Time limit: 0
Quiz Summary
0 of 35 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 35 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 35
1. Question
A 34-year-old woman, gravida 3 para 3, comes to the office 2 weeks after a spontaneous vaginal delivery for evaluation of urinary leakage. Since delivery, the patient has had leaking of urine in small amounts 5-6 times daily. She sometimes does not feel the urge to urinate despite a good appetite and frequent hydration. The patient has no dysuria or hematuria. She has no chronic medical conditions and has had no surgeries. Temperature is 98.8 F (37.1 C), blood pressure is 124/78 mm Hg, and pulse is 86/min. The uterus is firm, nontender, and extends 2 fingerbreadths above the pubic symphysis. There is urethral leakage of urine with Valsalva maneuver, but no urine in the vaginal vault. A postvoid residual is normal. The perineum is intact and there is scant lochia. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 2 of 35
2. Question
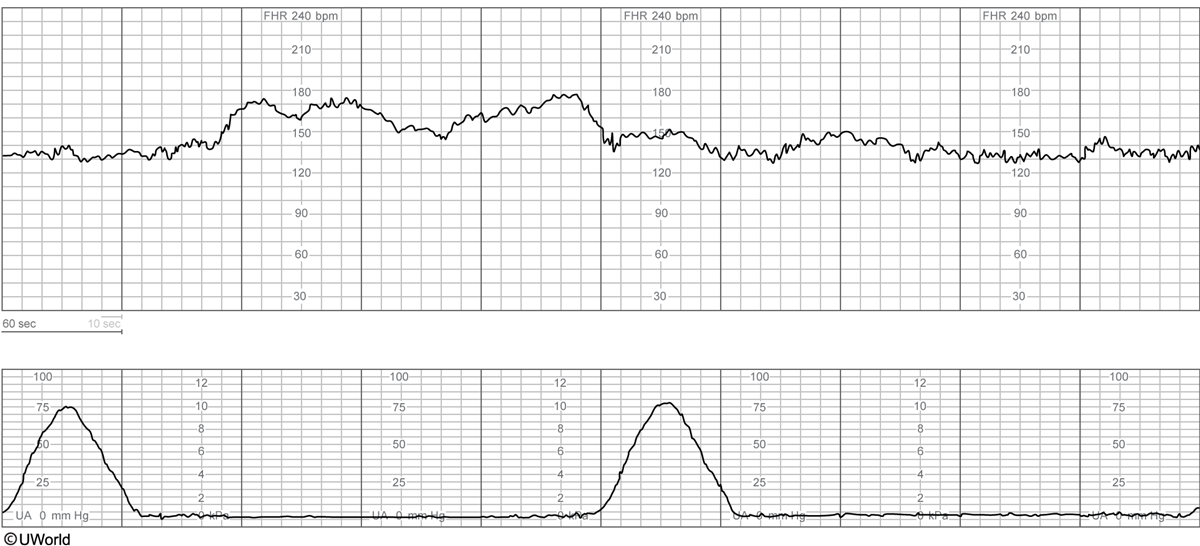
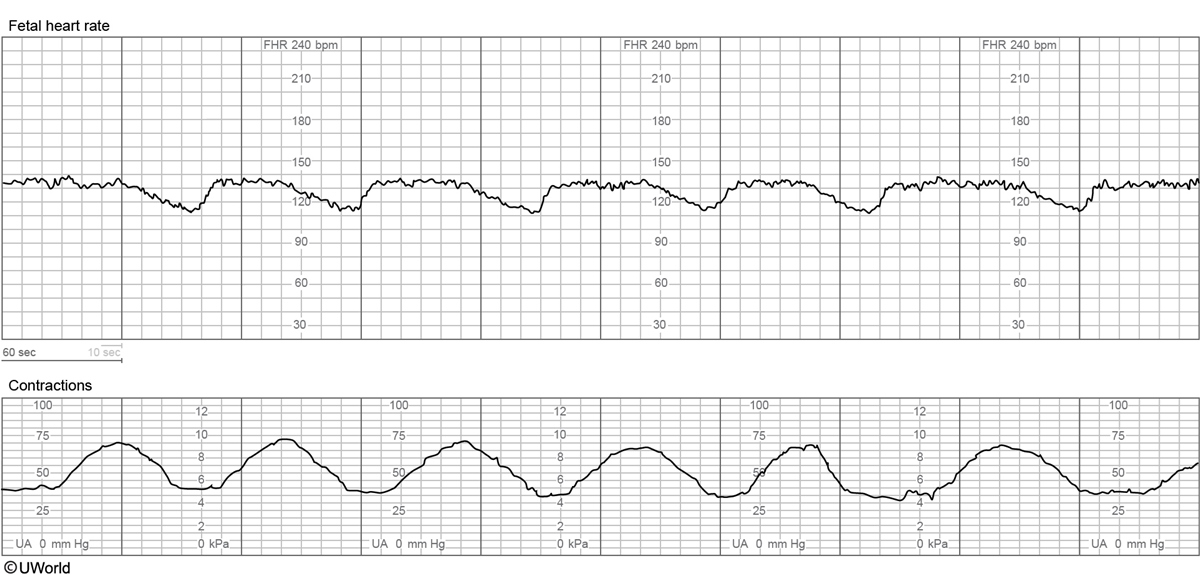
A 38-year-old woman, gravida 3 para 2, at 37 weeks gestation comes to the labor and delivery unit due to contractions. The contractions started this morning and now are painful and occur every 5 minutes. The patient has had no leakage of fluid or vaginal bleeding. Fetal movement is normal. Previous pregnancies ended in uncomplicated term vaginal deliveries. The patient has HIV that was diagnosed at her first prenatal visit during this pregnancy. Viral load 1 week ago was 12,300 copies/mL. She does not always take her combination antiretroviral medications but takes a daily prenatal vitamin. Blood pressure is 132/86 mm Hg and pulse is 98/min. The patient is tolerating labor well, and the uterus is soft and nontender between contractions. The fetal heart rate tracing is shown in the exhibit. The cervix is 4 cm dilated and 100% effaced, and the fetal vertex is at 0 station. The amniotic sac is tense and palpable. In addition to starting zidovudine, which of the following is the best next step in management of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 3 of 35
3. Question
A 28-year-old woman, gravida 2 para 1, at 24 weeks gestation comes to the office for a routine prenatal visit. She has had increasing shortness of breath but no cough or chest pain. The patient has had no vaginal bleeding, leakage of fluid, or contractions. Fetal movement is normal. She has no chronic medical conditions, and her only prior surgery is a cesarean delivery with her first pregnancy. The patient had a fetal anatomy ultrasound at 18 weeks gestation, but not all structures were well visualized. Blood pressure is 116/70 mm Hg and pulse is 68/min. Fundal height is 32 cm. Ultrasound reveals an amniotic fluid index of 40 cm (normal: 8-24 cm). The fetus is in breech presentation and has an estimated fetal size consistent with 24 weeks gestation. An isolated tracheoesophageal fistula is visualized. The placenta is located posteriorly. This patient is at increased risk for which of the following obstetric complications?
