Time limit: 0
Quiz Summary
0 of 37 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 37 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 37
1. Question
A 52-year-old woman undergoes laparoscopic cholecystectomy due to recurrent episodes of biliary colic. During the surgery, a blunt trocar is inserted near the umbilicus under direct vision (ie, open technique), and pneumoperitoneum is achieved via insufflation of the abdomen with carbon dioxide. Three additional trocars are inserted, and the cholecystectomy is completed uneventfully. After a period of observation in the postanesthesia care unit, the patient is discharged home. Three days later, the patient returns to the emergency department due to persistent abdominal pain and nausea. She takes acetaminophen and hydrocodone every 6 hours. Temperature is 38 C (100.4 F), blood pressure is 120/68 mm Hg, and pulse is 104/min. Physical examination shows intact port incisions with no erythema or discharge. There is mild generalized tenderness of the abdomen with some guarding. Bowel sounds are diminished. The remainder of the examination is normal. Laboratory testing shows leukocytes at 16,000/mm3; serum electrolytes and bilirubin are normal. Abdominal x-ray reveals generalized distension of the small and large bowel, stool in the distal colon, and intraperitoneal free air. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 2 of 37
2. Question
A 78-year-old woman is brought to the emergency department due to sudden-onset, right-sided hemiplegia and right-sided facial droop. Medical history is significant for chronic kidney disease and hypertension. The patient has a history of medication nonadherence and does not remember the names of her prescribed medications. Temperature is 37 C (98.6 F), blood pressure is 218/128 mm Hg, pulse is 84/min, and respirations are 15/min. On examination, the patient is mildly lethargic but able to converse. Cranial nerve examination shows upper-motor-neuron, right-sided facial weakness. Muscle strength is 0/5 in the right upper and lower extremities. CT scan of the head, immediately performed, is shown in the exhibit. Laboratory results are as follows:

Complete blood count
Hemoglobin
10.4 g/dL
Platelets
240,000/mm3
Serum chemistry
Blood urea nitrogen
32 mg/dL
Creatinine
2.1 mg/dL
Coagulation studies
INR
1.1
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 3 of 37
3. Question
A 20-year-old hockey player is brought to the emergency department 30 minutes after falling headfirst into the hockey rink boards. He did not lose consciousness during the impact but was unable to move his arms and legs afterward. The patient was placed in a rigid cervical collar and transported to the hospital on a backboard; 2 large-bore intravenous catheters were inserted en route. On arrival, blood pressure is 128/78 mm Hg, pulse is 102/min, and respirations are 14/min. The patient is alert and appears anxious. Cardiopulmonary examination is normal. Neurologic examination shows intact cranial nerves. Pinprick and temperature sensation are absent below the level of the clavicles; vibratory sense is intact. The patient is still unable to move his extremities. CT scan of the cervical spine reveals a burst fracture of C5 with impingement of posteriorly displaced fragments on the spinal cord. Neurosurgery is consulted. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 4 of 37
4. Question
A 20-year-old man comes to the emergency department due to worsening right leg pain. The patient runs 5 miles daily, but several weeks ago, he began having dull pain at the right lower shin during runs. Now, the pain occurs even with light walking. He has had no trauma, fever, chills, or redness in the affected area. The patient has no prior medical conditions and takes no medications. Temperature is 36.7 C (98.1 F), blood pressure is 110/60 mm Hg, pulse is 56/min, and respirations are 16/min. BMI is 17 kg/m2. Physical examination reveals tenderness of the right lower anterior tibia. X-ray of the right lower extremity reveals a small tibial stress fracture. When the findings are explained and treatment with analgesics and limited physical activity is discussed, the patient becomes distressed that he has to stop running. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 5 of 37
5. Question
A newborn boy is brought to the emergency department for coughing and difficulty feeding. The patient was born at home 3 hours ago via spontaneous vaginal delivery. When the mother, a 24-year-old primigravida, attempted to breastfeed him, the patient coughed and vomited. The mother had no prenatal care. She has a history of recreational drug use but says she did not use any substances during the pregnancy. Temperature is 37 C (98.6 F), pulse is 120/min, and respirations are 50/min. Oxygen saturation is 95%. Ballard score estimates the boy was born at 37 weeks gestation. Weight and length are at the 25th and 50th percentiles for age, respectively. After attempting another feed with 10 mL of formula, the patient has a coughing fit; there is formula mixed with saliva in his mouth. Coarse breath sounds are noted bilaterally on pulmonary examination with intercostal retractions. Cardiac examination reveals a grade 2/6 systolic murmur at the upper left sternal border. There is no hepatomegaly. Neurologic examination shows normal tone. Which of the following is the best next step in the management of this patient?
