting work as a radiology technician. The patient has no symptoms or medical problems and takes no medications. She has had no fever, night sweats, cough, anorexia, or weight loss and has no known exposure to a person with tuberculosis. The patient immigrated to the United States from India 7 years ago and had a negative tuberculin skin test at that time. She has received all recommended vaccinations, including Bacillus Calmette-Guérin (BCG) vaccine, as part of childhood immunization. She does not use tobacco, alcohol, or illicit drugs. Vital signs are within normal limits, and physical examination shows no abnormalities. Interferon-gamma release assay (IGRA) is positive.
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
Item 2 of 2
A subsequent chest radiograph reveals a discrete fibrotic scar in the right upper lobe with no airspace opacification, lymphadenopathy, or pleural effusion. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 38-year-old man comes to the office due to increasing depression over the past 2 months. The patient describes having very low energy, sleeping 12 hours a day, and lacking motivation and interest. He is worried about his end-of-year performance review because he has been unable to concentrate during meetings and has missed several project deadlines. The patient describes 2 previous episodes of depression. The first, at age 21, was severe and led to his taking a leave of absence from college for a year. The second, at age 35, responded rapidly to sertraline within a few days, but he stopped the medication after a week due to difficulty sleeping. The patient also reports having a “nervous breakdown” at age 27 shortly after being laid off from his job; he recalls that during this period, “I wasn’t sleeping at all and thought that I was God’s messenger.” He wrote lengthy letters to the Pope and called multiple priests at nearby churches to inform them. The patient states that his symptoms resolved after a few weeks. Physical examination shows no abnormalities. Mental status examination demonstrates a depressed mood, psychomotor retardation, and a logical thought process. There is no evidence of suicidal ideation, delusions, or hallucinations. Results of basic laboratory studies are normal. He is willing to try pharmacotherapy and requests sertraline because it helped his depression in the past. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
A 61-year-old woman comes to the emergency department due to fever, chills, and left flank pain that began abruptly last evening. A month ago, the patient was treated for a urinary tract infection with a short course of ciprofloxacin. She otherwise has no medical problems and currently takes no medications. The patient has no history of hospitalizations or surgeries. Temperature is 39.4 C (103 F), blood pressure is 80/40 mm Hg, pulse is 120/min, and respirations are 24/min. Pulse oximetry shows 94% on room air. Mucous membranes are dry and jugular veins are flat. Cardiopulmonary auscultation reveals clear lung fields and normal heart sounds without murmurs. The abdomen is soft and nontender. Left costovertebral angle tenderness is present. Skin examination is normal. Extremities are warm with no edema. Neurologic examination is within normal limits. Laboratory results are as follows:
Complete blood count
Hemoglobin
13 g/dL
Platelets
140,000/mm3
Leukocytes
17,000/mm3
Neutrophils
80%
Lymphocytes
8%
Bands
12%
Serum chemistry
Creatinine
1.4 mg/dL
Coagulation studies
INR
1.3
Activated PTT
41 sec
Plasma fibrinogen
163 mg/dL
Urinalysis
Leukocyte esterase
positive
Nitrites
positive
Bacteria
many
Broad-spectrum antibiotics and intravenous fluids are initiated, and the patient is admitted to the intensive care unit. Enoxaparin is given for prophylaxis against deep vein thrombosis. On hospital day 2, urine and blood cultures are positive for Escherichia coli, and antibiotics are narrowed based on culture sensitivities. Repeat laboratory testing is similar to admission, except platelet count has dropped to 105,000/mm3. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 56-year-old man comes to the emergency department due to fever and worsening headache and facial pain. The patient has had nasal congestion and sinus headache for the past several days. He was prescribed oral amoxicillin-clavulanate by his primary care physician 2 days ago, but his symptoms continued to worsen. He has a history of acute myeloid leukemia treated with hematopoietic stem cell transplant. The patient was briefly admitted 6 weeks ago for graft-versus-host disease. Temperature is 38.9 C (102 F), blood pressure is 118/60 mm Hg, and pulse is 110/min. Physical examination shows right periorbital swelling, mild proptosis of the right eye, and erythema of the facial skin overlying the right maxillary sinus. Thin, blood-tinged discharge is present in both nares, and percussion of the maxillary sinuses elicits pain. There is an area of decreased sensation over the right cheek. CT scan reveals opacification and bony erosions of the right maxillary sinus. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 12 of 40
12. Question
A 3 year-old boy with sickle cell disease is brought to the emergency department due to abdominal pain. The patient’s mother says that her son “seems so exhausted, refuses to eat or drink anything, and won’t stop crying from the pain.” The boy first developed a “tummy-ache” yesterday, but the pain worsened significantly this morning. He has also had 2 episodes of nonbloody, nonbilious emesis but no diarrhea. His last stool was 3 days ago. The mother gave him 2 doses each of ibuprofen and oxycodone this morning, with no significant improvement. She is not sure if the boy’s father administered any other medications. Medical history is significant for multiple prior hospitalizations for vaso-occlusive pain crises in the back and legs. However, the patient has no history of severe abdominal pain. Baseline hemoglobin is 9.8 g/dL. He is given penicillin twice daily, and his immunizations are up to date. Temperature is 36.7 C (98 F), blood pressure is 70/30 mm Hg, pulse is 162/min, and respirations are 36/min. Examination shows a sleepy young boy lying on a stretcher with significant abdominal tenderness to palpation, particularly over the left side of the abdomen. A spleen tip is palpated in the left lower quadrant. Laboratory results are as follows:
Hemoglobin
5.3 g/dL
Hematocrit
16.6%
Reticulocytes
12%
Platelets
120,000/mm3
Leukocytes
13,000/mm3
Which of the following is the most appropriate immediate step in management of this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
A 37-year-old woman, gravida 2 para 2, comes to the office 2 weeks after an uncomplicated vaginal delivery. The patient says, “I’m so lucky to have such a beautiful and healthy baby,” and then looks down and starts crying. She says, “I was so happy when I got pregnant, but now I feel overwhelmed and can’t manage. I’m exhausted all the time. I barely have the energy to keep up with my toddler, and the new baby is so difficult and demanding. I can’t enjoy the baby or playing with my toddler anymore. Maybe I shouldn’t have had a second baby after all.” The patient wakes up frequently throughout the night to feed the baby. Despite feeling tired, she is unable to sleep in the daytime, even when the baby is napping. The patient has a decreased appetite and is losing weight. Vital signs are normal. Physical examination shows no abnormalities. On mental status examination, the patient is visibly fatigued and restless. She appears sad and is intermittently tearful throughout the interview. The patient has no suicidal ideation, hallucinations, or delusions. Which of the following factors is most useful for distinguishing major depressive disorder from a normal postpartum course?