CorrectIncorrect -
Question 4 of 35
4. Question
A 42-year-old woman comes to the emergency department for severe lower abdominal pain. The pain started several hours ago and has progressively worsened. She has associated nausea and vomiting but no fever, diarrhea, or abnormal vaginal discharge. The patient was diagnosed with adenomyosis last month due to increasingly heavy menses and dysmenorrhea and is currently taking tranexamic acid as needed. Her menses started yesterday, but she reports that the pain is more severe than usual and radiates to the left lower quadrant. Temperature is 37.8 C (100 F), blood pressure is 110/74 mm Hg, and pulse is 110/min. The abdomen is soft with normoactive bowel sounds, and there is voluntary guarding in the left lower quadrant. On pelvic examination, the uterus is globular and boggy, and there is dark red blood with small clots in the vagina. The left adnexa is tender on bimanual examination, and there are no palpable adnexal masses. Urine pregnancy testing is negative. Hemoglobin is 11 g/dL. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 5 of 35
5. Question
A 36-year-old woman, gravida 1 para 0, at 38 weeks gestation comes to the hospital due to increased leakage of fluid. She reports spontaneous rupture of membranes approximately 48 hours earlier, and contractions started 12 hours after rupture. She reports intermittent vaginal spotting and regular fetal movement. The patient was attempting a home birth but came to the hospital because her cervix has been 6 cm dilated for the past 5 hours. Temperature is 39.4 C (103 F), blood pressure is 120/80 mm Hg, and pulse is 108/min. Digital examination reveals the cervix to be 6 cm dilated and 70% effaced, with the fetal vertex at 0 station. The fetal heart tracing is shown in the exhibit. Which of the following is most likely responsible for the findings on this patient’s fetal monitoring?
 CorrectIncorrect
CorrectIncorrect -
Question 6 of 35
6. Question
A 30-year-old woman, gravida 3 para 1 aborta 1, at 26 weeks gestation comes to the office for evaluation of increased vaginal discharge that started yesterday. She now changes her pad every hour and has noticed some spotting. Her initial prenatal visit was 2 weeks ago, and laboratory evaluation revealed a positive urine culture. The patient has not started her antibiotics because she has no symptoms. Her last delivery was 2 years ago via term cesarean delivery for recurrent late fetal decelerations. Vital signs are normal. The abdomen is soft, and the uterus is nontender. On speculum examination, there is pooling of clear, nitrazine-positive fluid in the vagina; the cervix is visibly closed. Fetal heart rate tracing shows a baseline of 150/min, accelerations, and no decelerations. There are irregular contractions on tocodynamometry. Transabdominal ultrasound shows an anterior placenta and an amniotic fluid index of 3 cm. Which of the following most likely contributed to this patient’s presentation?