CorrectIncorrect -
Question 6 of 37
6. Question
A 55-year-old woman undergoes allogeneic hematopoietic stem cell transplantation from an HLA-matched, unrelated donor for treatment of acute myeloid leukemia. She received conditioning chemotherapy prior to the transplantation, and her immediate post-transplant course was uncomplicated. However, 3 weeks after the transplant, the patient develops worsening crampy abdominal pain and diarrhea. The diarrhea is watery and persistent, even at night, with output up to 3 liters daily. No particular food makes the symptoms better or worse. Medications include tacrolimus, prophylactic acyclovir, trimethoprim-sulfamethoxazole, and voriconazole. The patient has no other chronic medical conditions. She has been in the hospital since the transplantation and is on a low-microbial diet. Physical examination shows generalized maculopapular rash. Stool testing for Clostridioides (formerly Clostridium) difficile and PCR testing for cytomegalovirus are negative. Which of the following is the most likely cause of this patient’s diarrhea?
CorrectIncorrect -
Question 7 of 37
7. Question
A 78-year-old woman is brought from the nursing home to the emergency department due to worsening abdominal distension. Over the past 3 days, the patient has had decreased appetite and progressive abdominal distension that is now accompanied by diffuse abdominal discomfort. Her last bowel movement was 4 days ago. Medical history is significant for dementia, hypertension, osteoarthritis, osteoporosis, and chronic constipation. Surgical history includes open appendectomy and open cholecystectomy. Temperature is 37 C (98.6 F), blood pressure is 138/80 mm Hg, and pulse is 92/min. Physical examination shows a distended and tympanitic abdomen with diffuse tenderness to palpation but no rigidity or rebound tenderness. Blood counts and serum electrolytes are within normal limits. Abdominal x-ray is shown in the exhibit. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 8 of 37
8. Question
A 34-year-old woman comes to the office due to sudden onset epigastric pain radiating to the back, nausea, and vomiting. Her medical history is significant for major depression, generalized anxiety, and irregular menses. She takes sertraline and an oral contraceptive. The patient describes occasional heavy alcohol use and drinks hard liquor daily. She does not use tobacco or illicit drugs. Temperature is 37 C (98.6 F), blood pressure is 120/80 mm Hg, pulse is 98/min, and respirations are 18/min. BMI is 24 kg/m2. No jaundice is present. Examination shows epigastric tenderness. Serum lipase levels are markedly elevated. Abdominal ultrasonogram reveals an enlarged pancreas, no gallstones, and normal gallbladder; a mass is also noted in the right lobe of the liver. Subsequent abdominal CT scan reveals a well-circumscribed, 5-cm mass with a central scar that appears hypodense on noncontrast imaging. Imaging with contrast indicates the lesion is hyperdense. The rest of the liver appears to be normal, and there is no intra- or extrahepatic duct dilatation. Which of the following is the most likely diagnosis for the liver lesion?
CorrectIncorrect -
Question 9 of 37
9. Question
A 30-year-old woman comes to the office due to increasing muscle weakness. The patient has not been able to grip her coffee mug or open jars due to weakness in her hands. She has also had some loss of sensation in the upper extremities that has caused her to cut herself while doing craft projects. The patient was in a motor vehicle collision 7 years ago in which she sustained a whiplash cervical spine injury. She has no other medical conditions. BMI is 22 kg/m2. Physical examination reveals moderate wasting of the small muscles of the hand. Bilateral upper extremities have impaired pain and temperature sensation. Light touch, vibration, and position senses are all intact. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 10 of 37
10. Question
A 56-year-old woman comes to the office for evaluation of a leg ulcer. The patient bumped her left leg on a chair 2 weeks ago and noticed painful papules at the injury site several days later. The lesions rapidly enlarged and opened, causing worsening pain and drainage. The ulcer progressively enlarged despite the use of topical antiseptics. The patient has a history of rheumatoid arthritis and does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 130/78 mm Hg, and pulse is 86/min. Physical examination shows a tender ulcer on the lower left extremity, as shown in the exhibit. There are no other lesions. Which of the following is the most likely cause of this patient’s skin condition?