CorrectIncorrect -
Question 14 of 40
14. Question
A 67-year-old man is evaluated prior to being discharged from the hospital. The patient came to the emergency department 2 days ago due to severe left eye pain, blurred vision, headache, nausea, and vomiting over several hours. The patient had no similar episodes previously and no prior medical problems. Ocular examination during the initial evaluation showed decreased visual acuity and conjunctival injection with circumcorneal prominence, and the left eye felt firmer to palpation than the right. The left pupil was mid-dilated and poorly reactive to light. The patient subsequently received appropriate treatment under the guidance of an ophthalmologist, and his symptoms significantly improved during the hospital stay. In addition to careful ophthalmology follow-up, which of the following is the most appropriate advice for this patient at this time?
CorrectIncorrect -
Question 15 of 40
15. Question
A 50-year-old man is brought to the emergency department due to an episode of syncope. The patient experienced a brief episode of palpitations and lightheadedness yesterday evening, which he attributed to a tiring day at work. Today, while eating breakfast with his wife, he suddenly slumped to the table and lost consciousness for several minutes. He has had no abnormal bowel movements or urinary incontinence. By the time emergency medical personnel arrived, he was awake and alert. The patient has had no chest pains or shortness of breath, but he has been having headaches and malaise for the past several days. His wife adds that about a month ago, he had a bright red rash on the right calf for a week. The patient says he had a full medical evaluation 6 months ago when he turned 50 and was told that he is in perfect health. He takes no medication and does not use tobacco, alcohol, or illicit drugs. The patient works in a veterinary clinic and says he likes animals and nature. He recently took a bird-watching trip to Maine. Temperature is 36.8 C (98.2 F), pulse is 46/min, blood pressure is 130/70 mm Hg, and respirations are 14/min. Physical examination shows moist mucous membranes and normal jugular venous pressure. The lungs are clear to auscultation and heart sounds are normal with no murmur. The extremities are warm and without edema. Neurologic examination is normal. No skin rashes are present. Laboratory results are as follows:
Complete blood count
Leukocytes
9,800/mm3
Hemoglobin
14.4 g/dL
Platelets
280,000/mm3
Serum chemistry
Sodium
142 mEq/L
Potassium
4.2 mEq/L
Creatinine
0.8 mg/dL
Glucose
105 mg/dL
ECG shows sinus rhythm with 2:1 atrioventricular block. Which of the following should be a component of treatment for this patient’s arrhythmia?
CorrectIncorrect -
Question 16 of 40
16. Question
A 76-year-old man with a history of idiopathic pulmonary fibrosis is brought to the emergency department due to worsening shortness of breath for the past 2 days. He was diagnosed with pulmonary fibrosis 4 years ago after a lung biopsy and has been taking chronic oxygen therapy for the past several years. Over the past year he has had 5 hospital admissions for acute exacerbations, including 2 that required endotracheal intubation and mechanical ventilation. During his most recent hospitalization 3 weeks ago, he specified that he would not want to be intubated or resuscitated in the future. He lives at home with his wife and had been doing well until 2 days ago when his shortness of breath worsened and his oxygen requirement increased from 3 L/min to 6 L/min by nasal cannula. In the emergency department, the patient is lethargic and unable to participate in conversation. He appears uncomfortable from respiratory distress. Temperature is 36.7 C (98 F), blood pressure is 140/90 mm Hg, pulse is 120/min, and respirations are 40/min. The patient’s pulse oximetry shows 82% while breathing 100% oxygen via the nonrebreather mask. Physical examination shows shallow breathing with accessory muscle use. There are diffuse crackles in bilateral lungs. Chest x-ray shows bilateral reticular opacities, which are unchanged from previous x-ray. The patient’s wife says she does not want him to suffer any more. Which of the following is the most appropriate next step in management of this patient’s respiratory distress?