CorrectIncorrect -
Question 7 of 35
7. Question
A 38-year-old woman, gravida 1 aborta 1, comes to the office for follow-up a week after suction curettage. The patient initially presented 7 weeks after her last menstrual period for an initial prenatal appointment. At that time, she had breast tenderness but no abdominal pain, nausea, or vaginal bleeding. During that visit, ultrasound revealed an empty gestational sac. β-hCG level was 53,256 IU/L. The patient returned a week later and a repeat ultrasound confirmed a missed abortion. Suction curettage was performed and the pathological specimen from the procedure indicated a diagnosis of hydatidiform mole. Today, the patient has minimal bleeding but no pain, fevers, chills, or abnormal vaginal discharge. Blood pressure is 110/80 mm Hg and weight is 55 kg (121.3 lb). Pelvic examination shows minimal dark red blood in the vaginal vault and no active bleeding. On bimanual examination, the uterus is small and nontender. No adnexal masses are palpable. β-hCG level is 1,412 IU/L. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 8 of 35
8. Question
A 26-year-old woman comes to the emergency department due to a bump on her vaginal introitus. The patient first noticed the mass 2 days ago, but it has increased in size and now causes discomfort when she walks or exercises. She had unprotected sex with a new partner 6 weeks ago and has had 10 lifetime partners. The patient had an abnormal Pap test last year but had a normal colposcopy. She smokes a half pack of cigarettes daily but does not use alcohol or illicit drugs. Temperature is 36.7 C (98.1 F), blood pressure is 110/60 mm Hg, and pulse is 80/min. On pelvic examination, the pubic hair is shaved. There is a 4-cm, mobile, soft, nontender cystic mass behind the right posterior labium majus that extends into the vagina. The remainder of the examination is normal. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 9 of 35
9. Question
A 29-year-old woman, gravida 1 para 0, at 30 weeks gestation comes to the office for a routine prenatal visit. For the past week, the patient has had increasing pruritus that has been most severe on her palms. She has tried using oatmeal baths and lotion, but the itching has continued. The patient also has had nausea and difficulty sleeping due to pruritus and increasing back pain. She takes diphenhydramine and acetaminophen nightly to help her sleep. The patient has chronic hypertension that has been well controlled during the pregnancy. Blood pressure is 138/86 mm Hg and pulse is 76/min. Fundal height is 30 cm. Fetal heart rate is 150/min. Multiple excoriations are noted on the abdomen and thighs. The remainder of the examination is normal. Laboratory results are as follows:
Liver function studies
Total protein
4.5 g/dL
Alkaline phosphatase
170 U/L (normal during pregnancy: 38-229)
Aspartate aminotransferase (SGOT)
66 U/L
Alanine aminotransferase (SGPT)
74 U/L
Total bile acids
26 µmol/L (normal: <10)
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 10 of 35
10. Question
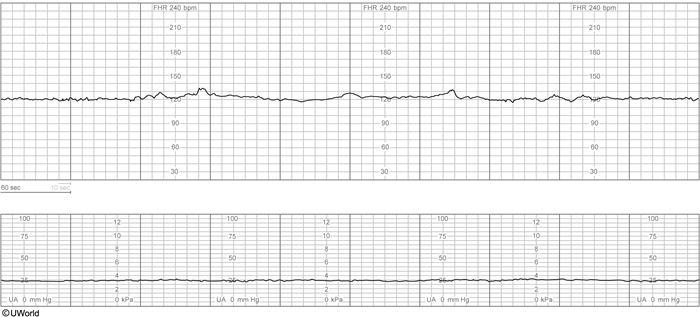
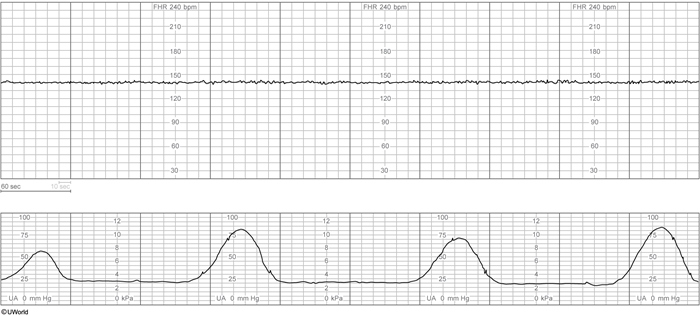
A 29-year-old woman, gravida 1 para 0, at 34 weeks gestation comes to the office for a routine prenatal visit. She has had no contractions, vaginal bleeding, or leakage of fluid. Fetal movement is normal. The patient has systemic lupus erythematosus with positive anti-Ro/SSA antibodies but has had no flares during this pregnancy. Her medications include hydroxychloroquine, low-dose aspirin, and a prenatal vitamin. Blood pressure is 130/88 mm Hg and pulse is 65/min. Fundal height is 33 cm. The remainder of the physical examination is unremarkable. Urine dipstick has trace protein. A nonstress test is performed for 10 minutes; results are shown in the exhibit. Which of the following is the most likely etiology for this patient’s fetal heart rate tracing?
 CorrectIncorrect
CorrectIncorrect -
Question 11 of 35
11. Question
A 33-year-old woman, gravida 1 para 0, at 39 weeks gestation comes to the hospital for a scheduled elective induction. She has had no contractions, vaginal bleeding, or leakage of fluid. Fetal movement is normal. Her pregnancy has been uncomplicated except for a positive group B Streptococcus (GBS) rectovaginal culture at 36 weeks gestation with resistance to erythromycin. The patient has no chronic medical conditions and has had no prior surgeries. She developed a nonpruritic maculopapular rash after taking penicillin in her 20s. Vital signs are normal. Abdomen is soft, gravid, and nontender. The cervix is 1 cm dilated and 60% effaced with the fetal vertex at -2 station. Fetal heart rate tracing is category 1. Given this patient’s penicillin allergy, which of the following is the most appropriate pharmacotherapy for this patient?