 CorrectIncorrect
CorrectIncorrect -
Question 11 of 37
11. Question
A 63-year-old man comes to the emergency department due to left leg pain. The patient typically has pain in both legs after walking a couple of blocks, but several hours ago, severe left leg pain suddenly developed while he was resting. He reports numbness in the left leg, and he is also experiencing intermittent palpitations. Medical history includes hypertension and hyperlipidemia. The patient has smoked a pack of cigarettes daily for 45 years. Blood pressure is 130/80 mm Hg, and pulse is 116/min and irregular. On examination, hair is sparse on both legs. Distal pulses are absent on the left and diminished on the right. Sensation to light touch is decreased on the dorsum of the left foot and leg, and ankle dorsiflexion is weaker on the left. Which of the following is the best first step in management of this patient?
CorrectIncorrect -
Question 12 of 37
12. Question
A 65-year-old man comes to the office due to 4 weeks of persistent epigastric pain and nausea. The pain is constant and does not improve or worsen with activities, position, or diet. The patient lost approximately 4.5 kg (9.9 lb) over this period. He has no fever, vomiting, constipation, or diarrhea. He was diagnosed with type 2 diabetes mellitus 6 months ago, which is controlled with a low-carbohydrate diet. The patient has never had surgery and has no other chronic medical conditions. He has a 45-pack-year history of smoking. He does not use alcohol or illicit drugs. Temperature is 36.5 C (97.7 F), blood pressure is 122/72 mm Hg, pulse is 68/min, and respirations are 16/min. BMI is 24 kg/m2. Mucous membranes are moist. No lymphadenopathy is present in the cervical or axillary chains. Bowel sounds are present, and the abdomen is soft with mild epigastric tenderness to deep palpation. No hepatosplenomegaly or shifting dullness is present. The remainder of the examination is normal. Complete blood count, serum chemistry, and liver function studies is all normal except a fasting blood sugar of 130 mg/dL. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 13 of 37
13. Question
A 67-year-old man comes to the office due to 2 days of back pain. The patient was moving boxes in his garage when the pain started. It is not relieved by lying down and increases in intensity when he strains or coughs. The patient cannot sleep due to pain and has taken acetaminophen several times without relief. He has never before had such pain. Physical examination shows 2+ symmetric knee and ankle jerk reflexes. Straight-leg raising test is negative. There is point tenderness to palpation and percussion along the midline at the fourth lumbar vertebra. Which of the following is the most likely underlying etiology of this patient’s current condition?
CorrectIncorrect -
Question 14 of 37
14. Question
A 67-year-old man comes to the emergency department due to abdominal discomfort and distension. Five days ago, he began having large-volume watery stools 6-8 times daily after eating at a new restaurant. He also has had associated mild abdominal cramps and nausea but no fever, chills, vomiting, or bloody stools. His wife, who had the same food, also experienced similar symptoms. He self-treated with increased oral fluids and the stool frequency and consistency began to improve. However, his bowel movements abruptly stopped yesterday, and the diffuse abdominal discomfort and distension worsened. Medical history includes hypertension, coronary artery disease, and heart failure treated with diuretics. Temperature is 37 C (98.6 F), blood pressure is 116/72 mm Hg, and pulse is 102/min. Physical examination shows dry mucous membranes. The abdomen is distended, tympanic, and mildly tender to palpation with no guarding or rebound tenderness. Bowel sounds are decreased. Digital rectal examination reveals an empty rectal vault with no evidence of blood or melena. Abdominal CT scan shows diffuse colonic dilation with nondilated small bowels. Leukocyte count is normal and testing for Clostridioides (formerly Clostridium) difficile is negative. Which of the following most likely contributed to this patient’s current condition?