CorrectIncorrect -
Question 17 of 40
17. Question
A 73-year-old woman is brought to the emergency department from an assisted living facility due to abdominal pain, diarrhea, and fever. The patient’s symptoms began 24 hours ago with abdominal cramping and discomfort, which then progressed to frequent watery, brown bowel movements. She also has had fever with progressively worsening abdominal pain. Medical history includes hypertension, hypothyroidism, and knee osteoarthritis. The patient recently underwent a tooth extraction and completed a 7-day course of oral clindamycin for a dental infection. She does not use tobacco, alcohol, or illicit drugs. She is allergic to penicillin, which causes skin rash. Temperature is 39.1 C (102.4 F), blood pressure is 105/60 mm Hg, pulse is 110/min, and respirations are 19/min. BMI is 19 kg/m2. The patient is frail and ill appearing. Physical examination shows dry mucous membranes. Auscultation of the heart and lungs is normal. Bowel sounds are hypoactive, and moderate abdominal distension is present. The abdomen is diffusely tender to palpation without guarding or rebound tenderness. Stool occult blood testing is negative. Laboratory results are as follows:
Complete blood count
Hemoglobin
12.4 g/dL
Platelets
440,000/mm3
Leukocytes
28,000/mm3
Serum chemistry
Sodium
142 mEq/L
Potassium
3.2 mEq/L
Chloride
104 mEq/L
Bicarbonate
18 mEq/L
Blood urea nitrogen
31 mg/dL
Creatinine
1.4 mg/dL
Stool samples are obtained for microbiologic testing, and intravenous fluids and empiric antibiotics are administered. Which of the following additional interventions is most appropriate in management of this patient?
CorrectIncorrect -
Question 18 of 40
18. Question
An 84-year-old man is evaluated in the intensive care unit due to fevers. The patient was admitted 5 days ago for an acute exacerbation of chronic obstructive pulmonary disease with respiratory failure and required endotracheal intubation. He remains intubated and on mechanical ventilation. He is receiving bronchodilators, corticosteroids, and intravenous cefepime. For the past 24 hours, the patient has had high-grade fevers. There is no diarrhea, change in urine color, or increased respiratory secretions. Medical history includes hypertension, severe pulmonary hypertension, and cor pulmonale. The patient appears ill and is lightly sedated. Temperature is 39.1 C (102.4 F), blood pressure is 100/60 mm Hg, and pulse is 102/min. There is no erythema around the central venous catheter site and no rash. Bilateral breath sounds are coarse. No new murmurs are present. Bowel sounds are decreased and the patient grimaces on abdominal palpation, but there is no rigidity. Stool occult blood is negative. He has 1+ pitting sacral edema. Laboratory results are as follows:
Complete blood count
Hemoglobin
9.8 g/dL
Platelets
105,000/mm3
Leukocytes
21,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
4 mEq/L
Blood urea nitrogen
22 mg/dL
Creatinine
1 mg/dL
Liver function studies
Total bilirubin
2.1 mg/dL
Alkaline phosphatase
220 U/L
Aspartate aminotransferase
62 U/L
Alanine aminotransferase
74 U/L
Lipase
32 U/L
Urinalysis
Blood
negative
Leukocyte esterase
negative
Leukocytes
1-2/hpf
Chest radiography demonstrates no new infiltrates or consolidation. CT scan of the abdomen is notable for a nonspecific bowel gas pattern and a distended gallbladder with wall thickening. There is mild pericholecystic fluid but no gallstones or biliary duct dilation. Blood cultures are obtained. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
A 21-year-old woman, gravida 1 para 0, at 35 weeks gestation comes to labor and delivery due to irregular contractions. She is not having any leakage of fluid or vaginal bleeding. Fetal movements are normal. The patient initiated prenatal care at 8 weeks gestation and has had an uncomplicated prenatal course. All prenatal laboratory results have been within normal limits except that she is a cystic fibrosis carrier; her partner is negative for cystic fibrosis. Fetal anatomy scan at 20 weeks gestation demonstrated no abnormalities, and fetal growth has been appropriate. The patient has a history of depression, for which she takes a selective serotonin reuptake inhibitor. She does not use alcohol, tobacco, or illicit drugs. Temperature is 36.7 C (98 F), blood pressure is 110/70 mm Hg, and pulse is 84/min. The abdomen is gravid and nontender, and there are no palpable contractions. Fundal height is appropriate. Cervical examination reveals a closed cervix with no effacement and −3 station. Bilateral lower extremities have minimal pedal edema. Nonstress test results are as follows:
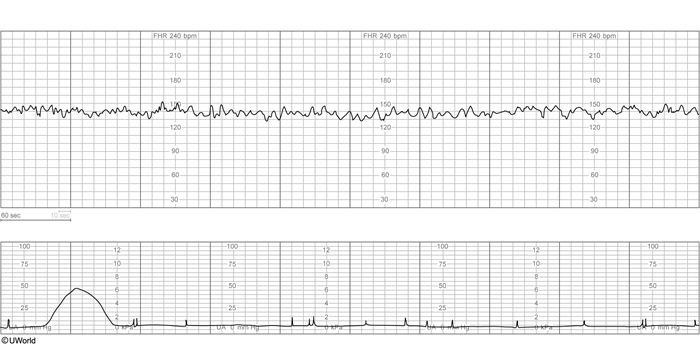
Over 40 minutes, fetal heart rate tracing remains unchanged. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 35-year-old woman comes to the office due to an 8-month history of pain and stiffness of her hand joints. The patient says, “I have had pain in my hands for several months, but now it seems like they hurt every day. I can hardly move them when I wake up in the morning, although by the time I get to work they loosen up enough for me to type at my computer. Ibuprofen helps the pain, but I am taking so much that it’s starting to bother my stomach.” She has had no pain in other joints, skin rash, chest pain, shortness of breath, or bluish discoloration of the fingers. Medical history includes allergic rhinitis that is well controlled with over-the-counter antihistamines. The patient does not use tobacco, alcohol, or illicit drugs. She is married and has 2 children. Temperature is 37.2 C (98.9 F), blood pressure is 130/80 mm Hg, and pulse is 76/min. Physical examination shows no oral mucosal lesions or cervical lymphadenopathy. The lungs are clear to auscultation and heart sounds are normal with no murmur. The abdomen is soft and nontender with no hepatosplenomegaly. There is mild swelling, erythema, and tenderness of several metacarpophalangeal and proximal interphalangeal joints of both hands. Blood cell counts, serum chemistries, and urinalysis are within normal limits. Other laboratory results are as follows:
C-reactive protein
12 mg/L (normal: <3 mg/L)
Anti-nuclear antibody
positive
Rheumatoid factor
negative
Anti-cyclic citrullinated peptide antibodies
positive
Human leukocyte antigen-B27
positive
Parvovirus IgM antibodies
negative
Parvovirus IgG antibodies
positive
Which of the following is the most appropriate response to this patient regarding her current condition?
CorrectIncorrect -
Question 21 of 40
21. Question
An 85-year-old woman is evaluated for constipation after being discharged from the hospital a week ago. The patient was hospitalized due to back pain and was found to have L3 and L4 vertebral osteomyelitis without evidence of cord compression; she is currently receiving intravenous antibiotics based on bone culture results. Other medical conditions include hypertension and chronic kidney disease with a baseline serum creatinine of 2.5 mg/dL. In addition to antibiotic therapy, the patient currently takes hydrocodone-acetaminophen every 6 hours, twice daily senna and docusate, and lisinopril. She eats a balanced diet. Vital signs are normal. Perianal sensation is intact. Rectal examination shows hard stool in the rectal vault but no impaction. Lower extremity neurologic examination shows no abnormalities. She reports back pain and rates it as 2 to 3 on a scale of 1-10 while on pain medication. What is the most appropriate next step in management for constipation?
CorrectIncorrect -
Question 22 of 40
22. Question
A 38-year-old woman, gravida 3 para 3, is evaluated for heavy vaginal bleeding following a spontaneous vaginal delivery. Labor was induced via oxytocin infusion at 38 weeks gestation for gestational hypertension. The patient delivered a 4167 g (9 lb 3 oz) healthy infant. Delivery of the placenta, assisted by traction on the umbilical cord and uterine massage, occurred 30 minutes later. Immediately after placental delivery, profuse vaginal bleeding and severe lower abdominal pain began. The patient had an uncomplicated prenatal course. Her first pregnancy ended at term with a cesarean delivery due to fetal heart rate abnormalities. Her second pregnancy ended with an uncomplicated term vaginal delivery. The patient has no chronic medical conditions. She takes a daily prenatal vitamin and did not use tobacco, alcohol, or illicit drugs during the pregnancy. Temperature is 36.7 C (98.1 F), blood pressure is 90/60 mm Hg, and pulse is 84/min. On pelvic examination, profuse vaginal bleeding is noticed. There is a smooth, round mass at the introitus. In addition to administering intravenous fluids, which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A newborn girl is evaluated on arrival in the hospital nursery. Three hours ago, she was born at home via spontaneous vaginal delivery due to precipitous labor. The umbilical cord was clamped in the ambulance, and intramuscular vitamin K and ophthalmic antibiotic prophylaxis were administered at the hospital. Temperature is 36.7 C (98.1 F), pulse is 120/min, and respirations are 24/min. On physical examination, the patient is awake, alert, and active. The head is normocephalic and the anterior fontanelle is open and flat. The pupils are equal and reactive to light and accommodation, extraocular movements are intact, and red reflexes are present bilaterally. The nares are patent without rhinorrhea and there is no cleft lip or palate. The clavicles are intact bilaterally without crepitus. S1 and S2 are normal without murmurs, and the lungs are clear to auscultation bilaterally. The abdomen is soft and nontender, with normal bowel sounds and no organomegaly. Peripheral and femoral pulses are normal and symmetrical, and capillary refill is normal. The skin is slightly ruddy, without rashes or lesions. Laboratory results for venous blood are as follows:
Complete blood count
Hemoglobin
19 g/dL
Hematocrit
66%
Platelets
240,000/mm3
Leukocytes
11,000/mm3
Liver function studies
Total bilirubin
2.3 mg/dL
Aspartate aminotransferase
37 U/L
Alanine aminotransferase
24 U/L
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
A 57-year-old woman is evaluated on the surgical floor for continuous bilious emesis over the last 12 hours. She has had 10 episodes of vomiting, which has continued despite intravenous antiemetic administration. The patient underwent a total abdominal hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and tumor debulking for epithelial ovarian cancer 4 days ago. During the procedure, 2 liters of ascites was drained. She ate solid food yesterday for lunch but is now unable to hold down even small sips of water. Her last bowel movement was prior to surgery and she has not passed flatus. The patient has type 2 diabetes mellitus controlled with diet, exercise, and metformin. She is married and has 3 children, all born via cesarean delivery. The patient does not use tobacco, alcohol, or illicit drugs. She has no known drug allergies. Temperature is 37.2 C (99 F), blood pressure is 134/74 mm Hg, and pulse is 78/min. BMI is 37 kg/m2. Physical examination shows a markedly distended abdomen with a vertical skin incision, and bowel sounds are absent. The incision is nontender to palpation, and the staples are clean and dry. Laboratory results are as follows:
Serum chemistry
Sodium
137 mEq/L
Potassium
2.9 mEq/L
Chloride
92 mEq/L
Bicarbonate
30 mEq/L
Blood urea nitrogen
26 mg/dL
Creatinine
1.2 mg/dL
Calcium
8.9mg/dL
Glucose
58 mg/dL
Abdominal x-ray reveals dilated loops of bowel with air in the distal colon and rectum. In addition to intravenous fluid administration, which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 71-year-old woman comes to the emergency department due to a week of fever, nonproductive cough, and shortness of breath. The patient states, “I have been healthy all my life but over the past year I have had 2 episodes of shingles, and I constantly feel tired. Maybe I am just getting old.” She has also had occasional loose stools, joint pains, and a 4.5-kg (10-lb) weight loss over the past year. She has had no chest pain, palpitations, abdominal pain, or melena. The patient takes no medications and recently received pneumococcal and zoster vaccinations. She drinks a glass of wine with dinner every evening and does not use tobacco or illicit drugs. The patient is widowed and lives alone but is socially active with her peers and frequently attends social gatherings. Temperature is 38 C (100.4 F), blood pressure is 130/60 mm Hg, pulse is 98/min, and respirations are 24/min. Pulse oximetry shows 90% on room air. BMI is 20 kg/m2. There are several enlarged lymph nodes in the cervical and inguinal regions and small white patches in her mouth. Lung auscultation reveals bilateral crackles, and heart sounds are normal with no murmur. The abdomen is soft and nontender with no hepatosplenomegaly. Bowel sounds are active. Neurological examination shows no abnormalities. There is no skin rash, extremity edema, or joint erythema or effusion. Laboratory results are as follows:
Complete blood count
Hemoglobin
11.4 g/dL
Mean corpuscular volume
88 µm³
Platelets
110,000/mm³
Leukocytes
3,800/mm³
Neutrophils
68%
Eosinophils
3%
Lymphocytes
22%
Monocytes
7%
Chest x-ray reveals bilateral interstitial infiltrates. Appropriate antimicrobial therapy is administered. Which of the following is the best next step in diagnosis of this patient?
CorrectIncorrect -
Question 26 of 40
26. Question
A 78-year-old woman is brought to the office by her daughter due to several days of increasing confusion and disorientation. Her daughter reports that the patient has been restless and confused, especially at night. The patient has been seen talking with people who are not in the room. Today, she was found frantically searching for clothing while saying, “I am late for work,” although she has been retired for 15 years. The patient has a history of hypertension, hyperlipidemia, and cerebral infarction without residual deficits. She also has mild memory deficits but independently performs activities of daily living. Two weeks ago, the patient was hospitalized for chest pain and was found to have chest wall shingles. She was started on antiviral therapy and amitriptyline for neuropathic pain. Her rash is now largely resolved, but she continues to take amitriptyline daily for the pain. Other medications include aspirin, lisinopril, and atorvastatin. The patient does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 140/70 mm Hg, pulse is 82/min, and respirations are 14/min. Oxygen saturation is 99% on ambient air. She is disoriented to time and place but recognizes her daughter. The patient remembers 0 out of 3 objects after 5 minutes. The remainder of the physical examination reveals no abnormalities. ECG shows normal sinus rhythm with nonspecific ST-T changes. Laboratory results are as follows:
Complete blood count
Hemoglobin
12.8 g/dL
Platelets
320,000/mm3
Leukocytes
9,200/mm3
Serum chemistry
Sodium
140 mEq/L
Potassium
4.2 mEq/L
Blood urea nitrogen
18 mg/dL
Creatinine
0.6 mg/dL
Glucose
102 mg/dL
Urinalysis
Blood
negative
Leukocyte esterase
negative
White blood cells
1-2/hpf
CT scan of the head demonstrates mild cortical atrophy. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
A 4-year-old boy is brought to the office due to difficulty stooling and stool leakage. He has a small, hard bowel movement every 4-5 days accompanied by straining and pain. He frequently complains of abdominal discomfort, which is partially relieved by defecation. The father says, “I am very embarrassed that he stools in his underwear 1 or 2 times a week, and that he seems to not care about the accidents or the fact that it makes him smell bad.” The symptoms began when the patient started preschool at age 3 and have worsened since then. Prior to this, he had normal soft bowel movements 1 or 2 times a day. Medical history is significant for an episode of otitis media at age 1, pneumonia at age 2, and occasional upper respiratory infections. Neither parent has a history of gastrointestinal disease, and the patient’s 1-year-old brother has normal bowel movements. The patient is up to date on immunizations, and developmental milestones are age-appropriate. Last year, his height and weight were at the 10th percentile; today, height is 100 cm (39.4 in, 25th percentile), weight is 15 kg (33 lb, 25th percentile), and BMI is 14.9 kg/m2. Physical examination reveals an alert and calm child. His neck is supple without lymphadenopathy. The abdomen is soft, nontender, and nondistended, but a mass is palpated in the left lower quadrant. Bowel sounds are normal, and the liver and spleen are not enlarged. Rectal sphincter tone is normal, and hard stool is palpated in the rectal vault. Which of the following is the most likely cause of the patient’s encopresis?