CorrectIncorrect -
Question 12 of 35
12. Question
A 21-year-old woman is evaluated for nausea, vomiting, and a severe headache. The patient developed a headache last night after getting out of bed and walking to the newborn nursery. Her headache has not improved with acetaminophen or ibuprofen, and the only thing that makes it better is lying down and sleeping. Now she has a severe headache, nausea, and vomiting whenever she gets out of bed. The patient has had no dizziness, changes in vision, or loss of consciousness. She had a spontaneous vaginal delivery 2 days ago after an induction of labor for gestational hypertension. She had an epidural placed for analgesia that was removed immediately after delivery. Temperature is 37.2 C (99 F), blood pressure is 136/88 mm Hg, and pulse is 108/min. The patient has neck stiffness and is unable to sit up due to severe nausea. There is no papilledema, and the pupils are equal and reactive. Bilateral lower extremities have pitting edema to the knees. Deep tendon reflexes are 2+. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 13 of 35
13. Question
A 42-year-old woman comes to the office after a positive home pregnancy test. The patient has a history of irregular menses and had a positive home pregnancy test after she went 6 months without a menstrual period. Her medical conditions include chronic hypertension, for which she takes multiple medications, and type 2 diabetes mellitus, for which she stopped taking metformin a few months ago due to side effects. BMI is 38 kg/m2. Temperature is 37.6 C (100 F), blood pressure is 138/88 mm Hg, and pulse is 90/min. The abdomen is soft and without rebound or guarding. The uterus is nontender and fundal height measures 24 cm. Ultrasound findings show a singleton fetus at 24 weeks gestation with bilateral small, underdeveloped kidneys and a bladder with minimal urine. The amniotic fluid index is 4 cm (normal: >5 cm). Which of the following is the most likely cause of this fetal presentation?
CorrectIncorrect -
Question 14 of 35
14. Question
A 36-year-old primigravid woman at 34 weeks gestation arrives at the emergency department after being found unresponsive on the floor by her husband. She was found unconscious about 30 minutes ago and became gradually responsive over a few minutes. The husband reports the patient has had increasing nausea and vomiting over the past few hours and a severe frontal headache. Currently she has no symptoms other than the headache. Medical history is significant for migraines, and the patient takes no daily medications. Temperature is 36.7 C (98.1 F), blood pressure is 138/98 mm Hg, pulse is 78/min, and respirations are 20/min. Cranial nerves are intact, and the neck is supple. Funduscopic examination is normal. The lungs are clear to auscultation bilaterally. Cardiac examination demonstrates normal heart sounds. The abdomen is nontender, and the uterine fundus measures 34 weeks gestation. There is minimal pretibial edema, and deep tendon reflexes are 3+. Motor examination is normal. Laboratory results are as follows:
Complete blood count
Hemoglobin
13.8 g/dL
Platelets
360,000/mm3
Leukocytes
11,000/mm3
Serum chemistry
Sodium
132 mEq/L
Potassium
3.8 mEq/L
Chloride
100 mEq/L
Bicarbonate
22 mEq/L
Creatinine
1.1 mg/dL
Glucose
80 mg/dL
Liver function studies
Alkaline phosphatase
180 U/L (normal: 38-229)
Aspartate aminotransferase (SGOT)
12 U/L
Alanine aminotransferase (SGPT)
24 U/L
Urinalysis
Protein
1+
Blood
negative
Glucose
negative
Ketones
present
Urine drug screen is negative. CT scan of the head reveals bilateral frontal lobe edema but no mass lesions or bleeding. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 15 of 35
15. Question
A 34-year-old woman, gravida 3 para 2, at 33 weeks gestation comes to the emergency department due to continued leakage of fluid. The patient reports intermittent vaginal spotting but has had no contractions. Fetal movement is normal. Her prenatal course has been complicated by group B Streptococcus bacteriuria treated in the first trimester. The patient has no other chronic medical conditions or previous surgeries. Temperature is 39.2 C (102.5 F), blood pressure is 90/56 mm Hg, and pulse is 109/min. Fundal height measures 30 cm. Speculum examination shows pooled fluid in the posterior fornix that turns nitrazine paper blue; the cervix appears visibly closed. A ferning pattern is visualized on microscopy. Fetal heart monitoring shows a rate of 170/min with moderate variability. Tocometry shows no contractions. A transabdominal ultrasound reveals a fetus in transverse lie; the single deepest vertical pocket of amniotic fluid is 1 cm. Which of the following is an indication for delivery in this patient?
CorrectIncorrect -
Question 16 of 35
16. Question
A 29-year-old woman, gravida 1 para 0, at 12 weeks gestation comes to the office for prenatal care. The patient was hospitalized at 7 weeks gestation for hyperemesis gravidarum. Since the hospitalization, she has received intravenous hydration several times in the emergency department due to dehydration from persistent nausea and vomiting. Despite taking antiemetics frequently, the patient is unable to eat or drink much. She is able to tolerate prenatal vitamins, which she takes with metoclopramide. Blood pressure is 90/50 mm Hg. Prepregnancy BMI was 18 kg/m2. Weight is 50 kg (110.2 lb), a decrease of 2 kg (4.4 lb) from her prepregnancy weight. Fetal heart tones are normal by Doppler. The patient is concerned about her weight loss and whether it will affect the baby. This patient is at greatest risk for which of the following pregnancy complications?