CorrectIncorrect -
Question 15 of 37
15. Question
A 62-year-old man returns to the emergency department due to urinary retention. Two days ago, the patient was moving furniture when he suddenly had sharp, shooting pain in the lower back and right leg. He came to the emergency department yesterday after his pain had not improved with naproxen. No work-up was indicated, and the patient was discharged with a short course of acetaminophen-hydrocodone. He took the medication and rested. When the patient woke up today, he had to strain to urinate. He has no chronic medical conditions. Vital signs are within normal limits. Examination of the right lower extremity shows that plantar flexion is impaired, sensation is reduced on the posterior aspect of the leg and the lateral edge of the foot, and the ankle reflex is absent. The straight-leg raising test markedly increases pain in the right posterior thigh and leg. Perianal sensation is decreased. The remainder of the neurologic examination is normal. What is the most likely cause of this patient’s urinary retention?
CorrectIncorrect -
Question 16 of 37
16. Question
A 25-year-old man comes to the office due to decreased force of the urinary stream and incomplete emptying of the bladder. He has no urgency, frequency, nocturia, dysuria, or fever. Bowel movements are regular. The patient has no chronic medical conditions and takes no medications. Vital signs are within normal limits. The abdomen is soft and nontender. External genitalia are normal; no penile discharge is noted. No inguinal lymphadenopathy is present. Neurologic examination shows no abnormalities. Urinalysis is normal. Postvoid residual volume is high. What is the most likely cause of this patient’s current condition?
CorrectIncorrect -
Question 17 of 37
17. Question
A 65-year-old man is evaluated in the hospital for acute-onset shortness of breath. The patient was originally admitted 5 days ago for peritonitis due to a perforated peptic ulcer, for which he underwent surgical repair. A large-bore, right internal jugular venous catheter was placed during the operation. Today, he was out of bed, sitting in a chair, and comfortable on room air. The internal jugular catheter was removed. Minutes after catheter removal, the patient develops acute-onset shortness of breath and cough. On examination, he appears in respiratory distress. Blood pressure is 110/60 mm Hg, pulse is 110/min, and respirations are 25/min. Oxygen saturation is 85% on room air. The jugular veins are distended. Breath sounds are normal and equal on both sides. In addition to high-flow oxygen supplementation, the patient should be immediately placed in which of the following positions?
CorrectIncorrect -
Question 18 of 37
18. Question
An 18-year-old man is brought to the emergency department after falling and striking his chest. He had been playing an interactive video game when he lost his balance and hit his left chest against the coffee table. The patient now has moderate left-sided chest pain, worse with deep inspiration. He also feels lightheaded. On examination, the patient appears uncomfortable and is taking shallow breaths. Blood pressure is 88/50 mm Hg, pulse is 122/min, and respirations are 28/min. Jugular veins are flat. The trachea is midline. The left chest wall has intact, bruised skin and is exquisitely tender to palpation. Breath sounds are present on the right but diminished in the left lung base, which is dull to percussion. Heart sounds are normal without murmurs. The abdomen is soft, nondistended, and nontender. Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 19 of 37
19. Question
A 62-year-old man is hospitalized for elective coronary artery bypass graft surgery. The patient had been having worsening exertional angina and was found to have 3-vessel coronary artery disease. His other medical conditions include hypertension, type 2 diabetes mellitus, and hyperlipidemia. He has had no infections and has not used antibiotics recently. The patient has a history of severe penicillin allergy causing anaphylactic shock. Blood pressure is 128/72 mm Hg and pulse is 78/min. The lungs are clear on auscultation and heart sounds are normal. Preoperative blood cell counts, serum chemistry, and coagulation studies are within normal limits. Which of the following is the most appropriate preoperative prophylactic antibiotic for this patient?