CorrectIncorrect -
Question 28 of 40
28. Question
A 14-year-old boy is brought to the clinic by his parents for his annual well-child check. The patient was identified with sickle cell trait during newborn screening, but otherwise he is well. He runs 3 miles daily and lifts weights 3 times a week. He says, “I want to try out for the junior varsity soccer team, but I heard that my cousins with sickle cell disease have been hospitalized frequently for severe pain.” The patient is performing well in school and is looking forward to starting high school in the fall. He takes no medications or supplements and does not use tobacco, alcohol, or illicit drugs. Family history is significant for sickle cell anemia in cousins on both sides but negative for heart disease, syncope, asthma, or sudden unexplained death. The patient’s blood pressure is 120/80 mm Hg and pulse is 60/min. Growth has been consistent along the 75th percentile for weight and height, and BMI is 23 kg/m2. Physical examination shows an alert, friendly, and well-nourished boy. Auscultation reveals regular rate and rhythm and no adventitious lung sounds. The abdomen is soft, nontender, and nondistended with no organomegaly. Brachial and femoral pulses are 2+ bilaterally. The patient has normal Tanner stage III external male genitalia. No jaundice or skin lesions are seen. Which of the following is the most appropriate advice for this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
A 42-year-old woman comes to the emergency department due to tremors and palpitations that began a few hours ago. Over the last month, the patient has had increasing anxiety and a 4.5-kg (10-lb) weight loss despite increased appetite. The patient has had no headaches, visual symptoms, or changes in bowel or urinary habits. She has no other chronic medical conditions and has had no previous surgeries. The patient has had irregular menses over the last 2 years; her last menstrual period was 4 months ago. She stopped oral contraceptives a year ago as she thought she was going through menopause. The patient has no known drug allergies. Temperature is 36.7 C (98.1 F), blood pressure is 146/84 mm Hg, and pulse is 110/min. BMI is 22 kg/m2. Physical examination shows warm, dry skin. The thyroid is enlarged symmetrically with no palpable masses. Cardiac examination reveals sinus tachycardia; there are no rubs or murmurs. The lungs are clear to auscultation bilaterally. Abdominal examination reveals a lower abdominal mass that extends from the pubic symphysis to the umbilicus; there is no rebound, guarding, or fluid wave. Examination of the bilateral upper extremities reveals a resting tremor. Deep tendon reflexes are intact. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 78-year-old woman comes to the office for an annual wellness visit. She has a history of bilateral knee osteoarthritis and lately the pain has been limiting her mobility. The patient has had no falls but feels weak most of the time and gets tired easily. She states, “Everything I do now requires an effort; maybe it’s just my age.” The patient has lost several pounds over the last year but has had no change in appetite. Medical history is also notable for hypertension, hyperlipidemia, hypothyroidism, and 2 episodes of pneumonia over the past year. The patient is up to date with recommended vaccinations and age-appropriate cancer screenings. She is a retired teacher and lives alone in her apartment; a home health aide spends several hours a day assisting her with shopping and household chores. The patient is independent in her basic activities of daily living and takes care of her own finances. Blood pressure is 146/82 mm Hg and pulse is 76/min and regular. The lungs are clear to auscultation and heart sounds are normal. The abdomen is soft and nontender. Knee examination shows mild bilateral joint line tenderness and crepitus but no erythema or effusion. Her handgrip is weak but symmetrical, and gait is slow. Neurologic examination is otherwise normal. Blood cell counts, serum chemistry, and TSH levels are normal. Geriatric depression screening is negative. Her analgesics are optimized. Which of the following interventions is most likely to decrease the risk of adverse health outcomes in this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 56-year-old man is evaluated for generalized weakness on the second day of hospitalization. The patient has a history of heavy alcohol use and poor nutrition since his wife died 6 months ago, and he has lost 6.8 kg (15 lb) over this period. He was admitted due to nausea, vomiting, and abdominal pain. In the emergency department, physical examination revealed dry mucous membranes and epigastric tenderness, and laboratory studies showed serum sodium of 128 mEq/L, serum amylase of 220 U/L, and positive urinary ketones. The patient was treated with thiamine, analgesics, antiemetics, and intravenous saline with dextrose, which improved his symptoms. However, the patient now has difficulty getting out of bed and feels “weak all over.” He also has shortness of breath and a pins-and-needles sensation in the extremities. Temperature is 37.1 C (98.8 F), blood pressure is 110/60 mm Hg, pulse is 92/min, and respirations are 26/min. Pulse oximetry is 96% on ambient air. The lungs are clear on auscultation but breathing is shallow. Heart sounds are normal with no murmurs. The abdomen is soft and nondistended; the epigastric tenderness has improved since the previous examination. Motor strength is 3/5 in all major muscle groups, and deep tendon reflexes are diffusely diminished. No tremors or asterixis is present. Immediate serum chemistry testing shows sodium of 132 mEq/L and potassium of 3.4 mEq/L. Which of the following is the most likely cause of this patient’s current symptoms?