CorrectIncorrect -
Question 17 of 35
17. Question
A 34-year-old woman, gravida 3 para 2, at 35 weeks gestation is evaluated in the labor and delivery unit due to increasing mucoid vaginal bleeding and contractions. The patient has been undergoing induction of labor for fetal growth restriction due to chronic hypertension. Pelvic examination an hour ago showed the cervix to be 6 cm dilated and 100% effaced after spontaneous rupture of membranes. Since then, the patient has developed increasing bloody discharge with some clots. Contractions have also increased in intensity and frequency. Group B Streptococcus rectovaginal culture performed last week was negative. Temperature is 37.2 C (99 F), blood pressure is 150/90 mm Hg, and pulse is 78/min. Fetal heart rate tracing shows a baseline of 120/min, moderate variability, multiple early decelerations, and no accelerations. Contractions occur every 2 minutes. The cervix is 8 cm dilated and 100% effaced with a moderate amount of mucus and blood on examination. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 18 of 35
18. Question
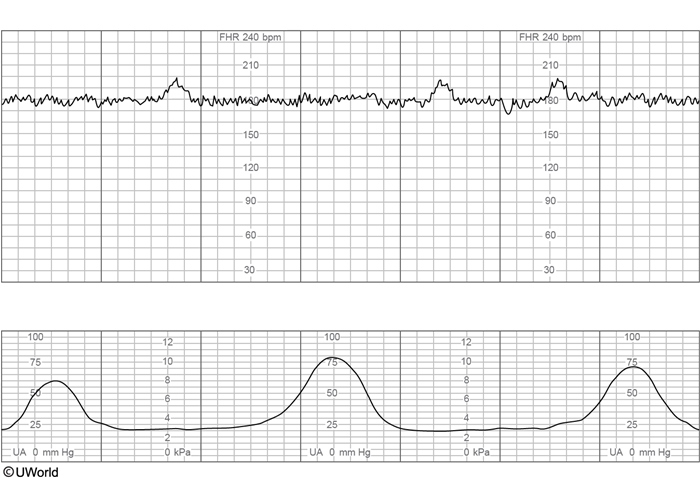
A 28-year-old woman, gravida 2 para 1, at 38 weeks gestation is admitted to labor and delivery due to prelabor rupture of membranes. Clear amniotic fluid has been leaking continuously for the last 2 hours. The patient has irregular, nonpainful contractions and no vaginal bleeding. Prenatal care during this pregnancy has been uncomplicated, and the patient’s previous pregnancy ended in a term vaginal delivery. Temperature is 36.7 C (98.1 F), blood pressure is 120/70 mm Hg, and pulse is 78/min. The cervix is 3 cm dilated and 50% effaced with the fetal vertex at −2 station. Fetal heart tracing on admission is as seen in the exhibit.
After an oxytocin infusion is started for labor augmentation, the patient begins to have regular, painful contractions that require epidural anesthesia. Two hours later, temperature is 37.2 C (99 F), blood pressure is 120/80 mm Hg, and pulse is 80/min. On repeat examination the cervix is now 7 cm dilated, 100% effaced, with the fetal vertex at +1 station; and current fetal heart tracing is as seen in the exhibit. Which of the following is the best next step in management of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 19 of 35
19. Question
A 30 year-old-woman, gravida 1 para 0, at 29 weeks gestation comes to the office for a routine prenatal visit. She reports increasing fatigue, shortness of breath with exertion, and bilateral leg swelling over the past few weeks. The patient has had no vaginal bleeding, contractions, or leakage of fluid. Fetal movement is normal. Her initial prenatal visit was at 10 weeks gestation, and results of a complete blood count at that time were as follows:
Hemoglobin
11.8 g/dL
Platelets
240,000/mm3
Leukocytes
8,000/mm3
Today, blood pressure is 124/84 mm Hg, pulse is 77/min, and respirations are 22/min. Cardiac examination is normal, and the lungs are clear to auscultation bilaterally. Fundal height is 29 cm and fetal heart rate is 160/min. Bilateral lower extremities have 2+ pitting edema up to the knees. Results of a complete blood count today are as follows:
Hemoglobin
11.2 g/dL
Platelets
118,000/mm3
Leukocytes
8,200/mm3
Third-trimester HIV and syphilis tests are negative. Which of the following is the most appropriate management of this patient?
CorrectIncorrect -
Question 20 of 35
20. Question
A 37-year-old woman, gravida 4 para 0 aborta 3, comes to the labor and delivery department with painful contractions. She has had no prenatal care this pregnancy, but states she is at 37 weeks gestation based on a first-trimester ultrasound performed in the emergency department. The patient has had 3 elective pregnancy terminations with dilation and curettage. On physical examination, the cervix is 6 cm dilated and 90% effaced with the fetal head at +1 station. She dilates quickly to 10 cm and vaginally delivers a 4.5-kg (10-lb) male infant. Following delivery of the infant, the umbilical cord avulses from the placenta, necessitating manual extraction. The placenta is extracted in pieces, and the patient suddenly develops profuse vaginal bleeding. The uterus is firm, and the bleeding is unresponsive to uterine massage and uterotonic medications. Which of the following is the most likely cause of this patient’s bleeding?