CorrectIncorrect -
Question 20 of 37
20. Question
A 35-year-old man comes to the office for follow-up of an abnormal chest x-ray finding. The patient went to the emergency department 2 weeks ago after a chest injury; during a softball game, he was struck in the chest by a ball thrown from a distance of 4 feet. Initial evaluation showed no significant trauma or rib fracture, but the chest x-ray revealed an air/fluid level posterior to the cardiac silhouette consistent with a sliding hiatal hernia. The patient feels well and has had no heartburn, regurgitation, difficulty swallowing, or abdominal discomfort. He has no other medical conditions and takes no medications. The patient does not use tobacco, alcohol, or illicit drugs. Vital signs are within normal limits. Physical examination shows no abnormalities. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 21 of 37
21. Question
A 47-year-old man is brought to the emergency department due to a fall down a flight of stairs. The patient was inebriated and missed a step. He did not lose consciousness but had neck and shoulder pain afterward. The patient also reports numbness and weakness of the left upper extremity. He has no prior medical conditions and takes no medications. Temperature is 37 C (98.6 F), blood pressure is 144/88 mm Hg, and pulse is 94/min. Physical examination reveals neck tenderness. There is mild, left-sided weakness of elbow extension and wrist flexion, with decreased pain sensation of the index and middle fingers. Lower extremity muscle strength and sensation are intact. Plantar reflex is down going bilaterally. CT scan of the cervical spine is shown in the exhibit. Which of the following is the most likely diagnosis?
 CorrectIncorrect
CorrectIncorrect -
Question 22 of 37
22. Question
A 26-year-old man comes to the office for follow-up related to painless progressive visual loss in the right eye. Recent ophthalmological evaluation revealed macular edema due to 2 retinal lesions consistent with capillary hemangioblastoma. He underwent laser photocoagulation treatment, and the vision in his right eye has improved. The patient has no other medical conditions. His father died from a cerebral hemorrhage at age 52. MRI of the brain with gadolinium reveals 2 small, cystic, enhancing nodules in the cerebellum. Renal ultrasonography reveals multiple cysts in both kidneys. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 23 of 37
23. Question
A 50-year-old man comes to the emergency department due to 2 days of malaise, decreased appetite, abdominal discomfort, and bloody stools. The patient had end-stage renal disease and underwent kidney transplantation 4 months ago. He had no major postoperative issues and currently takes mycophenolate, tacrolimus, and prednisone. The patient has a 15 pack-year smoking history but quit several years ago. Temperature is 37 C (98.6 F), blood pressure is 110/70 mm Hg, pulse is 104/min, and respirations are 22/min. Physical examination shows mild abdominal tenderness in the left lower quadrant. Rectal examination is normal. Stool is guaiac positive. Laboratory results are as follows:
Complete blood count
Hemoglobin
8.1 g/dL
Platelets
190,000/mm3
Leukocytes
3,800/mm3
Serum chemistry
Creatinine
1.2 mg/dL
Atypical lymphocytes are seen on peripheral blood smear. A colonoscopy reveals multiple ulcerations throughout the colon. Which of the following is the most likely diagnosis for this patient?
CorrectIncorrect -
Question 24 of 37
24. Question
Two days after undergoing a laparoscopic partial colectomy to resect a large adenoma, a 45-year-old woman becomes acutely agitated. She has been anxious and uncooperative since the surgery, but, today, she is repeatedly getting out of bed, shouting “Get your hands off me! God is watching!” when the nurses try to redirect her. The patient was given a preoperative dose of intravenous cefoxitin and is receiving IV ketorolac and acetaminophen as needed for pain. Medical history includes polysubstance use and schizoaffective disorder. Chart review shows that she has been prescribed sertraline and a long-acting injection of aripiprazole, but she is unable to provide information about when she had her last dose of either. Temperature is 39 C (102.2 F), blood pressure is 160/90 mm Hg, pulse is 102/min, and respirations are 18/min. The patient is diaphoretic and oriented only to person. Physical examination shows well-healing incision sites with no erythema; the remainder of the examination is limited due to agitation. Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 25 of 37
25. Question
A 34-year-old woman comes to the office due to difficulty hearing, especially in the left ear. The hearing loss has worsened over the past year, and she is now having trouble hearing people at work; however, when the environment is noisy, she can understand speech better than when she is in a quiet room. The patient also hears ringing in the left ear. She has no dizziness, vertigo, or ear pain. She has had no significant noise exposure. The patient has no other medical conditions and takes no medications. Her mother had surgery for hearing loss when she was in her 40s. On examination, the tympanic membranes are clear with a good light reflex, good landmarks, and no middle ear effusion. There is a slight reddish hue behind the left tympanic membrane. Which of the following is the most likely mechanism of this patient’s condition?