CorrectIncorrect -
Question 32 of 40
32. Question
A 25-year-old nulligravid woman comes to the emergency department because of left lower quadrant pain. The patient has no fevers, chills, nausea, vomiting, dysuria, hematuria, or vaginal bleeding. The pain is moderately controlled with ibuprofen. The patient has no chronic medical conditions or previous surgeries. Her only medications are a daily multivitamin and ibuprofen occasionally. Her last menstrual period was 2 weeks ago; menses are regular and last 4-5 days. The patient uses condoms for contraception and has no history of sexually transmitted infections. Her grandmother died of breast cancer at age 68, and her mother, diagnosed with ovarian cancer at age 60, tested negative for BRCA mutations. Temperature is 36.7 C (98.1 F), blood pressure is 110/80 mm Hg, and pulse is 68/min. BMI is 24 kg/m2. Abdominal examination shows tenderness of the left lower quadrant but no rebound, guarding, or organomegaly. Pelvic examination reveals an anteverted, small, nontender uterus. The left adnexum is mobile, mildly tender, and enlarged. Urine pregnancy test is negative. Transvaginal ultrasound reveals a 4-cm, left adnexal mass that is simple and unilocular with normal Doppler blood flow. Despite assurances that the cyst appears benign, the patient asks how she can reduce her risk for ovarian cancer. Which of the following is the best recommendation for ovarian cancer prevention in this patient?
CorrectIncorrect -
Question 33 of 40
33. Question
A 38-year-old woman, gravida 1 para 0, at 34 weeks gestation comes to the emergency department as she has not felt fetal movement for the last 18 hours. The patient has had no contractions, vaginal bleeding, or leakage of fluid. Her pregnancy has been complicated by fetal growth restriction diagnosed at 28 weeks, when ultrasound revealed an estimated fetal weight at the third percentile. Since then, the patient has been followed with serial biophysical profiles and umbilical artery Doppler sonography, which have been normal. She has no chronic medical conditions and has had no surgeries. She takes a prenatal vitamin and a stool softener daily. The patient does not use tobacco, alcohol, or illicit drugs. She has no known drug allergies. She is a preschool teacher and exercises for 20-30 minutes each day after school. Temperature is 36.7 C (98 F), blood pressure is 110/60 mm Hg, and pulse is 88/min. The cervix is closed and posterior. Fetal heart tones are not heard on Doppler ultrasound. Bedside ultrasound reveals no fetal cardiac activity. Blood type is A, Rh negative. Kleihauer-Betke test is negative. The patient is informed about the intrauterine fetal demise. The patient asks if there are any risks associated with waiting for the onset of labor. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 34 of 40
34. Question
A 21-year-old man comes to the office after an episode of lightheadedness. He is a runner and has been training intensely for the last several months. During one of his morning running sessions last week, he experienced lightheadedness and felt he was going to pass out. The patient had to stop and sit on the ground until this feeling subsided. He has not had any symptoms since then and attributes this episode to “pushing myself too much,” but his trainer insisted that he see a doctor. The patient has no chest pain or shortness of breath. He is a lifetime nonsmoker. He does not use performance-enhancing drugs. The patient is adopted and cannot provide any relevant biological history. Supine blood pressure is 133/78 mm Hg, standing blood pressure is 130/75 mm Hg, and pulse is 60/min. There is no jugular venous distension. Cardiac auscultation reveals no murmurs. Pulses are full and symmetric bilaterally. ECG shows sinus rhythm with increased voltage of QRS complexes, 0.5-mm downsloping ST-segment depression, and symmetric T-wave inversion in leads V4-V6. What is the best next step in management of this patient?
CorrectIncorrect -
Question 35 of 40
35. Question
The following vignette applies to the next 2 items.
A 7-year-old girl is brought to the office due to worsening ear pain. The girl developed left ear pain 2 days ago, but her father is concerned because “there was a yellow stain on her pillow this morning.” The patient received acetaminophen this morning for pain, but her father says, “She was so uncomfortable that I could not clean her ears with a cotton swab, which I normally help her with after she showers.” The patient has no fever, cough, rhinorrhea, or sore throat. She had 3 episodes of acute otitis media from age 2-4. Immunizations are up to date, and her only daily medication is a multivitamin. Temperature is 37.8 C (100 F), blood pressure is 100/60 mm Hg, pulse is 92/min, and respirations are 14/min. Physical examination shows a nervous-appearing girl who winces with any attempt to examine her left ear. Dried yellow discharge is noted posterior to the tragus. The patient starts to cry when her auricle is pulled back for otoscopy. Yellow discharge and erythema are seen in the ear canal. The tympanic membrane is partially obscured by drainage, but the visible portion is translucent and pearly gray in color, with a light reflex. There is no swelling or tenderness to palpation of the skin surrounding the ear. Examination of the right ear reveals a normal-appearing canal and tympanic membrane.