CorrectIncorrect -
Question 21 of 35
21. Question
A 27-year-old woman, gravida 2 para 1, at 40 weeks gestation has a forceps-assisted vaginal delivery after pushing for 2 hours. She was diagnosed with preeclampsia with severe features on admission and is receiving a magnesium sulfate infusion. Her first pregnancy ended with a cesarean delivery at 39 weeks gestation for breech presentation. Temperature is 37.2 C (99 F), blood pressure is 150/100 mm Hg, and pulse is 112/min. Ten minutes after delivery, the placenta delivers with gentle traction, and the patient develops profuse vaginal bleeding. Bimanual massage reveals a firm, nontender uterus with the fundus at the level of the umbilicus. Pelvic examination shows a right vaginal sidewall defect. There is minimal bleeding from the cervical os, and the perineum is intact. Which of the following is the most likely cause of this patient’s bleeding?
CorrectIncorrect -
Question 22 of 35
22. Question
A 36-year-old woman, gravida 3 para 2, at 35 weeks gestation comes to the emergency department due to leakage of fluid and painless vaginal bleeding. The patient had rupture of membranes 30 minutes ago; the fluid was initially clear but became bloody a few minutes later. She had normal fetal movement earlier today. The patient has not received prenatal care this pregnancy; her 2 previous pregnancies resulted in term cesarean deliveries. She has hypertension but stopped taking her medication when she became pregnant. Temperature is 36.1 C (97 F), blood pressure is 140/96 mm Hg, and pulse is 92/min. The uterus is nontender. Speculum examination confirms rupture of membranes; the cervical os is 1 cm dilated with minimal vaginal bleeding. Doppler ultrasound is unable to detect fetal heart tones. Which of the following is the most likely cause of this patient’s presentation?
CorrectIncorrect -
Question 23 of 35
23. Question
A 23-year-old woman, gravida 1 para 1, is evaluated on the postpartum floor due to increased perineal pain. The patient underwent a spontaneous vaginal delivery 8 hours ago after pushing for 3 hours. She had a second-degree perineal laceration repaired immediately after delivery. For the past 30 minutes, the patient has had increasing perineal pain, particularly with voiding. Temperature is 37.4 C (99.3 F), blood pressure is 132/86 mm Hg, and pulse is 90/min. On abdominal examination, there is no rebound or guarding and the uterus is firm and palpable below the umbilicus. The patient’s pad contains a small amount of dark red blood, and no clots are expressed with uterine massage. The perineum and labia majora are edematous. The laceration repair appears intact with no purulent drainage but is tender to palpation. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 24 of 35
24. Question
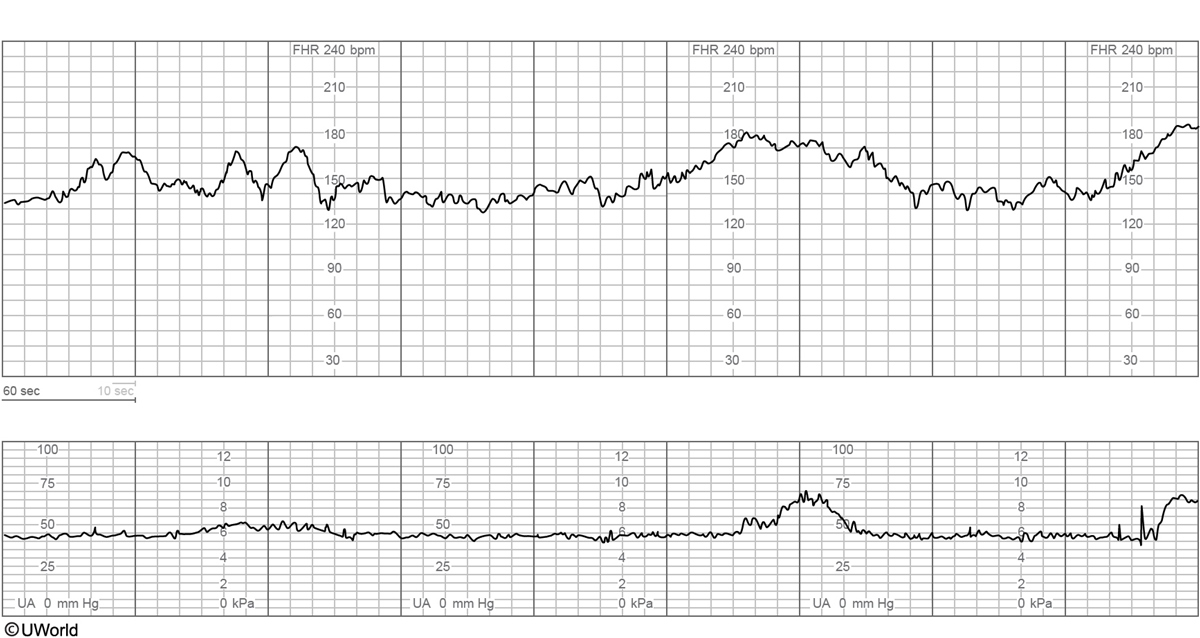
A 34-year-old woman comes to the labor and delivery unit via ambulance for contractions, rupture of membranes, and vaginal bleeding. The patient had rupture of membranes 4 hours ago, and her contractions have increased in intensity and frequency over the last hour, which required multiple doses of morphine in the ambulance. On arrival, temperature is 37.2 C (99 F), blood pressure is 130/80 mm Hg, and pulse is 94/min. On pelvic examination, the membranes are grossly ruptured with clear fluid, and there is scant, dark blood on the perineum. The cervix is 6 cm dilated and 80% effaced, and fetal position is occiput posterior. Fetal heart rate tracing is shown in the exhibit. Which of the following is the most likely cause of this fetal heart rate tracing?