CorrectIncorrect -
Question 26 of 37
26. Question
A 21-year-old woman comes to the office for evaluation of progressively increasing dyspnea and nonproductive cough for the past 2 weeks. Four months ago, the patient underwent bilateral lung transplantation for bronchiectasis due to underlying cystic fibrosis. Other medical conditions include pancreatic insufficiency and osteoporosis. Current medications are pancreatic enzymes, multivitamins, tacrolimus, mycophenolate mofetil, and prednisone. Temperature is 38 C (100.4 F), blood pressure is 110/78 mm Hg, pulse is 96/min, and respirations are 18/min. Pulse oximetry shows 98% with the patient using 2 liters/min of supplemental oxygen. Examination shows bilateral lung crackles. Chest x-ray reveals perihilar opacities, interstitial edema, and small bilateral pleural effusions. What is the most appropriate next step in management?
CorrectIncorrect -
Question 27 of 37
27. Question
A 30-year-old man is brought to the emergency department due to a worsening headache. The patient has had episodic right-sided headaches over the past 6 months. Thirty minutes ago, he began experiencing a right temporal headache while at rest, which gradually worsened to severe pain over the next several minutes. He also had nausea and an episode of vomiting. The patient is now somnolent and difficult to rouse. He has no other medical conditions and had a normal medical evaluation a year ago for military enlistment. Temperature is 37 C (98.6 F), blood pressure is 150/90 mm Hg, pulse is 64/min, and respirations are 14/min. The patient withdraws all extremities to painful stimuli, but left-sided deep tendon reflexes are increased. There is no neck rigidity. Which of the following is the most likely underlying cause of this patient’s current condition?
CorrectIncorrect -
Question 28 of 37
28. Question
A 32-year-old woman, gravida 1 para 1, is evaluated on the postpartum floor due to fluid leakage from her incision. Two days ago, the patient underwent a cesarean delivery after failed induction of labor and intraamniotic infection. She had her incision bandage removed this morning with minimal clear fluid on the bandage. The patient then walked to the nursery, where she noticed that serosanguineous fluid had stained her hospital gown. Fluid has continued to drain from her abdominal incision. Temperature is 37.2 C (99 F). BMI is 35 kg/m2. The uterus is palpable below the umbilicus and has no fundal tenderness. The Pfannenstiel incision has a 4-cm defect at the right corner that is draining scant serosanguineous fluid. There is no surrounding erythema or induration. The subcutaneous tissue has no areas of necrosis or crepitus, and the rectus fascia is intact. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 29 of 37
29. Question
A 56-year-old man with a recent diagnosis of cirrhosis comes to the hospital for elective upper gastrointestinal endoscopy to evaluate for esophageal varices. The patient has elevated liver aminotransferase levels, and a hepatitis serology was positive for chronic hepatitis C. Abdominal imaging studies revealed mild ascites, a nodular-appearing liver, and splenomegaly. He has no other medical problems. The patient has a remote history of injection drug use and does not use tobacco or alcohol. Vital signs are within normal limits. Benzocaine throat spray is used for topical anesthesia, and procedural sedation is obtained with midazolam and fentanyl. During the procedure, the patient’s oxygen saturation by pulse oximetry gradually decreases to 85% on ambient air and does not improve with application of supplemental oxygen via face mask. Physical examination demonstrates bluish discoloration of the lips and fingertips. Lung fields are clear to auscultation, and heart sounds are normal. Results of urgent laboratory tests are as follows:
Hematocrit
39%
Arterial blood gases
pH
7.39
PaO2
142 mm Hg
PaCO2
34 mm Hg
Oxygen saturation
99%
Which of the following is the most likely cause of this patient’s decrease in oxygen saturation?