Item 1 of 2
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 36 of 40
36. Question
Item 2 of 2
The diagnosis is discussed with the father, and appropriate therapy is prescribed. Which of the following is the most likely etiology for this patient’s presentation?
CorrectIncorrect -
Question 37 of 40
37. Question
A 24-year-old man comes to the office due to depression and fatigue for the past month. He says, “I have had no energy. I sleep at least 12 hours a day, but I wake up tired and force myself to get out of bed. I’m barely getting by at work—I just sit and stare at my computer screen and can’t concentrate.” The patient has no history of depression. He was hospitalized a few years ago for agitation and psychosis. At that time, the patient believed that he was a messenger from God and had a solution for climate change that would save the world. He was sleeping 1-2 hours a night and talking so rapidly that he was difficult to understand. The patient does not remember which medications he was prescribed and did not follow up after discharge. He does not use recreational substances. Family history is significant for depression in his mother, whose condition responded well to amitriptyline, and a history of schizophrenia in a maternal cousin. Vital signs are normal. BMI is 32 kg/m2. Physical examination shows no abnormalities. On mental status examination, the patient speaks slowly and softly. Mood is “depressed” and affect is dysthymic. He has no hallucinations or delusions. The patient wishes he could go to sleep and not wake up but has no thoughts of killing himself. Complete blood count, serum chemistry, and thyroid function tests are within normal limits. Urine drug screen is negative. Which of the following is the most appropriate pharmacotherapy?
CorrectIncorrect -
Question 38 of 40
38. Question
A 32-year-old man is brought to the emergency department after threatening to kill himself in response to hearing voices. On arrival, he is extremely frightened and agitated. He screams, “They are trying to replace my brain,” and strikes a nurse trying to assist him. The patient reports having command auditory hallucinations of multiple voices telling him to stab himself with a kitchen knife. He receives several doses of risperidone to help calm him down and is admitted to the psychiatry unit. Medical evaluation, including urine toxicology, is noncontributory. Records show that the patient has a diagnosis of schizophrenia and has been treated with olanzapine in the past with good results; however, he frequently drops out of treatment. Medical history is significant for asthma and an episode of pneumonia 3 months earlier. The patient is started on olanzapine 10 mg, which is subsequently increased to 20 mg. After 2 weeks, he is significantly calmer; the voices have decreased in frequency and intensity and are no longer of a command nature. He denies any suicidal or homicidal ideation and is discharged to attend a day program with instructions to continue the medication. At 3-month follow-up, the patient is no longer hearing voices. He attends the day program 3 days a week and reports being adherent to his medication. Which of the following tests should be obtained?
CorrectIncorrect -
Question 39 of 40
39. Question
A 70-year-old man with chronic obstructive pulmonary disease is brought to the hospital due to shortness of breath, dry cough, and wheezing. The symptoms began 6 hours ago and have progressively worsened. He has had 2 admissions in the past year for similar symptoms and both times also had atrial fibrillation with rapid ventricular response. The patient has smoked 2 packs of cigarettes daily for 40 years. In the emergency department, he is initiated on noninvasive positive pressure ventilation due to increased work of breathing. Temperature is 37.2 C (99 F), blood pressure is 121/60 mm Hg, pulse is 125/min, and respirations are 24/min. The patient’s pulse oximetry shows 92% on 40% fraction of inspired oxygen. Pulmonary examination reveals diffuse wheezing throughout the lung fields and prolonged expiration. Heart sounds are distant and irregular. There is 1+ pretibial edema bilaterally. Chest x-ray reveals hyperinflation with no pulmonary infiltrates. The patient is treated with intravenous corticosteroids and antibiotics as well as inhaled albuterol. Diltiazem infusion is administered for atrial fibrillation. Six hours later, his work of breathing is improved, and he is transitioned to nasal cannula oxygen. On repeat examination, the patient has bilateral face and neck swelling, and palpation reveals crepitus. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 64-year-old man comes to the office due to worsening urinary symptoms. For the past year, he has had difficulty initiating urination, a weak urinary stream, and increased urinary frequency. The patient wakes up 1 or 2 times a night to urinate. He has had no dysuria, hematuria, or abdominal pain. Medical history is notable for hypertension and diet-controlled type 2 diabetes mellitus. The patient is a former smoker with a 20 pack-year history, and he drinks 1 or 2 alcoholic beverages each evening. Family history is negative for cancer. Temperature is 36.7 C (98 F), blood pressure is 128/72 mm Hg, and pulse is 80/min. BMI is 30 kg/m2. The lungs are clear to auscultation, and heart sounds are normal. The abdomen is nondistended, soft, and nontender. There is no costovertebral angle tenderness. External genitalia appear normal. Perineal and lower extremity sensory examination is normal. Rectal examination shows normal rectal tone with a symmetrically enlarged, nontender prostate with a smooth surface. Four weeks ago, routine laboratory results showed a hemoglobin A1c of 7% and serum creatinine of 0.9 mg/dL. Which of the following is the most appropriate next step in management of this patient’s urinary symptoms?
CorrectIncorrect