 CorrectIncorrect
CorrectIncorrect -
Question 25 of 35
25. Question
A 2-hour-old boy is evaluated in the delivery room for minimal right arm movement. He was born at 37 weeks gestation by vacuum-assisted, vaginal delivery to a 39-year-old woman who had excessive weight gain during pregnancy. The delivery was complicated by a 3-minute shoulder dystocia. Birth weight was 4.6 kg (10.1 lb). Examination shows a small area of edema in the scalp that does not cross suture lines. The right upper extremity is held in adduction and internal rotation with the elbow extended, forearm pronated, and wrist and fingers flexed. Moro and biceps reflexes are absent in the right arm. The remainder of the examination is normal. Which of the following is the most appropriate next step in management of this patient’s condition?
CorrectIncorrect -
Question 26 of 35
26. Question
A 29-year-old woman, gravida 2 para 1, at 12 weeks gestation comes to the office for an initial prenatal visit. The patient has had no nausea, abdominal pain, or vaginal bleeding. Her first pregnancy ended in an operative vaginal delivery after induction of labor at 42 weeks gestation. She has no chronic medical conditions and has had no surgeries. The patient takes a daily prenatal vitamin and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 118/74 mm Hg and pulse is 76/min. BMI is 27 kg/m2. The uterine fundus is 2 cm below the umbilicus. Pelvic examination is normal. Ultrasound shows an intrauterine 12-week twin gestation with 2 posterior-fundal placentas. The fetal heart rates are normal. Compared to patients with singleton gestations, this patient is at increased risk for which of the following obstetric-related complications?
CorrectIncorrect -
Question 27 of 35
27. Question
A 25-year-old woman, gravida 1 para 0, at 24 weeks gestation comes to labor and delivery due to decreased fetal movement. The patient has felt decreased fetal movement for the past day and no fetal movement in the past hour. She has had no contractions, vaginal bleeding, or leakage of fluid. Last week, the patient went to a picnic and the next day she had nausea, watery diarrhea, and muscle aches, but no rashes or joint pain. Her symptoms resolved after 24 hours. She has no chronic medical conditions and takes no daily medications. Temperature is 98.9 F (37.2 C), blood pressure is 118/68 mm Hg, and pulse is 90/min. Cardiopulmonary examination is normal. There is no flank pain and the uterus is nontender. On pelvic examination, the cervix is closed, and membranes are intact. No fetal heart tones are detected on Doppler, and a transabdominal ultrasound confirms an intrauterine fetal demise. Which of the following pathogens is the most likely cause of this patient’s presentation?
CorrectIncorrect -
Question 28 of 35
28. Question
A 27-year-old woman, gravida 1 para 1, comes to the office for evaluation of postpartum bleeding. Four days ago, the patient had a forceps-assisted vaginal delivery due to recurrent fetal decelerations. She had a third-degree perineal laceration that was repaired, and she went home on the second postpartum day. Since delivery, the patient has had continuous, dark red vaginal bleeding with small clots, requiring her to change a menstrual pad 6 to 7 times daily. She has no chest pain, shortness of breath, or orthostasis. Temperature is 99.5 F (37.5 C), blood pressure is 124/76 mm Hg, and pulse is 88/min. BMI is 33 kg/m2. The uterine fundus is firm, nontender, and palpable at 4 cm below the umbilicus. The perineal laceration repair is intact, and the cervix is 1 cm dilated with minimal dark red blood in the vagina. Laboratory results are as follows:
Hemoglobin
10 g/dL
Platelets
140,000/mm3
Leukocytes
11,000/mm3
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 29 of 35
29. Question
A 20-year-old woman, gravida 1 para 0, at 36 weeks gestation is brought to the emergency department by her mother due to a seizure. The patient was sitting outside when she suddenly had a 2-minute seizure with loss of urinary continence. She is still confused when she arrives in the emergency department. Her mother reports that the patient has had increasing anxiety and has been acting out for the past several days. Her only surgery was a splenectomy after a motor vehicle collision last year. Temperature is 37.7 C (99.9 F), blood pressure is 158/98 mm Hg, and pulse is 120/min. The patient is agitated and diaphoretic. The pupils are dilated bilaterally. The cranial nerves are intact. The neck is supple and nontender. Cardiopulmonary examination is normal. The abdomen is gravid without rebound or guarding, and the uterus is nontender. There is 2+ pitting pedal edema bilaterally. Sensation and strength are normal in the bilateral upper and lower extremities. Laboratory results are as follows:
Complete blood count
Hematocrit
33%
Platelets
140,000/mm3
Leukocytes
13,000/mm3
Serum chemistry
Sodium
124 mEq/L
Potassium
3.4 mEq/L
Chloride
96 mEq/L
Bicarbonate
21 mEq/L
Blood urea nitrogen
18 mg/dL
Creatinine
0.8 mg/dL
Glucose
80 mg/dL
Urinalysis
Protein
none
Ketones
present
CT scan of the head is normal. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 30 of 35
30. Question
A 30-year-old woman, gravida 1 para 0, at 24 weeks gestation comes to the office for a prenatal visit. The patient feels well and has no vaginal bleeding, leakage of fluid, or contractions. She has had no headaches, changes in vision, or right upper quadrant pain. The patient has no chronic medical conditions and has had an uncomplicated pregnancy. She does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 152/88 mm Hg, pulse is 72/min, and respirations are 14/min. Oxygen saturation is 99% on room air. Physical examination is normal. Fetal heart rate is 150/min on Doppler ultrasound. Laboratory results are as follows:
Complete blood count
Hematocrit
30%
Platelets
280,000/mm3
Serum chemistry
Creatinine
0.6 mg/dL
Aspartate aminotransferase (SGPT)
17 U/L
Alanine aminotransferase (SGOT)
24 U/L
Urinalysis
Protein
1+
A nonstress test is reactive. Repeat blood pressure is 154/86 mm Hg. Which of the following is the best next step in management of this patient’s hypertension?