CorrectIncorrect -
Question 30 of 37
30. Question
A 25-year-old man is brought to the emergency department due to a stab wound to the chest. The patient was returning to his parked car when he was mugged. He tried to resist, but the assailant stabbed him once in the left chest with a switchblade. During transport, the patient became unresponsive and required intubation. He also received 2 L of normal saline. Upon arrival, blood pressure is 80/42 mm Hg and pulse is 132/min. Pulse oximetry is 98% on 60% oxygen. Weight is 80 kg (176.4 lb) and height is 177.5 cm (5 ft 9 in). On physical examination, there is a fist-sized blood stain on the patient’s shirt and a 3-cm linear wound in the left fifth intercostal space at the midaxillary line, with dried blood and no active external hemorrhage. Breath sounds are diminished in the left lung and normal in the right lung. Heart sounds are normal. The jugular veins are flat. The abdomen is nondistended and soft to palpation. Focused assessment with sonography for trauma (FAST) reveals left-sided intrathoracic free fluid. A left-sided chest tube is placed with immediate output of 2,000 mL of blood. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 31 of 37
31. Question
A 76-year-old man with multi-infarct dementia comes to the emergency department due to cough and low-grade fever. He was treated for pneumonia twice in the last year. For the past 6 months, he has had difficulty swallowing and has occasionally regurgitated undigested food. The patient has a lengthy history of hypertension and chronic atrial fibrillation. BMI is 22 kg/m2. Temperature is 38.5 C (101.3 F), blood pressure is 150/95 mm Hg, pulse is 102/min, and respirations are 16/min. Physical examination is notable for foul-smelling breath and a fluctuant mass in the left neck. Auscultation shows crackles in the right lung base. Chest x-ray shows an infiltrate without cavitation in the right lower lung field. The patient is admitted to the hospital, sputum and blood cultures are sent to the laboratory, and antibiotics are started. A few days later, the patient’s condition is markedly improved. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 32 of 37
32. Question
A 47-year-old woman comes to the office due to knee pain. The patient slipped on an icy step 2 weeks ago and fell on her knee. Since that time, she has had severe knee pain and a large overlying bruise, which has failed to heal. The patient underwent a Roux-en-Y gastric bypass 6 months ago for morbid obesity and has lost 20 kg (44.1 lb) since then. She does not use tobacco or alcohol. Vital signs are normal. On examination, a large ecchymosis is present over the left knee. The knee is swollen, painful to palpation, and has a limited range of motion. There are several smaller ecchymoses and petechiae located on all four extremities. Laboratory results are as follows:
Complete blood count
Hemoglobin
11.4 g/dL
Platelets
375,000/mm3
Leukocytes
6,200/mm3
Serum chemistry
Creatinine
0.8 mg/dL
Liver function studies
Albumin
2.9 g/dL
Total bilirubin
0.6 mg/dL
Aspartate aminotransferase (SGOT)
22 U/L
Alanine aminotransferase (SGPT)
14 U/L
Coagulation studies
Prothrombin time
12 sec
International Normalized Ratio (INR)
1.1 (normal: 0.8-1.2)
Activated partial thromboplastin time
31 sec
Left knee x-ray reveals a large effusion but no fracture. Arthrocentesis yields brown fluid positive for xanthochromia. Which of the following best explains this patient’s manifestations?
CorrectIncorrect -
Question 33 of 37
33. Question
A 23-year-old man is brought to the emergency department by his family due to a severe sore throat, persistent elevated fevers, pain and difficulty with swallowing, and shortness of breath. His symptoms worsened over the past day. Three days ago, he was seen at an urgent care center for pharyngitis and was prescribed azithromycin. The patient’s past medical history is otherwise insignificant. He does not use tobacco, alcohol, or illicit drugs. His temperature is 40 C (104 F), blood pressure is 90/58 mm Hg, pulse is 115/min, and respirations are 24/min. Pulse oximetry shows 94% on room air. Physical examination is notable for a well-built man in moderate distress due to pain. There is mild swelling and erythema of the oropharynx and tonsils without exudate. Dentition is intact and shows good hygiene. The neck is swollen and tender along the left sternocleidomastoid muscle. Lung examination reveals basilar crackles. There are no heart murmurs. Leukocyte count is 17,400/mm3 with 93% neutrophils. A duplex ultrasound shows left internal jugular vein thrombosis. Chest x-ray reveals multiple peripheral lung nodules, some with cavitation. Which of the following is the most likely causative organism?