CorrectIncorrect -
Question 31 of 35
31. Question
A 37-year-old woman, gravida 2 para 1, comes to the emergency department due to painful contractions and leakage of fluid. She has not received prenatal care during this pregnancy and is at 24 weeks gestation by a sure, regular last menstrual period. The patient has no chronic medical conditions. She precipitously delivers a male fetus with no cardiac activity. Examination of the fetus shows edematous, peeling skin. The scalp is edematous, but the palate appears normal and there are no dysmorphic facial features. The fetal abdomen is tense and fluid-filled. The placenta appears thickened and edematous. Maternal laboratory results are as follows:
Hemoglobin
11.2 g/dL
Blood type
O, Rh negative
Indirect Coombs test
negative
HIV-1 antibody
negative
Which of the following is the most likely etiology of this patient’s fetal demise?
CorrectIncorrect -
Question 32 of 35
32. Question
A 23-year-old woman, gravida 2 para 1, at 37 weeks gestation comes to the labor and delivery unit due to contractions and leakage of fluid for the last 8 hours. She had routine prenatal care until 20 weeks gestation but has not had an appointment since moving across the country. Her prior pregnancy was a term vaginal delivery complicated by intraamniotic infection. Her infant spent 3 weeks in the neonatal intensive care unit for early-onset neonatal sepsis. Temperature is 37.5 C (99.5 F), blood pressure is 120/80 mm Hg, and pulse is 84/min. The patient has grossly ruptured membranes with clear fluid, and the cervix is 3 cm dilated and 30% effaced with the fetal vertex at −1 station. Leukocyte count is 13,000/mm3, hematocrit is 33%, and platelets are 189,000/mm3. Which of following is the indication for intrapartum group B Streptococcus (GBS) prophylaxis in this patient?
CorrectIncorrect -
Question 33 of 35
33. Question
A 29-year-old woman, gravida 1 para 1, is evaluated due to recurrent fevers on day 5 after a cesarean delivery for arrest of descent after a prolonged induction of labor. Gentamicin and clindamycin were administered for fever on postoperative day 1. Ampicillin was added on postoperative day 3 as the patient continued to be intermittently febrile. She has had no nausea, vomiting, hemoptysis, dyspnea, hematuria, dysuria, or diarrhea. Temperature is 39 C (102.2 F), blood pressure is 120/80 mm Hg, and pulse is 108/min. Oxygen saturation is 98% on room air. The lungs are clear to auscultation bilaterally. Breast examination shows full, slightly tender breasts with no erythema. Abdominal examination shows mild bilateral lower quadrant tenderness to deep palpation and an incision with minimal serosanguineous drainage but no erythema or induration. Pelvic examination reveals a nontender uterine fundus that is below the umbilicus. Examination of the lower extremities shows no swelling, tenderness, or erythema. Hemoglobin is 10.8 g/dL. Urinalysis is normal. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 34 of 35
34. Question
A 43-year-old woman comes to the office for a routine health maintenance examination. She has no concerns today. The patient recently had a normal screening mammogram. She has type 1 diabetes mellitus and her last hemoglobin A1c level was 7.6%. The patient had an abnormal Pap test at age 35 that required cervical conization, but all subsequent Pap tests have been normal. She is currently sexually active and has had no pain with intercourse. Her last menstrual period was 2 weeks ago. The patient does not use tobacco, alcohol, or recreational drugs. Vital signs are normal. BMI is 26 kg/m2. Pelvic examination is shown in the exhibit. Which of the following is the most likely diagnosis in this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 35 of 35
35. Question
A 27-year-old woman at 8 weeks gestation comes to the office for her first prenatal visit. This is her first pregnancy; it was unplanned. The patient lives alone and works part-time as a restaurant server. She has a 5-year history of intravenous heroin use and says, “I’ve tried to quit before, but it was so hard. I know drugs are bad for the baby, so I want to try again.” The patient uses heroin daily. Her last injection was 6 hours ago. She has no other chronic medical conditions and no known drug allergies. Temperature is 37.2 C (99 F), blood pressure is 126/80 mm Hg, and pulse is 88/min. Physical examination is notable only for needle marks on the patient’s extremities. Transvaginal ultrasonography reveals an intrauterine gestation and a heart rate of 150/min. Which of the following is the best next step in management of this patient?
CorrectIncorrect