CorrectIncorrect -
Question 34 of 37
34. Question
A 40-year-old man is brought to the emergency department after a motor vehicle collision. Blood pressure is 130/84 mm Hg and pulse is 102/min. Heart and lung sounds are normal. Abdominal palpation shows fullness and tenderness in the suprapubic region. There is no blood at the urethral meatus, and digital rectal examination reveals a normal prostate. Chest x-ray is normal. Focused Assessment with Sonography for Trauma reveals no intraperitoneal free fluid. Pelvic x-ray reveals fracture of the left pubic ramus. A Foley catheter is placed without resistance, with immediate return of bloody urine. Emergency CT scan of the abdomen and pelvis is performed. Which of the following injuries is most likely to be seen on CT scan in this patient?
CorrectIncorrect -
Question 35 of 37
35. Question
A 27-year-old man is brought to the emergency department after a high-speed motor vehicle collision. On arrival, his blood pressure is 90/52 mm Hg, pulse is 122/min, and respirations are 30/min. The patient is in moderate respiratory distress. There are bruises on the anterior chest wall and abdomen. No breath sounds are heard in the left lung, and initial chest x-ray shows hemopneumothorax. Fluid resuscitation is given, left-sided chest tubes and a nasogastric tube are placed, and the patient is admitted to the trauma floor after stabilization. Four days later, the chest tubes continue to drain appropriate serosanguinous fluid, but the patient still feels short of breath. He has an occasional dry, nonproductive cough. Current temperature is 36.8 C (98.2 F), blood pressure is 118/78 mm Hg, pulse is 88/min, and respirations are 20/min. A repeat chest x-ray shows the following.
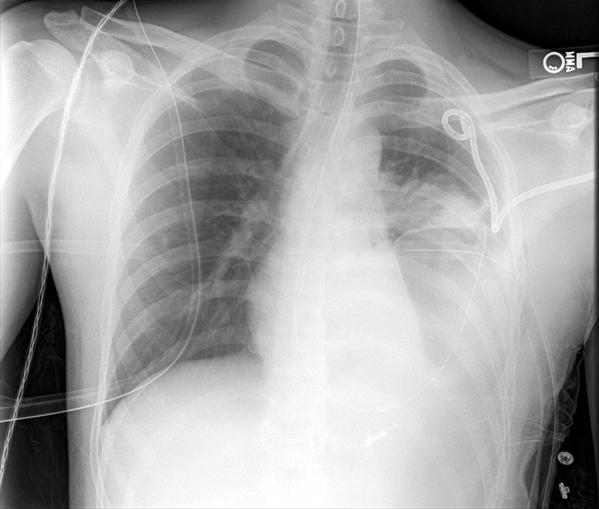
Which of the following is the most likely cause of the patient’s continued respiratory distress?
CorrectIncorrect -
Question 36 of 37
36. Question
A 17-year-old girl is brought to the emergency department due to severe right shoulder pain. She was playing basketball when her shoulder popped out of place. Her coach placed her arm in a sling, gave her an ice pack, and drove her to the emergency department. The patient has no numbness or tingling in the arm. She takes no medications. Vital signs are normal. On examination, the range of motion in the right shoulder is limited, with anterior and lateral tenderness to palpation. The neurovascular examination is normal. X-ray of the right shoulder is shown in the exhibit. The condition is treated successfully without complications. This patient is at greatest risk for which of the following conditions?
 CorrectIncorrect
CorrectIncorrect -
Question 37 of 37
37. Question
A 72-year-old man comes to the office due to fatigue and lower extremity swelling for the last several weeks. He also has a feeling of pulsation in his neck when he lies down. He has no chest pain. The patient takes lisinopril and amlodipine for hypertension. He underwent permanent pacemaker implantation for sick sinus syndrome 6 months ago. He is a lifetime nonsmoker. The patient has no family history of cardiovascular disease. Blood pressure is 112/70 mm Hg and pulse is 79/min and regular. The jugular veins are distended with the patient in the sitting position. A 3/6 holosystolic murmur is heard over the left lower sternal border. The lungs are clear on auscultation. The liver is enlarged and mildly tender on palpation. Bilateral 3+ edema is present in the lower extremities. Which of the following is the most likely diagnosis?
CorrectIncorrect
